Nursing Process and Critical Thinking
1. Explain the use of each of the six phases of the nursing process.
2. List the elements of each of the six phases of the nursing process.
3. Describe the establishment of the database.
4. Discuss the steps used to formulate a nursing diagnosis.
5. Differentiate between types of health problems.
6. Describe the development of patient-centered outcomes.
7. Discuss the creation of nursing orders.
8. Explain the evaluation of a nursing care plan.
9. Demonstrate the nursing process by preparing a nursing care plan.
10. Explain North American Nursing Diagnosis Association International (NANDA-I), Nursing Interventions Classification (NIC), and Nursing Outcomes Classification (NOC).
11. Describe the use of clinical pathways in managed care.
12. Discuss critical thinking in nursing.
13. Define evidenced-based practice.
http://evolve.elsevier.com/Cooper/foundationsadult/
According to the American Nurses Association (ANA), the current definition of nursing states, “Nursing is the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations” ( ANA, 2013 ). This broad definition seeks to illustrate nursing's growth as a profession. The nursing process serves as the organizational framework for the practice of nursing.
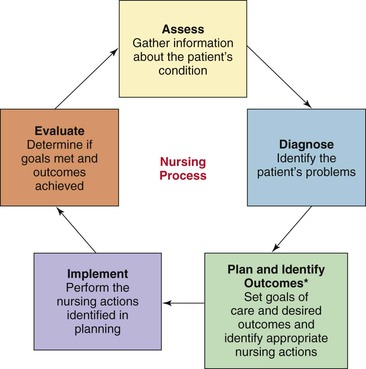
The nursing process is a systematic method by which nurses plan and provide care for patients. This involves a problem-solving approach that enables the nurse to identify patient problems and potential problems. Once these problems are identified, the nurse is then able to plan, deliver, and evaluate nursing care in an orderly, scientific manner. The nursing process consists of the following six dynamic and interrelated phases: assessment, diagnosis, outcomes identification, planning, implementation, and evaluation ( Figure 5-1 ). Box 5-1 describes how the nursing process is carried out by the registered nurse (RN) and licensed practical/vocational nurse (LPN/LVN). (The licensed practical/vocational nurse [LPN/LVN] has a significant role in the nursing process, which is discussed subsequently in the chapter.)
Implementation of the Nursing Process by the RN and LPN/LVN
Assessment: The RN is responsible for the initial assessment of the patient; the LPN/LVN assists the RN with ongoing assessments.
Diagnosis: The RN is responsible for identifying the appropriate nursing diagnosis for the patient with the assistance of the LPN/LVN.
Outcomes Identification: The RN develops individualized goals/expected outcomes directly associated with the nursing diagnoses. The LPN/LVN can also assist the RN with identifying these outcomes.
Planning: The RN, with assistance from the LPN/LVN, plans interventions that will help meet the patient’s desired goals/expected outcomes.
Implementation: The RN and LPN/LVN implement the proposed plan.
Evaluation: The RN and LPN/LVN perform ongoing assessments, allowing the RN to determine whether proposed goals/outcomes have been met.

Assessment Data
The ANA defines assessment as “a systematic, dynamic process by which the registered nurse, through interaction with the patient, family, groups, communities, populations, and health care providers, collects and analyzes data. Assessment may include the following dimensions: physical, psychological, sociocultural, spiritual, cognitive, functional abilities, developmental, economic, and lifestyle” ( ANA, 2010 ). Information is gathered by the nurse to identify the condition of the patient's health. The nurse performs a patient assessment on initial contact with the patient, with the remaining phases of the nursing process dependent on the accuracy and completeness of this initial data collection. Either a complete assessment or a focused assessment is performed, depending on the patient's status and the type of facility. The LPN/LVN assists the registered nurse by performing ongoing complete and focused assessments of patients, depending on the facility and scope of practice within a state.
A complete assessment involves a review and physical examination of all body systems (musculoskeletal, respiratory, gastrointestinal, etc.) (see Chapter 12 ). This type of assessment also includes cognitive, psychosocial, emotional, cultural, and spiritual components and is appropriate for a patient with a stable condition who is not in acute distress. Information about functional abilities, lifestyle, and developmental concerns is also important.
A focused assessment is advisable when the patient is critically ill, disoriented, or unable to respond. A focused assessment is used to gather information about a specific health problem. For example, if the patient reports abdominal distention, lack of appetite, and straining to have a bowel movement, one possible nursing diagnosis to suspect is constipation. For further investigation, the nurse may ask additional questions about intake of foods high in fiber, fluid intake, and amount of exercise.
Focused assessments are also performed continuously throughout nurse-patient contact. The nurse who monitors intake and output, skin turgor, and oral mucous membranes is performing a focused assessment for deficient fluid volume ( Ackley and Ladwig, 2011 ). Assessments made to determine progress toward the achievement of desired outcomes are also focused assessments.
Types of Data
In an assessment, the nurse gathers subjective and objective data. A cue is a piece or pieces of data that often indicates that an actual or potential problem has occurred or will occur. Subjective data refer to information that is provided by the patient. Statements about nausea and descriptions of pain, fatigue, and anxiety are examples of subjective data. Other terms for subjective data are symptoms and subjective cues. Subjective data are hidden until shared by the patient.
Objective data are observable and measurable signs. For example, the LPN/LVN is able to observe capillary refill, measure a patient's blood pressure, and observe and measure edema. Other terms for objective data are signs and objective cues. Table 5-1 shows a comparison of subjective and objective data.
Comparison of Subjective and Objective Data
Sources of Data
Data are obtained from primary or secondary sources. The primary source of data is the patient. In most instances, the patient is considered to be the most accurate reporter. The alert and oriented patient is able to provide information about past illnesses and surgeries and present signs, symptoms, and lifestyle.
When the patient is unable to supply adequate information because of deterioration of mental status, age, or seriousness of illness, the nurse turns to secondary sources. Secondary sources include family members, significant others, medical records, diagnostic procedures, and previous nursing progress notes. Members of the patient's support system are often able to furnish information about the patient's past health status, current illness, allergies, and current medications.
Health team professionals are also helpful secondary sources. Health care providers, nurses, dietitians, respiratory and physical therapists, and others frequently provide data about the patient. The nurse should review nursing literature to determine what information may be needed. Nursing textbooks are a good resource for information about etiology (cause), pathophysiology, clinical manifestations, assessment, diagnostic tests, medical management, nursing interventions, patient teaching needs, and prognosis. This important information then guides further data collection.
Methods of Data Collection
Two basic methods are used to collect data. In the first method, the nurse conducts an interview, the nursing health history, to obtain information about the patient's health history. The nurse commonly assesses several common components in the course of the interview. Biographic data provide information about the facts or events in a person's life. Additional information collected includes the reason the patient is seeking health care, a history of the present illness, the health history, and the family history. Because the environment in which the patient lives and works often plays a part in the patient's health status, an environmental history is important to obtain. A psychosocial history yields information about a combination of psychological and social factors. When gathering information about the function of each body system, the nurse follows the nursing health history with a review of systems.
The second method of data collection is the physical examination. The physical examination is often guided by subjective data provided by the patient. For example, the nurse should follow up with a thorough assessment of any body part or system for which the patient has reported symptoms or concerns. A head-to-toe format provides a systematic approach that helps avoid omission of important data (see Chapter 12 ).
A completed nursing health history and a physical examination allow the nurse to establish a database (a large store or bank of information) for the patient. Analysis of the database leads to the identification of nursing diagnoses. In addition, the database makes information available for the health care provider who assists in the medical management of the patient and all health care personnel who are involved in the patient's care.
Data Clustering
Data obtained from the health history, physical examination, and related diagnostic procedures are analyzed in development of a plan of care. Data clustering is one method of data organization. The clustering of related data helps to identify patterns that assist with the identification of nursing diagnoses. Some schools of nursing or health care facilities use the term defining characteristics as a synonym for data clustering. Examples of data clustering and the related nursing diagnosis include:
• Urine loss associated with physical exertion and urine loss associated with increased abdominal pressure are cues for the nursing diagnosis of stress urinary incontinence ( Ackley and Ladwig, 2011 ).
• Abnormal blood pressure and heart rate response to activity, exertional dyspnea, verbal report of fatigue or weakness are cues for the nursing diagnosis of activity intolerance ( Ackley and Ladwig, 2011 ).
To diagnose is to identify the type and cause of a health condition. The ANA defines diagnosis as “a clinical judgment about the client's response to actual or potential health conditions or needs. The diagnosis provides the basis for determination of a plan of care to achieve expected outcomes” ( ANA, 2010 ). The LPN/LVN and the registered nurse (RN) observe and collect data. Once the initial assessment has been completed, the data require analysis. In most situations, the RN is responsible for analyzing and interpreting data to identify health problems ( Table 5-2 ). The RN often collaborates with the LPN/LVN when determining the nursing diagnosis.
Determination of Significant Cues
* Conclusion is based on the appropriate norm for the age and sex of the patient.
Nursing Diagnosis
A nursing diagnosis is a type of health problem that can be identified. In 1990, the North American Nursing Diagnosis Association (NANDA) was created; in 2002, NANDA became NANDA International (NANDA-I) to reflect nursing diagnosis terminology that is used across the world. NANDA-I approves the official definition for a nursing diagnosis. A nursing diagnosis is a “clinical judgment about actual or potential individual, family, or community responses to health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability” ( NANDA-I, 2012 ). Nurses are legally permitted to identify and prescribe the primary interventions to treat or prevent problems that are nursing diagnoses. The nurse must be aware of this important point. By definition, if the nurse is not able to prescribe the primary treatment, the problem is not a nursing diagnosis.
Components of a Nursing Diagnosis
Nursing research is ongoing in its identification of nursing diagnoses. When nurses submit nursing diagnoses, the following four components are addressed: (1) nursing diagnosis title or label; (2) definition of the title or label; (3) contributing, etiologic, or related factors; and (4) defining characteristics. The diagnosis should also be research based. The selection of an accurate nursing diagnosis depends on closely matching the elements in the patient situation with all four components of the nursing diagnosis. These four components are found in numerous nursing diagnosis handbooks, and each component is explained in the following discussion.
Title or label.
The problem that is identified based on a pattern of related cues and this analysis is given a title or label. Frequently, the name given to the problem is simply called the nursing diagnosis. In this chapter, the terms nursing diagnosis and nursing diagnostic label are used to describe this component. The nursing diagnosis provides a concise name for the identified health problem. Lists of nursing diagnoses are often presented in alphabetical order. Constipation, fatigue, hopelessness, powerlessness, and pain are examples of nursing diagnostic labels.
Adjectives add meaning to the nursing diagnosis label by describing or modifying the label. Examples of adjectives are imbalanced, ineffective, perceived, impaired, and excess. The nursing diagnoses listed in the nursing care plans and nursing process sections of this book follow the format used by NANDA-I in the original list (i.e., placing the noun first for easier location and identification in a list). When writing the nursing diagnosis, however, the adjective is placed before the noun modified. This provides a more natural word order and is less awkward. For example, impaired physical mobility is easier to say and understand than mobility, impaired physical.
Both international nursing groups and American nurses have challenged NANDA-I to simplify the language of nursing diagnoses. Although this is ongoing work, many labels have already undergone modification. Altered comfort: pain has been shortened to acute pain or chronic pain. Similarly, alteration in bowel elimination: constipation has been changed to constipation.
NANDA-I currently uses an organization structure for the diagnostic labels that is called Taxonomy II. New modifiers have been suggested as part of the organizational system. (See Table 5-3 for terms and their definitions.) The work of NANDA-I was never intended to be stagnant, so the nurse must monitor language changes and label additions every 2 years following the NANDA-I meetings. The nurse may also visit the NANDA-I website at www.nanda.org to keep current with the changes. A new feature at NANDA-I is the periodic opportunity to vote on new diagnoses.
Descriptors for Taxonomy II
Used with permission from North American Nursing Diagnosis Association–International (NANDA-I): Nursing diagnoses: Definitions and classification 2012–2014, Hoboken, N.J., 2012, Wiley-Blackwell.
Definition.
The definition presents a clear, precise description of the problem. This description helps identify the difference between similar nursing diagnoses. For example, if the nurse is deciding whether to select constipation or perceived constipation, the definitions are helpful. Constipation is defined as “Decrease in normal frequency of defecation accompanied by difficult or incomplete passage of stool and/or passage of excessively hard, dry stool” ( Johnson et al., 2012 , p. 75). Perceived constipation is defined as “Self-diagnosis of constipation and abuse of laxatives, enemas, and/or suppositories to ensure a daily bowel movement” ( Johnson et al., 2012 , p. 76). For the most appropriate diagnosis, the nurse should refer to the definitions for nursing diagnoses in nursing diagnosis handbooks.
Contributing, etiologic, and related factors and risk factors.
Contributing, etiologic, and related factors are conditions that are often involved in the development of a problem. These topics are covered in nursing diagnosis handbooks. The factors may become the focus for nursing interventions. Most authors also refer to a contributing factor as a “related to.” Contributing, etiologic, and related factors are written as the “related to” in actual nursing diagnoses statements. A contributing, etiologic, or related factor for the nursing diagnosis of anxiety is a change in some area of the person's life, such as health, economics, or role function ( Ackley, 2011 ).
Risk factors are circumstances that increase the susceptibility of a patient to a problem. Prolonged immobility increases the risk for skin impairment and is a risk factor for the nursing diagnosis of impaired skin integrity. Risk factors are written as the “related to” in risk nursing diagnostic statements.
Defining characteristics.
Defining characteristics are the clinical cues, signs, and symptoms that furnish evidence that the problem exists. The cues, signs, and symptoms that were identified in the patient's assessment are prefaced with “as evidenced by” in the nursing diagnosis statement. Examples are presented in the following discussion of the writing of nursing diagnostic statements. Look for defining characteristics for each nursing diagnosis title or label in nursing diagnosis handbooks.
Writing Nursing Diagnosis Statements
The four main types of nursing diagnoses are: actual, risk, syndrome, and health promotion. The following discussion provides descriptions of each type and furnishes guidelines for writing each type of nursing diagnosis statement.
Actual nursing diagnosis.
NANDA-I's description of an actual nursing diagnosis is “a clinical judgment about human experience/responses to health conditions/life processes that exist in an individual, family, or community” ( NANDA-I, 2012 ). Cues obtained from a nursing assessment indicate that a problem exists. In an educational setting, the actual nursing diagnosis statement is usually represented by a three-part statement. In a clinical setting, only the first two parts of the statement are typically used. The three parts are written in the following order: (1) the nursing diagnosis label from the NANDA-I list; (2) the contributing, etiologic, or related factor; and (3) the specific cues, signs, and symptoms from the patient's assessment. Connecting phrases are used to join the three parts of the statement. “Related to” (r/t) links the first and second parts of the statement. “As evidenced by” (AEB) joins the second and third parts of the diagnostic statement. Note the italicized connecting words of an actual nursing diagnostic statement in the following example.
• Constipation, related to insufficient fluid intake as evidenced by increased abdominal pressure, no bowel movement for 5 days, and straining with defecation.
Risk nursing diagnosis.
NANDA-I defines a risk nursing diagnosis as a clinical judgment that “describes human responses to health conditions/life processes that may develop in a vulnerable individual/family/community. It is supported by risk factors that contribute to increased vulnerability” ( NANDA-I, 2012 ). The assessment indicates that risk factors are present that are known to contribute to the development of the problem. Risk nursing diagnoses are written as two-part statements: (1) the nursing diagnosis label from the NANDA-I list; and (2) the risk factor(s). As in an actual nursing diagnosis, the two parts are connected by the words “related to.” An example of a risk nursing diagnosis statement is as follows:
• Risk for impaired skin integrity, related to physical immobilization
Note that no third part (as evidenced by) is seen in this statement. If signs or symptoms were found, an actual problem would exist.
Syndrome nursing diagnosis.
A syndrome nursing diagnosis is “a clinical judgment describing a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions” ( NANDA-I, 2012 ). Posttrauma syndrome, risk for disuse syndrome, impaired environmental interpretation syndrome, and relocation stress syndrome are the current syndrome diagnoses. Because these diagnoses are so specific, the syndrome diagnoses are usually written as one-part statements.
Health promotion nursing diagnosis.
NANDA-I describes a wellness nursing diagnosis as “a clinical judgment about a person's, family's or community's motivation and desire to increase wellbeing and actualize human health potential as expressed in the readiness to enhance specific health behaviors, and can be used in any health state” ( NANDA-I, 2012 ). A wellness nursing diagnosis is written as a one-part statement. The words “readiness for enhanced” are used in a wellness nursing diagnosis. An example of a wellness nursing diagnosis is readiness for enhanced self-health management ( Ackley, 2011 ).
Other Types of Health Problems
Collaborative problems and medical diagnoses must be distinguished from nursing diagnoses. These two types of problems are defined and discussed separately.
Collaborative Problems
Collaborative problems are health-related problems that the nurse anticipates based on the condition or diagnosis of a patient. Both health care provider–prescribed and nursing-prescribed interventions (discussed subsequently in this chapter) are used in the management of collaborative problems ( Carpenito, 2013 ). An example of a collaborative problem is the care of a patient with hypertension who is taking a new medication for the condition. The potential for hypotension is considered a collaborative problem because prevention uses both physician-prescribed interventions (i.e., adjustment of the hypertensive medications as needed) and nursing-prescribed interventions (i.e., monitoring of the patient's blood pressure, assistance when the patient goes from a sitting to standing position). If the prevention or treatment of the problem is primarily the nurse's responsibility, the problem is identified as a nursing diagnosis. Risk for infection for the new postoperative surgical case is a potential complication that is a nursing responsibility.

Medical Diagnosis
A medical diagnosis is the identification of a disease or condition with evaluation of physical signs, symptoms, patient interview, laboratory tests, diagnostic procedures, review of medical records, and patient history. The health care provider is licensed to make and treat medical diagnoses. Examples of medical diagnoses are congestive heart failure, pneumonia, diabetes mellitus, and hepatitis B.
Differentiation of Medical and Nursing Diagnoses
Students often have difficulty with the distinction between a medical and a nursing diagnosis. Health care providers, including physicians and advanced practice nurses, diagnose diseases or disorders such as those listed previously. These diseases or disorders are the result of changes in the structure or the function of an organ or body system. Diagnostic studies such as x-ray examinations and laboratory studies help with identification of medical diagnoses. Although the patient is often able to recover from a medically diagnosed condition, the diagnosis itself does not change. The patient who recovers from a heart attack (myocardial infarction) has a history of a myocardial infarction. The patient who was diagnosed with diabetes is likely to still have diabetes.
In the case of nursing diagnoses, the situation is different. Nursing diagnoses address human responses to health problems and life processes. The nurse addresses the patient's concerns about the medical problem. If a patient is diagnosed with cancer, the nurse has the opportunity to address the patient's responses to the diagnosis; responses to the disease may include anxiety, fear, anticipatory grieving, activity intolerance, and nausea. These problems often change as the LPN/LVN carries out interventions. The nurse may assist the patient who is concerned about dying with grief resolution or perhaps teach the patient coping strategies. A nursing diagnosis may change or resolve as care is provided or the condition changes. The medical diagnosis of cancer may not go away; however, the goal for the patient may be the ability to resolve feelings of fear regarding the diagnosis, prognosis, and treatment through nursing interventions addressed in the care plan.
Outcomes Identification
The nurse, in collaboration with the patient, develops expected outcomes for the established nursing diagnosis. The outcomes statement indicates the degree of wellness desired, expected, or possible for the patient to achieve and contains a patient goal statement. The ANA uses the term outcome identification , but alternative terms for this statement are a patient goal, a patient-centered goal, an objective, a behavioral objective, or a patient outcome. A patient outcome statement provides a description of the specific, measurable behavior (outcome criteria) that the patient will be able to exhibit in a given time frame after the interventions. The nurse must avoid writing a goal statement that is centered on nursing interventions because this indicates what the nurse is meant to do rather than what the patient is to do.
Desired patient outcome statements serve two functions. First, they guide the selection of nursing interventions. Nursing interventions are selected to promote the achievement of the desired outcome. Second, the outcome statement establishes the measuring standard that is used to evaluate the effectiveness of the nursing interventions. Therefore, the outcome statement has to provide the specific details that can be used as the benchmark to judge progress or solution of the problem.
A well-written patient-centered goal or desired patient outcome statement does the following:
• Uses the word patient or a part of the patient as the subject of the statement
• Uses a measurable verb
• Is specific for the patient and the patient's problem
• Does not interfere with the medical plan of care
• Is realistic for the patient and the patient's problem
• Includes a time frame for patient reevaluation
Because the subject of the patient outcome statement is meant to be the patient or a part of the patient, the outcome statement should begin with the words, “The patient will” or “The patient's . . . will.”
Measurable verbs indicate the precise behavior that the nurse anticipates hearing or seeing. Define, describe, list, walk, demonstrate, and verbalize are examples of measurable verbs.
The properly written patient outcome statement is specific to the patient and the patient's health problem. A patient who is in traction because of a bone fracture has mobility restrictions. An outcome statement indicating that all joints will be moved through full range of motion is not safe for this patient's problem.
The patient outcome statement also has to be realistic for the patient and the patient's health problem. Although some 88-year-old patients are joggers, the expectation that an 88-year-old patient will learn to jog is probably not reasonable.
A time frame is written into the patient outcome statement to provide a deadline for evaluation of the patient's progress. Nursing experience assists the nurse in accurate prediction of realistic time frames.
Patient outcome statements indicate a reversal of the problem identified by the NANDA-I nursing diagnosis label, as shown in the following example:
Patient outcome statements can be written in two ways. The previous example illustrates the simple reversal of the problem statement in a concise fashion. A second approach is to list the desired behavior in broader terms and then list exact criteria or standards; this may also be referred to as a long-term and short-term goal. The following example first lists the long-term goal, with the second example the short-term goal:
• The patient will use her walker to ambulate at all times rather than using her wheelchair within the next 2 months.
• The patient will participate in range-of-motion exercises on her lower extremities bilaterally two times a day.
• The patient will ambulate 20 feet every day with assistance of her walker, increasing distance ambulated by 5 feet daily.
During the planning phase of the nursing process, priorities of care are established and nursing interventions are chosen to best address the nursing diagnosis. This information is typically communicated through the care plan so that all health care personnel directly involved in care of the patient can follow the same plan, resulting in continuity of care. The nurse must work with the patient and significant others in choosing appropriate interventions and in considering evidenced-based practice guidelines. The plan of care should be comprised of standardized languages or recognized terminology to document and effectively communicate the plan.
Priority Setting
The nurse in today's busy health care facility is caring for many patients with complex problems and is challenged daily to use time and effort wisely. Priorities must be established to provide care for each patient.
Once nursing diagnoses have been identified, the registered nurse must prioritize the diagnoses according to the patient's current health status. The framework most often used to guide the prioritization is Maslow's hierarchy of needs. This structure is based on the principle that lower-level needs must be met before higher-level needs can be satisfied. The physiologic needs are more vital than the safety and security needs, and the safety and security needs are more critical than the love and belonging needs. Review Maslow's hierarchy in Figure 1-8 . Life-threatening and health-threatening problems are ranked before other types of problems. Actual problems often are ranked before risk problems, unless the risk problems, if they were to develop, are life threatening. For example, risk for ineffective airway clearance might be prioritized higher than an actual problem of constipation. With use of Maslow's hierarchy, the nurse can determine whether the actual or risk for nursing diagnosis has the highest priority. The nurse must also take into consideration the patient's thoughts and feelings regarding prioritization of problems. If patients are not active participants in the plan of care, they are not likely to be driven to work towards meeting the agreed-upon goals.
Time factors and severity of illness are important considerations in the determination of what problems to address initially. The patient who is admitted to the emergency department with a possible heart attack (myocardial infarction) is not ready at that time to contemplate dietary instructions to reach a goal of reducing cholesterol.
Priorities change as the patient progresses through time in a health care facility. As some problems are resolved, the approach to other problems opens up. Consider the following scenario and how the concerns of nursing change during one patient's hospital stay.
A 28-year-old woman admitted for an abdominal hysterectomy may have the preoperative diagnosis of fear or anxiety. Acute pain is an important nursing diagnosis in the first few days after surgery. As the pain is controlled, imbalanced nutrition: less than body requirements and risk for constipation are managed. When the patient approaches discharge, teaching about wound care and activity restrictions becomes the focus for nursing diagnoses. Because of the loss of reproductive ability, self-esteem problems have to be confirmed or ruled out as possible nursing diagnoses for this patient. Note how the nursing diagnoses changed, but the medical procedure did not.
Selecting Nursing Interventions
Nursing interventions are those activities that promote the achievement of the desired patient outcome. Interventions include activities that the nurse selects, in partnership with the patient, to resolve a nursing diagnosis, monitor for the development of a risk problem, or carry out physician orders. Nursing interventions are classified as physician prescribed or nurse prescribed.
Physician-prescribed interventions are those actions ordered by a physician for a nurse or other health care professional to perform. Remember that physician orders are not orders for nurses but are prescriptive instructions for patients ( Carpenito, 2013 ). Although the physician has given the order, nursing judgment must still be used. The LPN/LVN must follow orders when administering medications, performing wound care, and ordering diagnostic tests. Assessing, teaching, and validating the safety of physician orders are important nursing responsibilities. In this text, the term “health care provider” has been used to encompass those health care professionals who have prescriptive authority, such as physicians, advanced practice nurses, and physician's assistants. The term “physician-prescribed interventions” applies to these individuals.
Nurse-prescribed interventions are any actions that a nurse is legally able to order or begin independently. Nurses write interventions for themselves or other nursing staff ( Carpenito, 2013 ). Examples of independent nursing interventions are providing a back massage, turning a patient every 2 hours, and monitoring for complications. When determining appropriate nursing interventions, the nurse should consider the contributing, etiologic, and related factors; risk factors; the patient-centered goal or desired patient outcome; and the nursing diagnosis label itself. Nursing interventions are focused on any or all of these areas.
Nursing interventions often are aimed at reducing or eliminating the causative factor. For example, for the nursing diagnosis anxiety, related to lack of knowledge about hospital procedures, an appropriate nursing intervention is to teach the patient about typical routines and procedures. Providing information addresses any knowledge deficit, which helps to reduce the fear of the unknown, thereby reducing anxiety.
The patient outcome is also considered when selecting nursing interventions. For example, when the patient outcome statement says, “The patient will plan a week's menu for an 1800-calorie diabetic diet within 1 week's time,” the interventions are selected to increase the patient's knowledge about planning for a diabetic diet.
The nursing diagnosis label itself may also direct the interventions. If the nursing diagnosis label is acute pain, interventions to relieve acute pain are selected.
A variety of sources list nursing interventions. Nursing textbooks, periodicals, and care planning books are helpful sources of information. The Nursing Interventions Classification (NIC) may be another helpful source for nursing interventions and activities. (The NIC is discussed subsequently in this chapter.) Nursing colleagues and previous experience in nursing care are also good sources of ideas for interventions, as are patient suggestions regarding care. In addition, nursing conferences held to plan patient care often provide an environment for the development of creative approaches to patient care.
Writing Nursing Interventions
Because nursing interventions offered in textbooks and care planning resources are often broad general statements that indicate an activity to be performed, these nursing interventions need to be converted to more specific instructional statements. Suggested interventions for constipation may include increase dietary bulk, increase activity, and encourage fluids.
This information is helpful because it prescribes a direction for care, but the information provided is lacking in specific details. The nurse must determine specific information regarding interventions so that any person following the direction of the care plan can carry out interventions without question. For care planning purposes, the nurse must be able to change the guiding general statement about the nursing intervention to a more specific statement. Nursing interventions have to be written to reduce the likelihood of misinterpretation. Details are provided to convey the intended meaning. Written nursing interventions should include the subject (the nurse is assumed unless stated otherwise), action verb, and qualifying details. Consider the following interventions:
• Ambulate the patient three times a day at 0900, 1400, and 1900.
• Ambulate the patient 30 feet three times a day at 0900, 1400, and 1900.
The correctly written nursing intervention is the second one because it contains the subject (the nurse is assumed), the action verb (ambulate), and the qualifying details (30 feet three times a day). This intervention is specific and easily interpreted by any health care professional following the care plan.
A properly written nursing intervention is specific for the problem, realistic for the patient, compatible with the medical plan of care, and based on scientific, evidenced-based principles. The following examples illustrate appropriate conversion of general nursing interventions into specific nursing interventions:
• Add four servings of fruits and vegetables of patient's choice to daily menu, one extra serving per meal and one snack.
• Turn the patient every 2 hours with the assistance of two personnel and the lift sheet.
• Offer water and juices up to 2000 mL per day according to the following schedule: 7 to 3 shift, 1200 mL; 3 to 11 shift, 600 mL; 11 to 7 shift, 200 mL.
Communicating the Nursing Care Plan
After completing the initial assessment, analyzing the data, writing the nursing diagnoses, selecting outcomes, and selecting appropriate nursing interventions (which are then made more specific with written nursing interventions), the nurse has the responsibility to communicate the detailed plan of care for the patient. The written nursing care plan is the tangible product of the nursing process ( Table 5-4 ). (Refer to Chapter 3 for additional information on charting and documentation.)
Nursing Care Plan Form
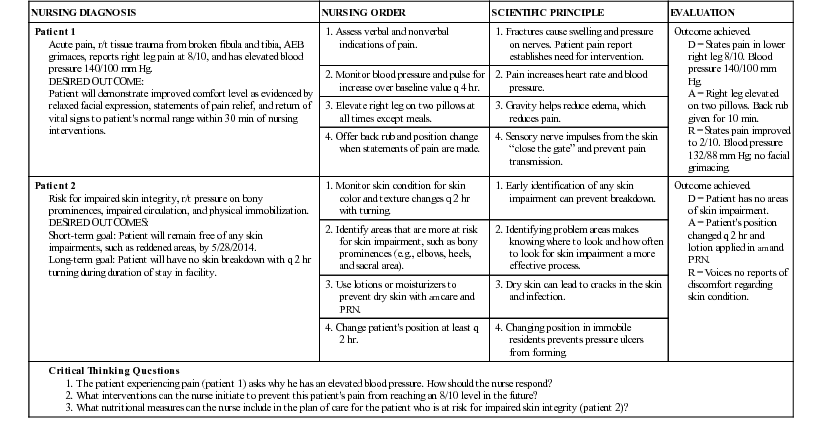
A, Action; D, data; AEB, as evidenced by; PRN, as needed; q 2 hr, every 2 hours; R, response/evaluation; r/t, related to.
Because the nursing staff constantly changes (nurses work different shifts and have days off), written guidelines are important for continuity of patient care. Continuity increases patient trust in the nursing staff and promotes outcome achievement.
Nursing care plans may be specifically written for a patient, or the nurse may use a standardized care plan for a patient. The nurse must individualize each care plan to the patient, even with use of standardized care plans. Individually prepared care plans are the most time consuming but often provide care that is best matched to the specific patient's needs and situation. An individualized plan of care takes into consideration pertinent patient characteristics such as age, culture, and medical diagnosis.
Standardized nursing care plans are appropriate for patient populations with routine, expected care requirements. Women who have had a vaginal delivery or a cesarean delivery are ideal patient populations for standardized care plans. Many standardized care plans include blank spaces that the nurse fills in to individualize to some degree.
Linear Care Plans versus Concept Maps
Among nursing faculty, a range of different expectations often exists for the care planning process. Formats for the written nursing care plan vary from school to school. Components that are common in an educational setting are NANDA-I diagnostic labels, patient-centered goals and desired patient outcomes, and nursing interventions and orders.
Nursing faculty may require students to submit the care plan in a four-column or five-column format that is referred to as a linear style. With this system, rationale is often necessary to explain why the intervention is needed or how the intervention will work. This encourages the student to use critical thinking skills and evidence-based practice for supporting the nursing interventions chosen.
Other nursing faculty may prefer the care plan to be represented as a concept map. A concept map, with use of different shapes and connecting lines to show relationships, provides a visual representation of the care plan ( Berman et al., 2008 ). With concept mapping, the student may put the nursing diagnosis into a rectangular shape in the middle of the page; interventions are in circles that branch off from the nursing diagnosis, and outcomes are placed into a triangle. The student should follow the specific guidelines of the nursing program for topics to be included on a concept map and its organization.
Implementation
During the implementation phase of the nursing process, the nurse and other members of the team put the established plan into action to promote outcome achievement. This is the fifth phase of the nursing process. With evidence-based interventions, the nurse should ensure that the plan is implemented in a timely and safe manner.
In emergency situations, the nursing process as a means of problem solving is accelerated. The nurse proceeds directly from assessment of the problem to intervention. If a patient has gone into cardiac or respiratory arrest, the nurse initiates cardiopulmonary resuscitation immediately.
Nursing interventions include both nurse-prescribed and physician-prescribed activities. (See the discussion of selecting nursing interventions in the previous “Planning” section in this chapter.) According to the ANA Scope and Standards of Practice (2010) , implementation for nursing intervention includes activities such as teaching, monitoring, providing, counseling, delegating, and coordinating.
Evidence-Based Practice
Nursing research is the basis for evidence-based practice. Nursing research was cultivated in the 1950s, leading to the development of nursing theories in the 1960s and 1970s. In the 1990s, nursing theories were researched and further tested to expand the field of nursing and evidence-based practice. Nursing research today continues to solidify theories and practice and introduce new theories. Other disciplines such as sociology, psychology, biology, and physics are incorporated into nursing theory.
The ANA Scope and Standards of Practice (2010) defines evidence-based practice as: “a scholarly and systematic problem-solving paradigm that results in the delivery of high-quality health care. In order to make the best clinical decisions using EBP, external evidence from research is blended with internal evidence (i.e., practice-generated data), clinical expertise, and healthcare consumer values and preferences to achieve the best outcomes for individuals, groups, populations, and healthcare systems.”
Evaluation is a determination made about the extent to which the established outcomes have been achieved. The nurse takes several steps to complete the evaluation phase. (1) Review the patient-centered goals or desired patient outcomes that were established previously. These outcome statements present standards and criteria that are observable and measurable. (2) Reassess the patient to gather data that indicate the patient's actual response to the nursing interventions. (3) Compare the actual outcome with the desired outcome and make a critical judgment about whether the patient-centered goal or desired patient outcome was achieved.
This critical judgment leads the nurse to make one of three conclusions or decisions: the outcome was achieved, the outcome was not achieved, or the outcome was partially achieved. Evaluation of the desired patient outcome is illustrated in the following statement:
The plan of care generally undergoes changes during this phase of the nursing process. The nurse makes modifications according to whether the outcome has been achieved, partially achieved, or not achieved. When a problem has been resolved, it is removed from the nursing care plan.
When the outcome has been partially achieved or not achieved, further analysis is needed. At this point, the nurse should review all phases of the nursing process. The following are examples of questions the nurse should consider to ensure the accuracy of the nursing process:
• Was the assessment complete and accurate?
• Was the problem identified correctly?
• Was the desired patient outcome realistic and specific?
• Were the interventions realistic, and did all personnel implement them consistently?
• Did new problems develop?
• Was adequate time allowed?
Once the nurse has determined the answers to these questions, the nursing care plan can be modified accordingly.
Standardized Languages: NANDA-I, NIC, and NOC
Effective communication in the health care setting is vital in providing consistent quality care for patients. Nurses work in a variety of settings, and patients may be cared for in a variety of settings, sometimes with transfer from one facility to another. The use of a standardized language (terms that have the same definition and meaning regardless of who uses them) fosters communication regarding aspects of patient care.
NANDA-I, Nursing Interventions Classification (NIC), and Nursing Outcomes Classification (NOC) provide standardized nursing diagnoses, nursing intervention, and nursing-sensitive patient outcomes. These classification systems further provide research-based information regarding nursing treatments and judgments. NANDA-I, NIC , and terminology are used internationally in all patient settings, including acute care hospitals, long-term care facilities, outpatient and ambulatory settings, and home care. The benefits of these systems are support for the framework for clinical decisions, evidence-based plans of care, and support of effective staffing, student learning, and staff education. The groups behind NANDA-I, NOC, and NIC (NNN) are working together to demonstrate links between these three standardized languages and thus to improve communication both in the United States and internationally. An example of an NNN linkage is listed as follows ( Johnson et al., 2012 ):
Nursing Interventions Classification (NIC)
This standardized language, developed at the University of Iowa, encourages enhanced communication between nurses about nursing interventions. The current NIC edition lists more than 500 interventions and 13,000 activities. Each NIC intervention has a label, a definition for that label, a list of activities that can be used for that intervention, and background information. The label and definition should not be altered when they are used, but the activities can be individualized to the patient's needs. The title given to nursing interventions is concise. Examples of nursing interventions are airway management; analgesic administration; teaching: prescribed diet; and therapeutic play. Some NIC interventions are called indirect interventions because they occur away from the bedside but on behalf of the patient. Examples of indirect care interventions are emergency cart checking, shift report, staff development, and supply management ( Bulechek et al., 2013 ).
The list of activities is very helpful to guide beginning nurses. The following example shows a NIC intervention and lists 3 of the 36 possible activities for the intervention ( Bulechek et al., 2013 ). Note the definition given and the indicated number that can be retrieved with computer systems. These numbers “run in the background” and are not for memorization.
NIC intervention: 6540
Infection control: Minimizing the acquisition and transmission of infectious agents
Activities:
• Isolate persons exposed to communicable disease.
• Wash hands before and after each patient-care activity.
• Ensure appropriate wound care technique.
Nursing Outcomes Classification (NOC)
NOC, which measures the effects of nursing care, is the effort of a group of researchers working at the University of Iowa. These researchers have developed a standardized system with an organized structure to name and measure nursing-sensitive patient outcomes. Identification of outcomes that are responsive to nursing care is important work for nursing, especially in connection with efforts to contain costs and establish best practices ( Moorhead et al., 2013 ). There are currently 385 outcomes with accompanying definitions, measurement standards, indicators, and references ( Moorhead et al., 2013 ).
The NOC outcomes use brief phrases to describe the result of nursing care. Indicators are given as subheadings for each outcome. These indicators use a measurement scale to evaluate the degree of outcome attainment. An example of an NOC outcome with 1 of the possible 19 indicators follows. The outcome statement and indicator can be described with selected key words from a patient outcome statement (“The patient will demonstrate beginning grief resolution as evidenced by the ability to verbalize reality of loss after nursing interventions”). Also note the coded nature of the outcome and indicators that are used to enhance entry and retrieval of information from a computer database.
• Grief resolution (outcome 1304). Verbalizes reality of loss (indicator 130403). The scale used for this indicator measures from “never demonstrated” to “consistently demonstrated” (1 to 5 scale) ( Moorhead et al., 2013 ).
The nurse should realize that these measurement scales can be used to establish a baseline assessment and then the scale can be applied again during the evaluation phase. Some facilities use these indicators to plan for patient discharge. For example, if the patient does not achieve a 4 or 5 on a scale, then a referral is sometimes necessary.
Role of the Licensed Practical/Vocational Nurse
The LPN/LVN plays a vital role in the collaborative care of the patient. The role of the LPN/LVN in the nursing process may vary from state to state and with different institutions. All practical and vocational student nurses should be knowledgeable regarding their own state's practice. In many states, the registered nurse is responsible for the coordination of care, initiation of the nursing care plan, and evaluation of patient outcomes with the assistance of the LPN/LVN. The LPN/LVN is frequently responsible for providing direct bedside nursing care. This direct care position allows the LPN/LVN to closely observe, prioritize, intervene, and evaluate the care provided to and for the patient. See Box 5-2 for a summary of the role of the LPN/LVN in the nursing process.
Role of the Licensed Practical/Vocational Nurse in the Nursing Process
• Observe and report significant cues to the nurse in charge or to the health care provider.
• Assist with the determination of accurate nursing diagnoses.
• Gather further data to confirm or eliminate problems.
Outcomes Identification and Planning
• Assist with setting priorities.
• Suggest interventions.
• Assist with the development of realistic patient-centered goals and desired patient outcomes.
• Assist with the establishment of priorities.
• Carry out health care provider and planned nursing interventions.
• Evaluate the effectiveness of nursing activities.
• Assist with reevaluation of the patient's health state after nursing interventions.
• Suggest alternative nursing interventions when necessary.
Nursing Diagnoses and Clinical Pathways
To practice in the changing world of health care today, nurses are called on to go beyond performing technical skills and providing direct patient care. Responsibilities include working with outcomes, cost, resources, and other members of the health care team. One way of addressing cost containment issues is through managed care. Managed care refers to health care systems that have control over primary health care services and attempt to trim down health care costs by reducing unnecessary or overlapping services; an emphasis is placed on health promotion, education, and preventative medicine. Case management is one way managed care is achieved in a health care setting. Case management encompasses planning, coordination of care, and patient advocacy in providing quality, cost-effective outcomes for the patient. The case management system of care allows for continuity in care because one person coordinates the plan of care for an individual patient within the health care setting, including discharge planning.
Case management usually depends on the use of clinical pathways. A clinical pathway is a multidisciplinary plan that incorporates evidence-based practice guidelines for high-risk, high-volume, high-cost types of cases while providing for optimal patient outcomes and maximized clinical efficiency. Synonyms for clinical pathways are critical pathways, multidisciplinary action plans, action plans, and care maps. The clinical pathway guides care with coordination of actions from disciplines such as nursing, medicine, pharmacy, social services, dietary therapy, and physical therapy to develop the plan of care. Reduced complications and improved documentation, decreased costs, and decreased time the patient is in the health care setting are potential benefits of the use of clinical pathways ( Rotter et al., 2010 ). When a patient does not achieve the projected outcome, a variance, or exit, is said to have occurred. Variances and exits are examined by members of the multidisciplinary team to determine whether the failure to achieve the outcome was a problem with the system, the provider, or the patient ( Craven and Hirnle, 2012 ). Variance analysis is then used to promote continuous quality improvement. Repetition of variances often leads the health care team to revise a clinical pathway.
Whether the health care facility uses the traditional care plan, clinical pathways, or another system for organizing care, the goal remains the same: efficient care with positive patient outcomes. In addition, the nurse and all health care professionals must be cognizant of cost containment when providing care.
Critical Thinking
“Thinking with a purpose” describes the term critical thinking. Critical thinkers question information, conclusions, and points of view and look beneath the surface. They are logical and fair in their thinking. The skills related to critical thinking are applied to reading, listening, and writing across all subjects. Critical thinking is a complex process, and no single simple definition explains all aspects of critical thinking. Each author who writes about critical thinking has his or her own definition. The National League for Nursing (2000) defines critical thinking for nursing as “a discipline-specific, reflective reasoning process that guides a nurse in generating, implementing, and evaluating approaches for dealing with client care and professional concerns.”
Critical thinking is essential to providing quality nursing care for patients in various situations. One of the first skills a nursing student learns is to take a temperature. The student nurse must choose between obtaining tympanic (ear), oral, rectal, skin, temporal, or axillary measurements. Critical thinking enables the nurse to use the nursing process in choosing the appropriate method. One consideration is the need for accuracy in the results. Also, certain medical or surgical problems may interfere with the accuracy of the reading. If a patient has an ear infection, the results of a tympanic reading may not be accurate. The nurse avoids a rectal thermometer when the patient is recovering from hemorrhoid surgery. If the patient is likely to have a seizure, an oral thermometer is contraindicated because the patient may bite down on the device. The condition of the site to be used should also be taken into consideration. Heavy perspiration often interferes with axillary temperature readings; oral temperature is affected by ingestion of hot or cold beverages. All of these variables are taken into consideration by the student nurse who uses critical thinking skills in the decision-making process.
It is crucial for nurses to not only be able to perform skills (the “doing” of nursing) but also to think about what they are doing. Nurses use a knowledge base to make decisions, generate new ideas, and solve problems. Nursing students add to their knowledge base by studying facts, principles, evidence-based practice guidelines, and theories. Knowledge of psychology, anatomy, physiology, pharmacology, and other related course work helps the student to gain the scientific knowledge base to think critically.
Nurses also must reflect on situations or care given to determine what was effective and what was not effective. Critical thinkers are able to analyze this information and adjust care accordingly, if necessary. Critical thinkers are also able to explore the relationships between concepts and ideas and apply these concepts to unique patient care situations.
To help determine the difference between thinking and critical thinking, consider the following nonclinical situations:
• Situation 1: On the day before classes begin, the student is anxious about getting started and is unsure of her chances of success. She is thinking, “I hope I don't get lost. I hope the teachers are nice. I wonder if I will be able to pass the tests. Will I succeed?” On the day classes begin, she drives to school, finds a parking space, and enters the building to locate her classroom.
• Situation 2: On the day before classes begin, the student is anxious about getting started and is unsure of her chances of success. She is thinking, “I will drive to the school so I can judge how much time to allow for travel. I want to go early and locate my classroom today so I will have an easier time tomorrow. Maybe I can get some course materials early so I can organize my notebook.”
Both of these situations describe individuals who are thinking. The student in situation 1 is experiencing a mental activity, but it is aimless and without purpose. The student in situation 2 has recognized the need to gain control and get organized. This student is beginning to think critically and with a purpose, which is to decrease the anxiety associated with her first day of class.
The following clinical situations provide examples of some aspects of critical thinking at the bedside.
• Situation 1: The nurse was caring for a patient with chronic obstructive pulmonary disease and peripheral vascular disease. During the assessment, the nurse used a pulse oximeter on the patient's finger to measure the patient's oxygen saturation level. The measurement yielded an oxygen saturation of 87%. The assessment revealed clear lung sounds, no difficulty with respirations or reports of shortness of breath, capillary refill <2 seconds, and extremities cool to the touch. The nurse demonstrates critical thinking skills by realizing that the assessment does not match the oxygen saturation measurement and decides to recheck the oxygen saturation level with the earlobe probe because the patient's hands were cool to the touch. The oxygen saturation level with the earlobe probe was 93%, which matched the assessment findings. With use of critical thinking skills, the nurse was able to make comparisons between the assessment findings and the oxygen saturation level and problem solve by determining how to address the situation.
• Situation 2: A patient with diabetes was admitted to the hospital for a bladder infection. At the change of shift, the oncoming nurse entered the room to perform an assessment. The nurse noted that the patient was unresponsive. The nurse demonstrates critical thinking skills by realizing the patient is most likely experiencing one of two problems: hypoglycemia or hyperglycemia. The nurse first performed a quick “ABC” assessment and determined that the patient's airway was open, the patient was breathing, and the patient's heart was circulating blood. Then, because the patient was admitted with an infection, the nurse suspected that the patient was experiencing a rise in blood glucose levels, or hyperglycemia. He obtained a finger stick blood sugar reading of 346. The nurse also noted that the patient's skin was warm, dry, and flushed. The patient's respirations were deep, and her breath smelled “fruity.” The nurse quickly called the physician to report these findings and anticipated receiving orders to give the patient more insulin. Critical thinking skills enabled the nurse to deal with this patient situation appropriately.
Anticipating questions, asking an expert, and asking why are all examples of other strategies to improve critical thinking. It often takes a while to become comfortable with these ideas, but doing so helps the student or nurse gain insight into one's thinking. Hearing others think aloud may also help the student learn how other people reason. The student should take advantage of every learning opportunity and realize that every experience, mistake, and encounter is a potential learning opportunity.
- High School
- You don't have any recent items yet.
- You don't have any courses yet.
- You don't have any books yet.
- You don't have any Studylists yet.
- Information
HA1 Test 1 study questions
Advanced physical assessment (n671), samuel merritt university, recommended for you, students also viewed.
- Intro to history taking and PE in Dermatology
- 671 Chest and Lungs reading notes
- N671 Sample SOAP Note 2023-1
- W6 Case Presentation
- Administering Pediatric Medications
- Acute Coronary Syndrome
Related documents
- Ch 24 critical care calculations
- CH .4 - Conclusion: Advanced assessment skill is the means to an accurate interpretation
- 01 General Survey - Lecture notes 1
- Notes from BOX 23-17 muscoskeletal
- Chapter 12 part 2 aca - quiz notes
- #6 Differential Diagnosis Table
Preview text
Critical thinking.
The use of critical thinking skills during the assessment phase of the nursing process ensures that the nurse
a. Completes a comprehensive database.
b. Identifies pertinent nursing diagnoses.
c. Intervenes based on patient goals and priorities of care.
d. Determines whether outcomes have been achieved.
The assessment phase of the nursing process involves data collection to complete a thorough patient database. Identifying nursing diagnoses occurs during the diagnosis phase. The nurse carries out interventions during the implementation phase, and determining whether outcomes have been achieved takes place during the evaluation phase of the nursing process.
Which of the following is a nursing intervention?
a. The patient will ambulate in the hallway twice this shift using crutches correctly.
b. Impaired physical mobility related to inability to bear weight on right leg
c. Provide assistance while the patient walks in the hallway twice this shift with crutches.
d. The patient is unable to bear weight on right lower extremity.
Providing assistance to a patient who is ambulating is a nursing intervention. The statement, “The patient will ambulate in the hallway twice this shift using crutches correctly” is a patient goal. Impaired physical mobility is a nursing diagnosis. The statement that the patient is unable to bear weight and ambulate can be included with assessment data and is a defining characteristic for the diagnosis of Impaired physical mobility.
In which step of the nursing process does the nurse provide nursing care interventions to patients?
a. Assessment
b. Planning
c. Implementation
A nursing database includes a physical examination. Orders are included in the order section of the patient’s chart. The nurse reviews the current literature in the implementation phase of the nursing process to determine evidence-based actions, and the health care provider is responsible for ordering medications. Medication orders are usually written after the database is completed.
Which of the following are examples of subjective data? (Select all that apply.)
a. Patient describing excitement about discharge
b. Patient’s wound appearance
c. Patient’s expression of fear regarding upcoming surgery
d. Patient pacing the floor while awaiting test results
e. Patient’s temperature
Subjective data include patient’s feelings, perceptions, and reported symptoms. Expressing feelings such as excitement or fear is an example of subjective data. Objective data are observations or measurements of a patient’s health status. In this question, the appearance of the wound and the patient’s temperature are objective data. Pacing is an observable patient behavior and is also considered objective data.
Components of a nursing health history include
a. Current treatment orders.
b. Nurse’s concerns.
c. Nurse’s goals for the patient.
d. Patient expectations.
Components of a nursing health history include physical examination findings, patient expectations, environmental history, and diagnostic data. Current treatment orders are located under the Orders section in the patient’s chart and are not a part of the nursing health history. Patient concerns, not nurse’s concerns, are included in the database. Goals that are mutually established, not nurse’s goals, are part of the nursing care plan.
c. Convection.
d. Evaporation.
Applying an ice pack or bathing a patient with a cool cloth increases conductive heat loss. Radiation is the transfer of heat from the surface of one object to the surface of another without direct contact between the two. Evaporation is the transfer of heat energy when a liquid is changed to a gas. Convection is the transfer of heat away from the body by air movement.
The patient is restless with a temperature of 102° F (39° C). One of the first things the nurse should do is
a. Place the patient on oxygen.
b. Restrict fluid intake.
c. Increase patient activity.
d. Increase patient’s metabolic rate.
During a fever, cellular metabolism increases and oxygen consumption rises. Myocardial hypoxia produces angina. Cerebral hypoxia produces confusion. Interventions during a fever include oxygen therapy. Dehydration is a serious problem through increased respiration and diaphoresis. The patient is at risk for fluid volume deficit. Fluids should not be restricted. Increasing activity would increase the metabolic rate further, which would not be advisable.
The patient requires temperatures to be taken every two hours. Which of the following cannot be delegated to nursing assistive personnel?
a. Selecting appropriate route and device
b. Obtaining temperature measurement at ordered frequency
c. Being aware of the usual values for the patient
d. Assessing changes in body temperature
The nurse is responsible for assessing changes in body temperature. The nurse instructs nursing assistive personnel to select the appropriate route and device to measure temperature, to obtain temperature measurement at ordered frequency, and to be aware of the usual values for the patient.
The patient is being admitted to the emergency department following a motor vehicle accident. His jaw is broken, and he has several broken teeth. He is ashen, and his skin is
c. Understand that respirations are estimated to save time.
d. Not be touched until the entire process is finished.
Do not let a patient know that respirations are being assessed. A patient who is aware of the assessment can alter the rate and depth of breathing. Respirations are the easiest of all vital signs to assess, but they are often the most haphazardly measured. Do not estimate respirations. Accurate measurement requires observation and palpation of chest wall movement.
The patient’s blood pressure is 140/60. The nurse realizes that this equates to a pulse pressure of
The difference between the systolic pressure and the diastolic pressure is the pulse pressure. For a blood pressure of 140/60, the pulse pressure is 80 (140 – 60 = 80). 140 is the systolic pressure. 60 is the diastolic pressure. 200 is the systolic (140) added to the diastolic (60), but this has no clinical significance.
Of the following values, which value would be considered prehypertension?
a. 98/50 in a 7-year-old child
b. 115/70 in an infant
c. 140/90 in an older adult
d. 120/80 in a middle-aged adult
An adult’s blood pressure tends to rise with advancing age. The optimal blood pressure for a healthy, middle-aged adult is less than 120/80. Values of 120 to 139/80 to 89 mm Hg are considered prehypertension. Blood pressure greater than 140/90 is defined as hypertension. Blood pressure of 98/50 is normal for a child, whereas 115/70 can be normal for an infant.
The incidence of hypertension is greater in which of the following?
a. Non-Hispanic Caucasians
Smoking immediately increases BP, and this increase lasts up to 15 minutes. Caffeine increases BP for up to 3 hours. Both affect a patient’s blood pressure. The patient should rest at least 5 minutes before BP is measured.
Of the following patients, which one is the best candidate to have his temperature taken orally?
a. A 27-year-old postoperative patient with an elevated temperature
b. A teenage boy who has just returned from outside “for a smoke”
c. An 87-year-old confused male suspected of hypothermia
d. A 20-year-old male with a history of epilepsy
An elevated temperature needs to be evaluated, and there is no contraindication in this patient. Ingestion of hot/cold fluids or foods, smoking, or receiving oxygen by mask/cannula can require delays in taking oral temperature. Oral temperatures are not taken for patients who have had oral surgery, trauma, history of epilepsy, or shaking chills, nor for infants, small children, or confused patients.
When temperature assessment is required, which of the following cannot be delegated to nursing assistive personnel?
a. Temperature measurement
b. Assessment of changes in body temperature
c. Selection of appropriate route and device
d. Consideration of factors that falsely raise temperature
The skill of temperature measurement can be delegated. The nurse is responsible for assessing changes in body temperature. The nurse instructs nursing assistive personnel to select the appropriate route and device to measure temperature and to consider specific factors that falsely raise or lower temperature.
The nursing assistive person is taking vital signs and reports that a patient’s blood pressure is abnormally low. The nurse should
a. Have the nursing assistive person retake the blood pressure.
e. Pulmonary artery
Intensive care units use the core temperatures of the pulmonary artery, esophagus, and urinary bladder. Because the tympanic membrane shares the same arterial blood supply as the hypothalamus, the tympanic temperature is a core temperature. Oral, rectal, axillary, and skin temperature sites rely on effective blood circulation at the measurement site.
The patient has new-onset restlessness and confusion. His pulse rate is elevated, as is his respiratory rate. His oxygen saturation, however, is 94% according to the portable pulse oximeter. The nurse ignores the oximeter reading and calls the physician to obtain an order for an arterial blood gas (ABG). The nurse does this because many things can cause inaccurate pulse oximetry readings, including which of the following? (Select all that apply.)
a. O2 saturations (SaO2) >70%
b. Carbon monoxide inhalation
c. Nail polish
d. Hypothermia at the assessment site
e. Intravascular dyes
ANS: B, C, D, E
Inaccurate pulse oximetry readings can be caused by outside light sources, carbon monoxide (caused by smoke inhalation or poisoning), patient motion, jaundice, intravascular dyes (methylene blue), nail polish, artificial nails, metal studs, or dark skin. Other factors include peripheral vascular disease (atherosclerosis), hypothermia at the assessment site, pharmacological vasoconstrictors (e., epinephrine), low cardiac output, hypotension, peripheral edema, and tight probes.
The nurse is assessing the patient and his family for probable familial causes of the patient’s hypertension. The nurse begins by analyzing the patient’s personal history, as well as family history and current lifestyle situation. Which of the following issues would be considered risk factors? (Select all that apply.)
b. Cigarette smoking
c. Recent weight loss
d. Heavy alcohol consumption
Xerosis is the term used to describe skin that is excessively dry. Pruritus refers to itching, alopecia refers to hair loss, and seborrhea refers to oily skin.
The nurse is examining a patient who tells the nurse, “I sure sweat a lot, especially on my face and feet but it doesn’t have an odor.” The nurse knows that this condition could be related to:
a. Eccrine glands.
b. Apocrine glands.
c. Disorder of the stratum corneum.
d. Disorder of the stratum germinativum.
The eccrine glands are coiled tubules that directly open onto the skin surface and produce a dilute saline solution called sweat . Apocrine glands are primarily located in the axillae, anogenital area, nipples, and naval area and mix with bacterial flora to produce the characteristic musky body odor. The patient’s statement is not related to disorders of the stratum corneum or the stratum germinativum.
The nurse educator is preparing an education module for the nursing staff on the epidermal layer of skin. Which of these statements would be included in the module? The epidermis is:
a. Highly vascular.
b. Thick and tough.
c. Thin and nonstratified.
d. Replaced every 4 weeks.
- Multiple Choice
Course : Advanced Physical Assessment (N671)
University : samuel merritt university.

- Discover more from: Advanced Physical Assessment N671 Samuel Merritt University 24 Documents Go to course
- More from: Advanced Physical Assessment N671 Samuel Merritt University 24 Documents Go to course

IMAGES