An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Breech presentation.
Caron J. Gray ; Meaghan M. Shanahan .
Affiliations
Last Update: November 6, 2022 .
- Continuing Education Activity
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation are frank, complete, and incomplete. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. This activity reviews the cause and pathophysiology of breech presentation and highlights the role of the interprofessional team in its management.
- Determine the pathophysiology of breech presentation.
- Apply the physical exam of a patient with a breech presentation.
- Differentiate the treatment options for breech presentation.
- Communicate the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by breech presentation.
- Introduction
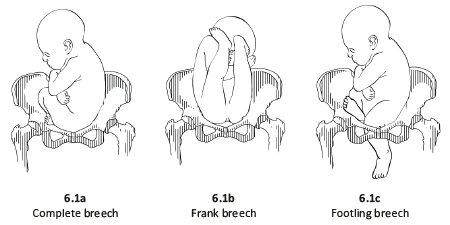
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The 3 types of breech presentation are frank, complete, and incomplete. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of 1 or both hips extended, also known as footling (one leg extended) or double footling breech (both legs extended). [1] [2] [3]
Clinical conditions associated with breech presentation may increase or decrease fetal motility or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
- Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 25% are breech at 28 weeks or less.
Specifically, following 1 breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Some have also described prior cesarean delivery as increasing the incidence of breech presentation twofold.
- Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in breech presentation affect fetal motility or the vertical polarity of the uterine cavity. [6] [7] Conditions that change the vertical polarity or the uterine cavity or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta occupies the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Larger myomas are mainly located in the lower uterine segment, often intramural or submucosal, and prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: The fetus is often in an unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to the vertex due to lack of fluid
- Laxity of the maternal abdominal wall: The Uterus falls forward, and the fetus cannot engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
- History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex. Any of these findings should raise suspicion, and an ultrasound should be performed.
An abdominal exam using the Leopold maneuvers in combination with the cervical exam can diagnose a breech presentation. Ultrasound should confirm the diagnosis. The fetal lie and presenting part should be visualized and documented on ultrasound. If a breech presentation is diagnosed, specific information, including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously), should be documented.
- Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000, compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, the 2 groups had no significant difference in maternal morbidity or mortality. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at 2 years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11]
Since the TBT, many authors have argued that there are still some specific situations in that vaginal breech delivery is a potential, safe alternative to a planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by 1 report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering an external cephalic version (ECV) to those patients who meet the criteria, and for those who are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age determines the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide the mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note is that no prospective clinical trials examine this issue due to a lack of recruitment.
- Differential Diagnosis
The differential diagnoses for the breech presentation include the following:
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
- Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
- Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor, delivery nurse, anesthesiologist, and neonatologist. The ultimate decision rests on the obstetrician. To prevent complications, today, cesarean sections are performed, and experience with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
- Review Questions
- Access free multiple choice questions on this topic.
- Click here for a simplified version.
- Comment on this article.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gray CJ, Shanahan MM. Breech Presentation. [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Breech Presentation - StatPearls Breech Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
6.1 Breech presentation
Presentation of the feet or buttocks of the foetus.
6.1.1 The different breech presentations
- In a complete breech presentation, the legs are tucked, and the foetus is in a crouching position (Figure 6.1a).
- In a frank breech presentation, the legs are extended, raised in front of the torso, with the feet near the head (Figure 6.1b).
- In a footling breech presentation (rare), one or both feet present first, with the buttocks higher up and the lower limbs extended or half-bent (Figure 6.1c).
6.1.2 Diagnosis
- The cephalic pole is palpable in the uterine fundus; round, hard, and mobile; the indentation of the neck can be felt.
- The inferior pole is voluminous, irregular, less hard, and less mobile than the head.
- During labour, vaginal examination reveals a “soft mass” divided by the cleft between the buttocks, with a hard projection at end of the cleft (the coccyx and sacrum).
- After rupture of the membranes: the anus can be felt in the middle of the cleft; a foot may also be felt.
- The clinical diagnosis may be difficult: a hand may be mistaken for a foot, a face for a breech.
6.1.3 Management
Route of delivery.
Before labour, external version (Chapter 7, Section 7.7 ) may be attempted to avoid breech delivery.
If external version is contra-indicated or unsuccessful, the breech position alone – in the absence of any other anomaly – is not, strictly speaking, a dystocic presentation, and does not automatically require a caesarean section. Deliver vaginally, if possible – even if the woman is primiparous.
Breech deliveries must be done in a CEmONC facility, especially for primiparous women.
Favourable factors for vaginal delivery are:
- Frank breech presentation;
- A history of vaginal delivery (whatever the presentation);
- Normally progressing dilation during labour.
The footling breech presentation is a very unfavourable position for vaginal delivery (risk of foot or cord prolapse). In this situation, the route of delivery depends on the number of previous births, the state of the membranes and how far advanced the labour is.
During labour
- Monitor dilation every 2 to 4 hours.
- If contractions are of good quality, dilation is progressing, and the foetal heart rate is regular, an expectant approach is best. Do not rupture the membranes unless dilation stops.
- If the uterine contractions are inadequate, labour can be actively managed with oxytocin.
Note : if the dilation stales, transfer the mother to a CEmONC facility unless already done, to ensure access to surgical facility for potential caesarean section.
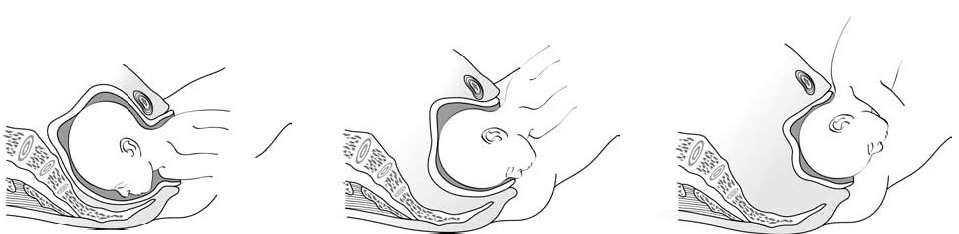
At delivery
- Insert an IV line before expulsion starts.
- Consider episiotomy at expulsion. Episiotomy is performed when the perineum is sufficiently distended by the foetus's buttocks.
- Presence of meconium or meconium-stained amniotic fluid is common during breech delivery and is not necessarily a sign of foetal distress.
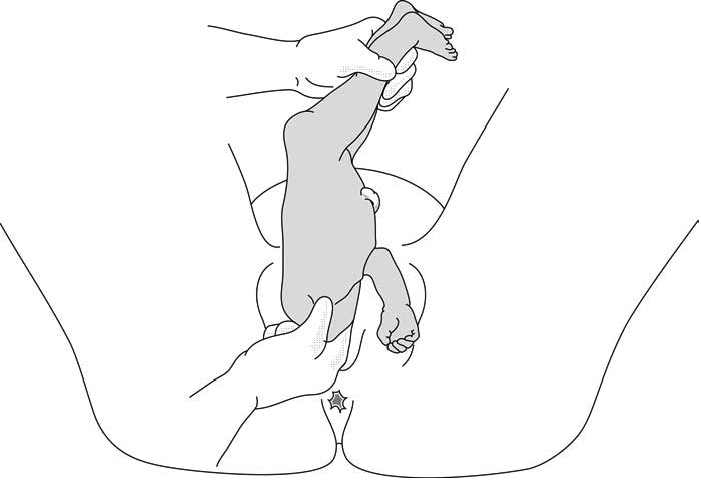
- The infant delivers unaided , as a result of the mother's pushing, simply supported by the birth attendant who gently holds the infant by the bony parts (hips and sacrum), with no traction. Do not pull on the legs.
Once the umbilicus is out, the rest of the delivery must be completed within 3 minutes, otherwise compression of the cord will deprive the infant of oxygen. Do not touch the infant until the shoulder blades appear to avoid triggering the respiratory reflex before the head is delivered.
- Monitor the position of the infant's back; impede rotation into posterior position.
Figures 6.2 - Breech delivery
6.1.4 Breech delivery problems
Posterior orientation.
If the infant’s back is posterior during expulsion, take hold of the hips and turn into an anterior position (this is a rare occurrence).
Obstructed shoulders
The shoulders can become stuck and hold back the infant's upper chest and head. This can occur when the arms are raised as the shoulders pass through the mother's pelvis. There are 2 methods for lowering the arms so that the shoulders can descend:
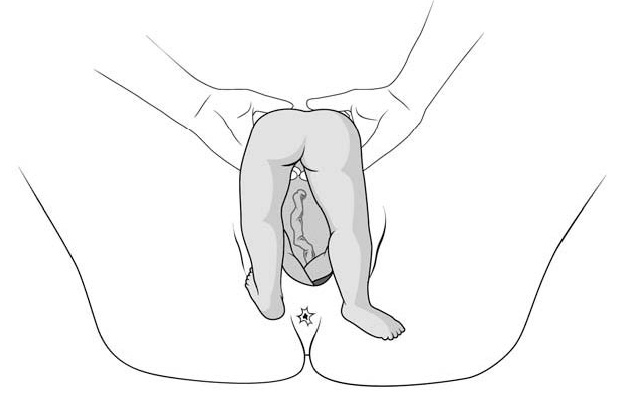
1 - Lovset's manoeuvre
- With thumbs on the infant's sacrum, take hold of the hips and pelvis with the other fingers.
- Turn the infant 90° (back to the left or to the right), to bring the anterior shoulder underneath the symphysis and engage the arm. Deliver the anterior arm.
- Then do a 180° counter-rotation (back to the right or to the left); this engages the posterior arm, which is then delivered.
Figures 6.3 - Lovset's manoeuvre

6.3c - Delivering the anterior arm and shoulder
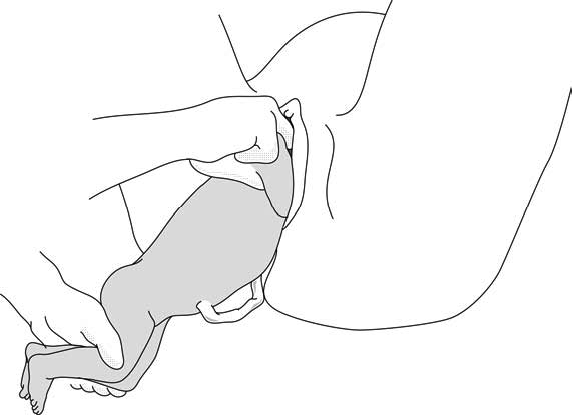
2 - Suzor’s manoeuvre
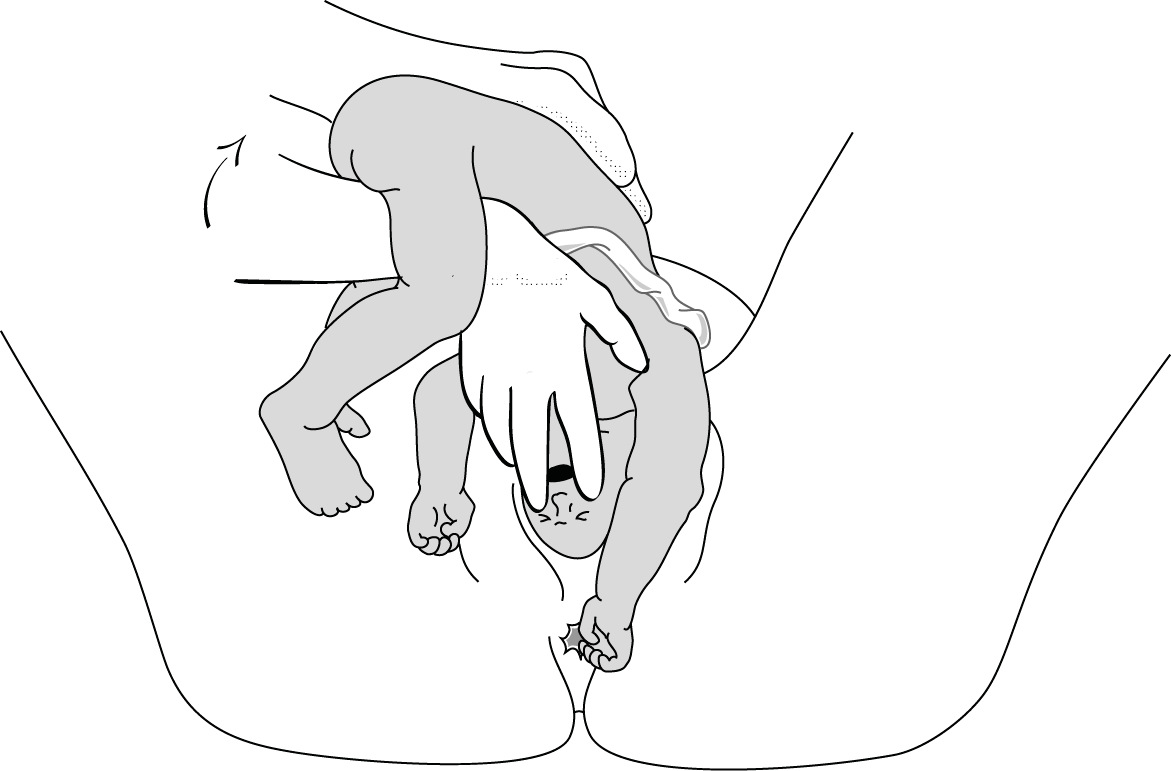
In case the previous method fails:
- Turn the infant 90° (its back to the right or to the left).
- Pull the infant downward: insert one hand along the back to look for the anterior arm. With the operator thumb in the infant armpit and middle finger along the arm, bring down the arm (Figure 6.4a).
- Lift infant upward by the feet in order to deliver the posterior shoulder (Figure 6.4b).
Figures 6.4 - Suzor's manoeuvre
6.4b - Delivering the posterior shoulder
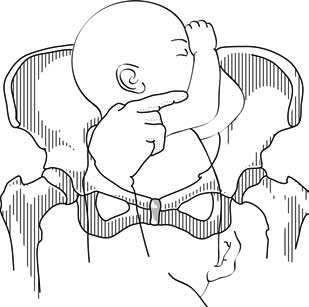
Head entrapment
The infant's head is bulkier than the body, and can get trapped in the mother's pelvis or soft tissue.
There are various manoeuvres for delivering the head by flexing it, so that it descends properly, and then pivoting it up and around the mother's symphysis. These manoeuvres must be done without delay, since the infant must be allowed to breathe as soon as possible. All these manoeuvres must be performed smoothly, without traction on the infant.
1 - Bracht's manoeuvre
- After the arms are delivered, the infant is grasped by the hips and lifted with two hands toward the mother's stomach, without any traction, the neck pivoting around the symphysis.
- Having an assistant apply suprapubic pressure facilitates delivery of the aftercoming head.
2 - Modified Mauriceau manoeuvre
- Infant's head occiput anterior.
- Kneel to get a good traction angle: 45° downward.
- Support the infant on the hand and forearm, then insert the index and middle fingers, placing them on the infant’s maxilla. Placing the index and middle fingers into the infant’s mouth is not recommended, as this can fracture the mandible.
- Place the index and middle fingers of the other hand on either side of the infant's neck and lower the infant's head to bring the sub-occiput under the symphysis (Figure 6.6a).
- Tip the infant’s head and with a sweeping motion bring the back up toward the mother's abdomen, pivoting the occiput around her symphysis pubis (Figure 6.6b).
- Suprapubic pressure on the infant's head along the pelvic axis helps delivery of the head.
- As a last resort, symphysiotomy (Chapter 5, Section 5.7 ) can be combined with this manoeuvre.
Figures 6.6 - Modified Mauriceau manoeuvre
6.6a - Step 1 Infant straddles the birth attendant's forearm; the head, occiput anterior, is lowered to bring the occiput in contact with the symphysis.

6.6b - Step 2 The infant's back is tipped up toward the mother's abdomen.
3 - Forceps on aftercoming head
This procedure can only be performed by an operator experienced in using forceps.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.

Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Pregnancy and Postpartum
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Original Author(s): Alice Reid and Chloe Webster Last updated: 4th December 2024 Revisions: 25
- 1 Types of Breech Presentation
- 2 Aetiology and Risk Factors
- 3 Clinical Features
- 4 Differential Diagnosis
- 5 Investigations
- 6.1 External Cephalic Version
- 6.2 Caesarean Section
- 6.3 Vaginal Breech Birth
- 7 Complications
A breech presentation is when the fetus presents buttocks or feet first (rather than head first – a cephalic presentation).
It has significant implications in terms of delivery – especially if it occurs at term (>37 weeks). Breech deliveries carry a higher perinatal mortality and morbidity, largely due to birth asphyxia/trauma, prematurity and an increased incidence of congenital malformations.
In this article, we shall look at the risk factors, investigations and management of a breech presentation.
Types of Breech Presentation
In a breech presentation, the fetus presents ‘bottom down’. There are three main types, depending on the position of the legs:
- Complete (flexed) breech – both legs are flexed at the hips and knees (fetus appears to be sitting ‘crossed-legged’).
- Frank (extended) breech – both legs are flexed at the hip and extended at the knee. This is the most common type of breech presentation.
- Footling breech – one or both legs extended at the hip, so that the foot is the presenting part.
Approximately 20% of babies are breech at 28 weeks gestation. The majority of these revert to a cephalic presentation (head down) spontaneously , and only 3% are breech at term.
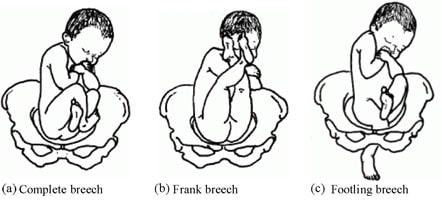
Fig 1 – The different types of breech presentation.
Aetiology and Risk Factors
Most breech presentations seem to be chance occurrences. However, in up to 15% of cases, it may be due to fetal or uterine causes. The risk factors are listed below:
Clinical Features
The diagnosis of breech presentation is of limited significance prior to 32-35 weeks (as the fetus is likely to revert to a cephalic presentation before delivery).
Breech presentation is usually identified on clinical examination . Upon the palpating the abdomen, the round fetal head can be felt in the upper part of the uterus, and an irregular mass (fetal buttocks and legs) in the pelvis.
Breech presentation can also be suspected if the fetal heart is auscultated higher on the maternal abdomen.
In around 20% of cases, breech presentation is not diagnosed until labour. This can present with signs of fetal distress, such as meconium-stained liquor . On vaginal examination, the sacrum or foot may be felt through the cervical opening.
Differential Diagnosis
There are two main differential diagnoses for a breech presentation:
- Oblique lie – the fetus is positioned diagonally in the uterus, with the head or buttocks in one iliac fossa.
- Transverse lie – the fetus is positioned across the uterus, with the head on one side of the pelvis and the buttocks on the other. The shoulder is usually the presenting part.
The other important diagnosis to consider is unstable lie . This is where the presentation of the fetus changes from day-to-day (and can include breech presentation). Unstable lie is more likely if there is known polyhydramnios or the woman is multiparous.
Investigations
Any suspected breech presentation should be confirmed by an ultrasound scan – which can also identify the type of breech (flexed/extended/footling). It can also reveal any fetal or uterine abnormalities that may predispose to breech presentation.
At term, the options for management of breech presentation are (i) external cephalic version; (ii) Caesarean section; or iii) vaginal breech birth.
External Cephalic Version
External cephalic version is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. This, if successful, can enable an attempt at vaginal delivery.
It has an approximate 50% success rate (40% success rate in a primiparous woman, and a 60% success rate in a multiparous woman). In contrast, only 10% of breech presentations spontaneously revert to cephalic in primiparous women.
ECV should be offered from 37 weeks gestation. In primiparous women, ECV can be offered from 36 weeks gestation.
Complications of ECV include transient fetal heart abnormalities (which revert to normal), and rarer complications such as more persistent heart rate abnormalities (e.g fetal bradycardia), and placental abruption . The risk of the woman needing an emergency Caesarean is around 1/200.
There is no consensus on the contraindications to ECV. Women should be informed that ECV after one Caesarean section delivery has no greater risk compared to ECV performed on an unscarred uterus.
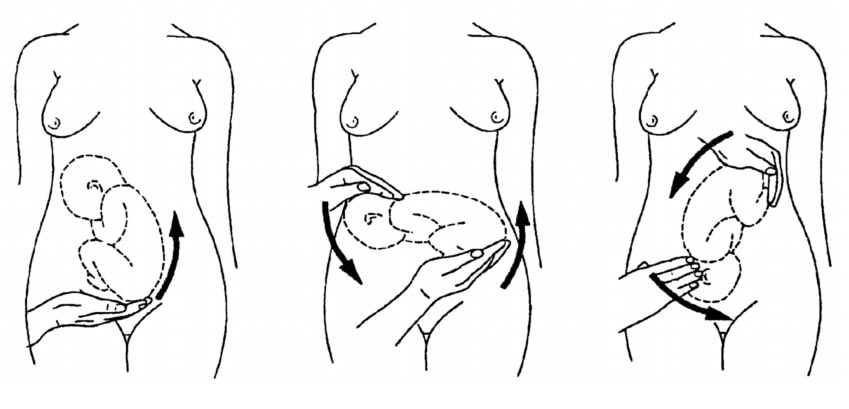
Fig 2 – External cephalic version.
If the external cephalic version is unsuccessful, contraindicated, or declined by the woman, current UK guidelines advise an elective Caesarean delivery .
This is based on evidence that perinatal morbidity and mortality is higher in cases of planned vaginal breech birth (compared to Caesarean) in term babies . There is no significant difference in maternal outcomes between the two groups.
The evidence for preterm babies is less clear, but generally C/S is preferred due to the increased head to abdominal circumference ratio in preterm babies.
Vaginal Breech Birth
A woman may still choose to aim for a vaginal breech delivery . Additionally, a small proportion of women with breech presentation present in advanced labour – with vaginal delivery the only option.
A contraindication to vaginal breech delivery is footling breech, as the feet and legs can slip through a non-fully dilated cervix, and the shoulders or head can then become trapped.
The most important advice when conducting a vaginal breech delivery is “ hand off the breech ”. This is because putting traction on the baby during delivery can cause the fetal head to extend, getting it trapped during delivery. The fetal sacrum does need to be maintained anteriorly, which can be done by holding the fetal pelvis. However, occasionally the baby does not deliver spontaneously, and some specific manoeuvres are required:
- Flexing the fetal knees to enable delivery of the legs.
- Using Lovsett’s manoeuvre to rotate the body and deliver the shoulders.
- The delivery of the aftercoming head can be challenging, but if MSV fails forceps can be used.
Complications
A major complication of breech presentation is cord prolapse (where the umbilical cord drops down below the presenting part of the baby, and becomes compressed). The incidence of cord prolapse is 1% in breech presentations, compared to 0.5% in cephalic presentations.
Other complications include:
- Fetal head entrapment
- Premature rupture of membranes
- Birth asphyxia – usually secondary to a delay in delivery.
- Intracranial haemorrhage – as a result of rapid compression of the head during delivery.
- 3% of babies are in breech presentation at term (>37 weeks), with a higher incidence in preterms.
- The main implication of breech presentation is on delivery.
- External cephalic version may be offered to turn the baby via the maternal abdomen to cephalic presentation. This is successful in around 50% of cases.
- If the baby remains breech, the options for delivery are by Caesarean section or vaginal breech.
- Current guidelines recommend Caesarean delivery, but a vaginal breech birth is possible with an experienced obstetrician or midwife.
A breech presentation is when the fetus presents buttocks or feet first (rather than head first - a cephalic presentation).
It has significant implications in terms of delivery - especially if it occurs at term (>37 weeks). Breech deliveries carry a higher perinatal mortality and morbidity, largely due to birth asphyxia/trauma, prematurity and an increased incidence of congenital malformations.
In a breech presentation, the fetus presents 'bottom down'. There are three main types, depending on the position of the legs:
- Complete (flexed) breech - both legs are flexed at the hips and knees (fetus appears to be sitting 'crossed-legged').
- Frank (extended) breech - both legs are flexed at the hip and extended at the knee. This is the most common type of breech presentation.
- Footling breech - one or both legs extended at the hip, so that the foot is the presenting part.
- Oblique lie - the fetus is positioned diagonally in the uterus, with the head or buttocks in one iliac fossa.
- Transverse lie - the fetus is positioned across the uterus, with the head on one side of the pelvis and the buttocks on the other. The shoulder is usually the presenting part.
Any suspected breech presentation should be confirmed by an ultrasound scan - which can also identify the type of breech (flexed/extended/footling). It can also reveal any fetal or uterine abnormalities that may predispose to breech presentation.
A woman may still choose to aim for a vaginal breech delivery . Additionally, a small proportion of women with breech presentation present in advanced labour - with vaginal delivery the only option.
- Birth asphyxia - usually secondary to a delay in delivery.
- Intracranial haemorrhage - as a result of rapid compression of the head during delivery.
[start-clinical]
[end-clinical]
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
- Health Boards
- NHS 111 Wales
404 - Page not found
This might be because you typed in the web address incorrectly. Please check the address and spelling.

IMAGES
COMMENTS
Breech Presentation Guideline (including ECV, Breech Birth and Emergency Procedure) WAHT-TP-094 Page 2 of 17 Version 7 Antenatal Management Women with a confirmed breech presentation should be reviewed at 36 weeks by an experienced member of staff to discuss on-going options for birth. The three options for management of breech at term are:
What causes a breech presentation? discus. Breech presentation may be more common if you have: • a low-lying placenta • lax muscles of the uterus (usually due to having a number of babies) • too much, or too little, amniotic fluid (waters) around the baby • an uncommon shape of the uterus, or large fibroids • previous breech presentation
Nov 6, 2022 · Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The 3 types of breech presentation are frank, complete, and incomplete. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of ...
In a frank breech presentation, the legs are extended, raised in front of the torso, with the feet near the head (Figure 6.1b). In a footling breech presentation (rare), one or both feet present first, with the buttocks higher up and the lower limbs extended or half-bent (Figure 6.1c). Figures 6.1 - Breech presentations 6.1.2 Diagnosis
Jun 9, 2024 · Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen. In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus.
Breech presentation is when the baby’s buttocks, foot or feet present instead of its head. Breech presentation is sometimes associated with uterine, placental, or fetal abnormalities. 3. Antenatal Management Breech presentation does not become clinically significant until 36 weeks gestation.
Management of Breech Presentation Breech presentation refers to a fetal position in which the baby's buttocks or feet are positioned to be delivered first instead of the head. While most babies naturally assume a head-down position for birth, occurring in about 3-4% of pregnancies, breech presentation presents unique challenges and
Aug 17, 2023 · Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered. ... During the entire procedure, the fetus's health will be monitored ...
Dec 4, 2024 · The diagnosis of breech presentation is of limited significance prior to 32-35 weeks (as the fetus is likely to revert to a cephalic presentation before delivery). Breech presentation is usually identified on clinical examination. Upon the palpating the abdomen, the round fetal head can be felt in the upper part of the uterus, and an irregular ...
Breech Presentation Guideline 1. INTRODUCTION Breech presentation occurs in 3-4% of term deliveries and is more common preterm. It is associated with uterine and congenital abnormalities, has a significant recurrence risk and is more common in nulliparous people. Term babies presenting in breech position have worse