- Open access
- Published: 14 November 2024

The last decade of air pollution epidemiology and the challenges of quantitative risk assessment
- Francesco Forastiere 1 , 2 ,
- Hans Orru 3 , 4 ,
- Michal Krzyzanowski 2 &
- Joseph V. Spadaro 5
Environmental Health volume 23 , Article number: 98 ( 2024 ) Cite this article
Metrics details
Epidemiologic research and quantitative risk assessment play a crucial role in transferring fundamental scientific knowledge to policymakers so they can take action to reduce the burden of ambient air pollution. This commentary addresses several challenges in quantitative risk assessment of air pollution that require close attention. The background to this discussion provides a summary of and conclusions from the epidemiological evidence on ambient air pollution and health outcomes accumulated since the 1990s. We focus on identifying relevant exposure-health outcome pairs, the associated concentration-response functions to be applied in a risk assessment, and several caveats in their application. We propose a structured and comprehensive framework for assessing the evidence levels associated with each exposure-health outcome pair within a health impact assessment context. Specific issues regarding the use of global or regional concentration-response functions, their shape, and the range of applicability are discussed.
Peer Review reports
Introduction
It is widely acknowledged that air pollution is one of the most significant environmental risks to health globally [ 76 ]. The updated World Health Organization (WHO) air quality guidelines (AQGs), published in September 2021, underscore the urgent need for immediate action to combat the adverse effects of pollutants such as fine particulate matter (PM 2.5 ), nitrogen dioxide (NO 2 ), and ozone (O 3 ) on public health and the environment [ 85 ]. Modern quantitative health risk assessment (HRA) plays a crucial role in transferring fundamental scientific knowledge to policymakers, empowering them to take action to reduce the burden of air pollution, and evaluating the health benefits of interventions. Rigaud et al.‘s recent contribution to this Journal (2024) provides an extensive overview of HRA methods and offers excellent examples. This commentary addresses some of the challenges in quantitative risk assessment of ambient air pollution that require close attention, especially considering the lessons learnt from the recently completed WHO project Estimating the Morbidity from Air Pollution and its Economic Costs (EMAPEC) [ 26 ]. A summary of the epidemiological evidence on air pollution and health outcomes accumulated over the last decades provides a background to this discussion.
Early epidemiological studies on short and long-term exposure
During the early stages of research in environmental epidemiology, the identification of an association between short (on the scale of hours to days) and long-term exposure to air pollution (on the scale of months to years) and various adverse health outcomes, particularly the impact on mortality, laid the foundation for quantifying the attributable burden of pollution. Short-term observational studies began gaining prominence in the late 1980s and early 1990s [ 6 , 67 , 68 ]. These studies were driven by growing concerns about air quality and its impact on public health, particularly in urban areas with significant air pollution levels. Throughout the 1990s, these short-term studies expanded, particularly with the use of time-series analyses, which examined daily fluctuations in air pollution levels and corresponding health outcomes, such as hospital admissions and mortality, in several cities [ 39 ]. These studies provided compelling evidence of the acute health effects of air pollution. Regarding long-term exposure, a seminal air pollution research paper published in 1993, the ‘Six Cities’ cohort study in the United States [ 21 ], demonstrated a link between mortality and long-term exposure to PM 2.5 . This discovery gained further support in 1995 after the analysis of the health data from the American Cancer Society (ACS), a cohort of approximately half a million residents from across the United States [ 61 ], which revealed an almost linear increase in mortality risk across the entire range of observed PM 2.5 annual mean concentrations (from 10 to 30 µg/m³) in urban background areas. A subsequent 2002 analysis of cardiovascular and lung cancer mortality with exposure to PM 2.5 [ 61 ] of the same ACS cohort triggered research into the biological mechanisms responsible for these effects. Note that the statistical methodology used in the ACS study was advanced and considered several individual potential confounders. The potential spatial autocorrelation due to missing or mismeasured risk factors spatially correlated with air pollution was addressed in the statistical model by incorporating a spatially-varying random-effects component to correct for autocorrelation, a practice that has been in common use in subsequent years. This overall evidence led to the formulation of the first global air quality guidelines by WHO in 2005 [ 84 ].
The first decade of the 21st century witnessed a convergence of epidemiological studies, controlled human exposure trials, and animal experiments. Epidemiological studies in humans (both on short- and long-term exposures) have provided refined estimates of environmental risks, with evidence suggesting that associations between PM and health outcomes are present even at ambient concentrations below the WHO air quality guideline levels. Mechanistic studies in animals and humans have provided a framework for understanding the pathways by which air pollution exposure may predispose individuals to health effects. This interdisciplinary approach deepened the understanding of the cardiovascular effects of PM exposure and confirmed the causality of PM 2.5 effects [ 5 ]. Results from cohort studies during this period further strengthened the epidemiological evidence of the effects of PM 2.5 and NO 2 on all-cause (in many cases non-accidental or natural mortality) and cause-specific mortality, and the development (incidence) of selected cardiovascular and respiratory diseases. Evidence from European cohorts, such as the collaborative ESCAPE study [ 1 ], confirmed earlier findings reported in North American studies. In addition, epidemiological studies began using administrative databases, including census and mortality registries, which enabled large-scale data pooling of millions of individuals for a period extending a decade or longer, as exemplified by the observational study of the 2.1 million people from Canada [ 16 ] and 1.3 million residents of Rome [ 10 ]. Exposure to ultrafine particles has been gaining attention because of the potential translocation from the lungs to the circulatory system and the possible effects on the heart [ 35 , 55 ].
The last decade of air pollution epidemiology
Several studies based on “administrative cohorts” have been published in the last decade [ 7 , 11 , 17 , 19 , 25 ]. Cohorts based on administrative data have several advantages over “traditional cohorts” in investigating air pollution risks, namely their size, including millions of people, their representativeness of the general population, including different demographic and socioeconomic groups, enhancing the generalizability of findings, data collected over many years that allow for an extended follow-up. These advantages make administrative cohorts a valuable resource for large-scale, population-based research. However, the lack of detailed individual-level data on lifestyle factors is a drawback. This limitation has been partially overcome using area-based indicators to represent individual data, for example, area-based socioeconomic status (SES) as a surrogate for individual SES. In addition, several cohorts have used “indirect adjustment” for individual confounders that employs an ancillary database that matches the demographic characteristics of the original cohort and contains information on both the individual factors (that are missing in the original cohort) and air pollution exposure data [ 24 , 73 ].
While most initial cohort studies were conducted in North America and Europe, areas in which populations were exposed to low or medium levels of PM 2.5 concentration (< 30 µg/m 3 ), the last decade has seen a notable expansion of epidemiological studies in regions with higher ambient air pollution levels, particularly in China and Korea [ 43 , 46 ], where observed PM exposures were typically 2 to 4 times higher than in previous studies. The newer studies accounted for various confounders that may influence mortality, such as diet, lifestyle, and climate. A meta-analysis published in 2020, specifically designed to support the work in updating the WHO AQGs, considered the findings from over 100 cohort studies that examined the link between PM 10 or PM 2.5 and all-cause and cause-specific premature mortality [ 12 ]. This latter meta-analysis has been recently updated to consider several studies published in the last few years [ 57 ].
The literature on air pollution and its impact on health has witnessed significant methodological advancements over the past decade. Firstly, the modelling of air pollution exposure has undergone substantial enhancements. Early evaluations at the population level relied primarily on fixed monitors, which, while providing benchmark standards, were limited in assessing small-scale exposure variability due to geographical constraints. To address this issue, recent air pollution exposure assessments have incorporated various indicator variables to measure fine-scale exposures, including land-use regression variables to better capture a subject’s proximity to roads and industrial facilities, as well as using remote sensed satellite measurements with appropriate downscaling, and results of chemical transport model (CTM) estimates of PM 2.5 and NO 2 concentrations [ 18 , 20 , 30 , 80 ]. These enhancements have broadened the geographical coverage of exposures, especially in areas lacking physical monitoring stations, to provide highly spatially resolved concentration maps in both urban and rural settings, with a typical resolution scale of one kilometre, or less (100 m) in some cases. This spatial precision allows for addressing issues related to community exposure disparities and pinpointing local pollution hotspots. A recent application of these models in the US over the past decade revealed an increase in racial and ethnic relative disparities in PM 2.5 -related mortality and NO 2 -related pediatric asthma despite overall declines in public health effects associated with these pollutants [ 40 ].
Secondly, notable systemic consequences of air pollution have been identified, leading to additional adverse health outcomes. While respiratory and cardiovascular conditions have traditionally been linked to air pollution, recent studies suggest potential associations with neurological conditions (such as Parkinson’s and Alzheimer’s disease), diabetes, various types of cancer (in addition to lung cancer, which was studied long before), neurobehavioral development issues in children, mental disorders, and perinatal health [ 75 ]. Ongoing research explores the mechanistic pathways connecting environmental exposure to these health outcomes, highlighting the potential role of air pollution-induced inflammatory responses and the persistent generation of reactive oxygen radicals [ 53 ]. Moreover, investigations into the intake of ultrafine particles and their passage across biological barriers, including the circulatory system, blood-brain barrier, and placental barrier, have spurred additional insights. Ultrafine particles can reach all organs of the body, and potentially accumulate at sites of disease [ 66 ]. Epidemiological research on ultrafine particles is complicated because of the difficulties in exposure assessment, but increasing evidence in both North America and Europe suggests important health impacts [ 56 ].
Most recently, three large-scale studies funded by the Health Effects Institute (HEI) have investigated the health effects of low-level air pollution exposure in Canada, the United States, and Europe. These studies are the “Mortality Air Pollution Associations in Low Exposure Environments” (MAPLE) Canadian study by Brauer et al. [ 3 ], the USA Medicare study by Dominici et al. [ 23 ], and the Effects of Low-Level Air Pollution: A Study in Europe (ELAPSE) by Brunekreef et al. [ 7 ]. These studies included millions of participants, employed advanced exposure assessment techniques, and used comprehensive statistical analyses with innovative approaches. All three studies reported statistically significant positive associations between long-term PM 2.5 exposure and mortality risks in nationally representative administrative cohorts. The hazard ratios (HR) and 95% confidence intervals (CI) associated with an increase in PM 2.5 exposure of 5 µg/m³ and mortality from natural causes were as follows: 1.041 (95%CI 1.036, 1.047) in the Canadian Census Health and Environment Cohorts (CanCHEC) in MAPLE; 1.032 (95%CI 1.029, 1.036) in the USA Medicare cohort; and 1.053 (95%CI 1.021, 1.085) in the six ELAPSE administrative cohorts. Note that the USA Medicare cohort used the all-cause mortality (i.e. including accidental deaths) in the cohort older than 65 years old. The pooled analysis of the three studies provided by Chen et al. [ 11 ] suggests an increasing risk starting from the lowest observed exposure level (3.7 µg/m 3 ). The ELAPSE study in Europe, using pooled data from several traditional cohorts [ 74 ], also explored several morbidity outcomes, including myocardial infarction and stroke [ 88 ], asthma in adults [ 51 ], COPD [ 50 ], and lung cancer [ 37 ].
The insights derived from these “low-level studies” [ 2 ] have informed the WHO in its work on the 2021 AQGs and played a crucial role in shaping recent regulations on PM 2.5 in both the USA and Europe. Notably, the US Environmental Protection Agency’s decision to lower the National Ambient Air Quality Standards (NAAQS) for fine particulate matter air pollution (PM 2.5 ) in urban background areas from 12 to 9 µg/m 3 in 2024 Footnote 1 , and the European Parliament’s decision to approve the revision of the Ambient Air Quality Directive to reduce the annual limit value for PM 2.5 from 25 µg/m 3 to 10 µg/m 3 in 2030 Footnote 2 are outcomes directly influenced by the information provided by these studies.
Global burden of Disease (GBD) studies
The first in a series of GBD studies was published in 1993, and detailed the state of global health for eight world regions as of 1990 [ 54 ]. The comparative risk assessment covered 106 illnesses and ten risk factors. The study of morbidity and mortality was an effort to characterise the burden of disease using a standardised approach. The risk factors included behavioural, occupational, metabolic, and environmental factors, including air pollution.
In 2007, a new study (GBD 2010) was funded by the Bill & Melinda Gates Foundation (BMGF) [ 48 ]. An important innovation of the air pollution health impact assessment methodology in GBD 2010 was the introduction of the integrated exposure-response functions (IERs) for cause-specific mortality. Since PM 2.5 levels in many regions of the world exceed the levels observed in epidemiological studies, the IERs combined population exposure to various sources of combustion particulates, such as outdoor and indoor air pollution, environmental tobacco smoke (second-hand smoke), and active smoking. The health outcomes included diseases of the cardiovascular and respiratory systems, and lung cancer. The IERs, which have changed considerably over the years [ 58 ], have a non-linear shape, and they increase monotonically with concentration, starting from a “counterfactual concentration”, also known as the theoretical minimum risk exposure level (TMREL), which represents the lowest exposure across the available epidemiological studies with the lowest credible level for the existence of a health burden. In principle, the TMREL is uncertain, and might vary by location and demographic characteristics. Since 2015, the GBD study has used a TMREL for PM 2.5 based on a uniform distribution over the range of 2.4 to 5.9 µg/m³.
Since GBD 2010, several revisions of the GBD have been published, with the most recent update in 2024 and identified as GBD 2021 [ 27 ]. Each iteration has contributed to methodological innovations and the development of more robust techniques for exposure assessment, data synthesis, analysis, and interpretation. Furthermore, with each iteration of GBD, the level of detail of the results has improved, including added diseases and risk factors, geographical stratification, and specification of health effects by age. The latest GBD 2021 study provides results (e.g. attributable deaths and disability-adjusted life years (DALYs)) for 88 risk factors across 204 countries and 811 subnational areas for the historical period between 1990 and 2021. Forecasted estimates for 2050 are also available [ 28 ]. The current calculations for PM are based on an updated risk function, estimated in an analysis of epidemiological studies of the effect of particulate air pollution from outdoor and indoor sources, with no inputs from studies on environmental tobacco smoke or active smoking. According to the GBD 2021 study, the global mortality attributed to PM 2.5 ambient air pollution in 2021 was 4.7 2 (95% Uncertainty Interval: 3.48; 5.80) million deaths, including 4.51 million deaths among the population over 25 years (97 deaths per 100,000 in the population 25+, or 7.9% of natural deaths). Air pollution has increased its importance compared to other leading risk factors like high systolic blood pressure, smoking, and high fasting plasma glucose. Among all risk factors, particulate matter pollution (indoor plus outdoor exposure) contributed the largest share of global DALYs (approx. 8%), and the second largest share of global deaths (approx. 12%) in 2021. ( https://vizhub.healthdata.org/gbd-compare/ )
The benefits of quantitative risk assessment
Briggs [ 4 ] focused on the evolution from risk assessment of single exposures to the more complex need to predict “the health-related impacts of policies and other interventions that affect the environment in ways that take account of the complexities, interdependencies and uncertainties of the real world” in an integrated Health Impact Assessment (HIA). Therefore, risk assessment is traditionally focused on single exposures or events while HIA takes a broad concept of both the environment and health [ 86 ]. Rigaud et al. [ 64 ] emphasize that there is a terminology issue, and the term “quantitative risk assessment” represents a systematic approach that uses the same methodology to evaluate and present the potential health impacts of single exposures, projects, policies, or programs with the aim of protecting public health. For this reason, we will use the term quantitative risk assessment or health impact assessment interchangeably. Quantitative risk assessment has been crucial in formulating air pollution guidelines and regulatory criteria to safeguard human health. Recent initiatives by regulatory bodies like the US Environmental Protection Agency and the European Parliament indicated above have underscored the significance of quantitative risk assessment in shaping appropriate regulatory measures. In both the USA and EU, the CRFs derived from large epidemiological studies are used to estimate the health impacts of air pollution. In setting air quality standards, a cost-benefit analysis is conducted where benefits (e.g. lives saved) are monetized using value of statistical life (VSL) and compared to the costs of achieving lower air pollution levels through regulations. Undoubtedly, the total number of deaths attributable to exposure in a population speaks more clearly than relative risks or hazard ratios, providing an indication of the actual number of cases that a population has to deal with because of the exposure. The number of cases/deaths serves as a cornerstone for understanding the risks associated with exposure to major air pollutants. It is the basis for an economic assessment to identify the cost efficiency of the proposed interventions, and to guide the implementation of measures to safeguard public well-being. Rigaud et al. [ 64 ] provide valuable references for historical context and methodological insights, drawing from works such as those by Harris-Roxas et al. [ 32 ] and Briggs [ 4 ], as well as resources like the WHO document “Health risk assessment of air pollution – general principles” [ 86 ].
Approaches like the Global Burden of Disease (GBD) [ 27 ] and those adopted by the European Environment Agency (EEA) [ 71 ] have contributed significantly to this field. For the specific situation of Europe, Khomenko et al. [ 41 , 42 ] conducted studies estimating the proportion of annual deaths due to air pollution in numerous cities across Europe. Their work also evaluates spatial and sector-specific emission contributions to ambient air pollution, and assesses the effects of source-specific reductions in pollutants on mortality in European cities.
Navigating new challenges in quantitative risk assessment
The basic approach in a Health Impact Assessment (HIA) is well-established [ 87 ]. It uses exposure data (either measured or modelled pollutant concentrations), baseline health data (e.g. mortality/morbidity data from registers), and concentration-response functions (CRF) from epidemiological studies to quantify the health effects in terms of premature death and/or morbidity. Rigaud et al. [ 64 ] have underscored several important challenges that we will specifically address in this discussion, e.g., issues about identifying pollution/health outcome pairs, the associated concentration-response functions, and their application in an HIA. Other pertinent issues will be reserved for future deliberations, such as estimates of vulnerable populations, exposure data, baseline morbidity and mortality data, methodological uncertainties, and counterfactual values.
Traditionally, air pollution HIA have focused on all-cause (non-accidental or natural mortality) and cause-specific mortality based on CRFs derived from systematic literature reviews and meta-analyses, which synthesize the epidemiological evidence on the health effects of air pollution. While the most appropriate CRFs for the relationship between long-term exposure to PM 2.5 /NO 2 and mortality are currently under discussion [ 36 ], the ongoing work in the revision of the WHO-HRAPIE project (Health risks of air pollution in Europe) [ 34 ] is actively addressing this aspect by carrying out updated meta-analyses on CRFs [ 56 ]. Earlier, morbidity outcomes reflecting the multiplicity of air pollutant effects on various organs have often been overlooked [ 75 ], leading to an underestimation of the full burden of air pollution. When considering societal costs, chronic conditions such as chronic obstructive pulmonary disease (COPD) or dementia place a significant burden on social welfare and healthcare systems. The EMAPEC project coordinated by WHO has proposed CRFs for the incidence of various diseases related to long-term exposure to PM 2.5 and NO 2 [ 26 ]. The selection was made after reviewing the empirical epidemiological evidence and screening for acceptable systematic review/meta-analysis quality to propose appropriate CRFs.
The most recent studies, based on very large populations and advanced air pollution modelling methods, go beyond using a mass concentration of PM 2.5 as a health risk determinant and explore the associations of selected PM 2.5 chemical components with mortality [ 31 , 83 ]. Confirmation of these associations, including the relevant CRFs, in further studies, especially from regions with different pollution levels and sources, would create new opportunities for risk assessment, allowing better impact assessment of source- (and component-) specific PM 2.5 reduction.
Ongoing research is anticipated to yield further proposals for pollutant/outcome pairs in the future. This multiplicity of potential CRFs makes Rigaud’s open question regarding “ proposing a formal approach to the quantitative handling of the level of evidence regarding each exposure-health outcome pair ” very relevant and timely. Based on insights gained in EMAPEC, we address it in a proposed framework illustrated in Fig. 1 . This framework aims to provide a structured and comprehensive approach to assessing the evidence levels associated with each exposure-health outcome pair in an HIA or cost-benefit analysis (CBA) context.

Schematic representation of the steps in choosing the appropriate concentration-response function (CRF)
Is causality a necessary condition ?
Conducting an HIA requires a causality determination of the health effects associated with the specific exposure. It would be difficult to recommend a particular risk assessment function if the qualitative relationship between exposure and disease has not passed the hazard identification steps, which consider the entirety of human, toxicological and mechanistic evidence. In other words, we must be certain that a specific exposure is causally related to a particular outcome before quantifying the impact. In the EMAPEC project, the decision on hazard identification was taken based on the determination from the US Environmental Protection Agency’s Integrated Science Assessment (EPA ISA) for NO 2 [ 77 ] and PM 2.5 [ 78 ]. Only pollutant/outcome pairs categorised as “ Causal” or “Likely to be causal ” according to the US EPA ISA methodology [ 59 ] were considered (this is schematically summarised in the left part of Fig. 1 . The sole exception was for the relationship between PM 2.5 and type II diabetes, which was not considered as “ Causal” or “Likely to be causal ” in the US EPA ISA 2019, but its inclusion in the list of relevant health outcomes was supported, in our view, by independent new epidemiological and toxicological evidence [ 46 , 47 ].
It should be acknowledged that relying solely on the US EPA ISA is a conservative approach, especially if the assessment is outdated (as in the case of NO 2, which was last reviewed in 2016; in this specific case, insufficient adjustment for other pollutants was a major reason for giving a low causality rating for this pollutant). Choosing causality as a prerequisite, especially when a causality assessment has not already been done, might lead to a potential underestimation of the health burden or impact. We aim to avoid neglecting emerging hazards due to insufficient data for a comprehensive impact assessment, as Rigaud et al. [ 63 , 64 ] highlighted, we do not want to “ leave emerging hazards by the roadside ”.
A possible solution is to compile two lists of CRFs to be used in an HIA, one that contains the CRFs for which the causality link has been well established (Core list) and one that includes CRFs for which the causality assessment has yet to be established, but the emerging evidence of an association is reasonably strong to consider the exposure-outcome pair in a sensitivity analyses (Non-Core list) (Fig. 1 ). The right part of Fig. 1 illustrates the situation when there is a causality evaluation less than “Likely to be causal” (e.g. “Suggestive”), including situations where the causality evaluation has not been done. In such cases, the decision to proceed is influenced by the information gathered from epidemiological studies, and the supporting evidence from toxicological and mechanistic studies. While the relationship between PM 2.5 and diabetes is well-supported in the published literature [ 62 , 63 ], for other illnesses reaching a decision could be more challenging as it would require careful consideration and justification for inclusion by experts using multiple sources of information. A guiding principle in this respect is a critical evaluation of the quality of the available epidemiologic studies and the information they provide. Following the general framework for the design and analysis of aetiologic studies [ 52 ], the likelihood of finding evidence of causality in air pollution research is higher when more scientifically rigorous decisions are taken [ 22 ]. An in-depth evaluation of design choices, such as the exposure levels being compared, appropriate comparison group, and care to control confounding, should be used to determine the evidence of causation. Triangulation can be useful as it involves considering different studies that reach or do not reach the same conclusion about the risk association, but that are potentially affected by different biases (or the same bias to different extents). In other words, we can justify the need to proceed with the assessment if the epidemiological studies are of good design, are robust to covariate adjustment, and the cross-study results are consistent. The presence of information from toxicology and the mechanism of action is important, but it should not be a prerequisite. For instance, in the IARC strategy [ 65 ], “sufficient” evidence from human observational investigations (e.g. epidemiological studies) is enough in categorising a substance as being carcinogenic to humans (Group 1).
Pollutant/outcome pairs from this part of the evaluation enter the “Non-Core” list rather than the “Core” list and might be applied in a sensitivity analysis. The “Non-Core” category may include pollutant/outcome pairs with varying levels of evidence supporting causality, allowing for a nuanced approach to assessing health effects. Further, a pollutant/outcome pair could migrate from the “Non-Core” list to the “Core” list once a formal level of evidence of causality has been established based, for example, on the US EPA or other authoritative agencies evaluation. In the EMAPEC work, a Core CRF list (list A) and a Non-Core CRF list (List B+) were suggested. For PM 2.5, the Core list (List A) included incidence of asthma in children, COPD, ischemic heart disease events, stroke, hypertension, and lung cancer. For NO 2 , a Core list (list A) was provided for the incidence of asthma in children, asthma in adults, and acute respiratory infections in children. Three outcomes (diabetes, dementia, and autism spectrum disorders) in relation to PM 2.5 were added to the list for sensitivity analysis (Non-Core, list B+).
Quality of Systematic Reviews and Meta-analyses providing CRF
To provide a reliable CRF, it is imperative to gather evidence from human studies, which is typically achieved through systematic reviews (SRs) and meta-analyses. Situations may arise where no SRs exist or existing reviews on a given health effect are outdated. In such cases, the only viable solution is to initiate a new SR, carefully considering the required human and time resources to do the work. Luckily, recent SRs are often readily available, and two primary options exist:
New SR based on a comprehensive selection of individual studies from all available SRs. One option is to select all individual studies from all available SRs and then use this collective experience to perform a new SR. This approach leverages the groundwork laid by previous SRs, streamlining the search, scrutiny, and selection of primary studies. However, the subsequent work would involve conducting a new SR to synthesise the entirety of the collected information.
Quality evaluation and selection of SRs . Alternatively, as undertaken in the EMAPEC project, one can assess the quality of all recently available SRs, and then choose those with the highest quality for further consideration. A meticulous evaluation of systematic reviews is crucial for extracting reliable CRFs. Based on the EMAPEC experience, this was achieved by considering various aspects, including literature search, inclusion criteria, data extraction, statistical analysis, and bias assessment [ 26 , 69 ]).
In both options, verifying the evidence included in the SRs based on original papers is advisable. The experience from EMAPEC shows that mistakes (e.g. the inclusion of studies that do not fit the review scope, or the use of incorrect risk estimates in the meta-analysis) or simply selective choices (e.g. a fully co-pollutant adjusted estimate versus a non-co-pollutant adjusted estimate, or an estimate in a subgroup versus an estimate in the full population) may occur even in SRs that are deemed to be of overall good quality.
Drawing lessons from previous experiences, such as the need to consider new outcomes in the HEI traffic review [ 33 ] or the approach taken in EMAPEC when multiple SRs were available, can significantly improve the assessment process.
Confidence in the CRF
To ascertain confidence in the findings derived from selected systematic reviews and meta-analyses, which serve as sources for the recommended CRFs, a comprehensive evaluation of various aspects concerning the robustness of the results should be taken into consideration [ 26 ]:
Number of studies and size of the cohorts: Evaluate the number of studies (and their size, e.g. the size of the various cohort studies) used in the systematic reviews and meta-analyses. A larger database often contributes to more robust and reliable findings, providing a broader foundation for drawing meaningful conclusions.
Geographic coverage: Assess the geographic diversity of the studies included in the systematic reviews. A wide-ranging representation of diverse populations and regions enhances the generalisability and applicability of the CRFs, contributing to their reliability across different geographical settings.
Weight of studies: Consider the relative weight of individual studies within the systematic reviews. Higher-quality studies with robust methodologies and larger sample sizes should have more influence in the selection of the CRFs, ensuring that the recommendations are anchored in strong evidence. At the same time, it is desirable that the evidence should come from various studies and regions, rather than a limited number of studies.
Precision of effect estimates: Scrutinise the precision of effect estimates provided by the systematic reviews. Precise estimates, indicated by narrow confidence intervals, signify a higher degree of certainty in the observed relationships and contribute to increased confidence in the recommended CRFs.
Unexplained heterogeneity: Evaluate the level of heterogenicity across the studies, as lower unexplained heterogenicity provides greater confidence in the results. The presence of factors that could explain heterogeneity among the included studies should be considered. A practical approach is to evaluate whether there is heterogenicity across regions [ 12 ]. Heterogeneity in the direction of associations (both positive and negative associations) across studies should be considered a factor limiting the confidence in the CRF more than when heterogeneity is in the magnitude of the effects (different effect estimates but in the same direction). Addressing and understanding sources of heterogeneity contribute to the robustness of the CRFs, ensuring that the recommended functions are not unduly influenced by the variability of external factors.
By systematically evaluating these aspects, one can gain valuable insights into the reliability and robustness of the concentration-response functions derived from the systematic reviews and meta-analyses.
A different approach to assess the quality of the epidemiological evidence has been applied in GBD 2021, namely, based on Zheng et al. [ 90 ]; a “Burden of proof risk function (BPRF)” method was developed to understand, evaluate and summarise evidence of risk across different risk-outcome pairs. Five outcomes associated with particulate air pollution (Ischemic Heart Disease, Diabetes, Stroke, Lung cancer, Lower Respiratory Infection) were assigned 3 stars (indicating moderate evidence of association), while COPD was rated 4 stars (indicating strong evidence of association).
Global versus regional CRF
The choice between using a global (based on the ensemble of studies from across the world) or regional CRF (based on studies in a particular continent, country, or location) to estimate the effects of air pollution will depend on several factors, including the nature of the assessment, the specific policy questions, and the intended application. There are various advantages to using global CRFs. (1) they are derived from pooled data covering multiple regions and populations, thus providing a broader perspective of the overall relationship by integrating susceptibility across world populations. (2) The uncertainty around the global estimate could be narrower than the one based on fewer regional studies. (3) A single global CRF can be applied to estimate health impacts in various locations without requiring region-specific CRFs (although region-specific baseline health data would still be necessary). (4) It is suitable for generating overarching policies and general recommendations for widespread application. The last reason is the most compelling because policies for large areas are not intended to account for local specificity. For instance, the Global monitoring of the Sustainable Development Goal (SDG) indicator 3.9.1 (mortality attributed to air pollution) that was established by the United Nations deliberation [ 79 ] applies global functions to estimate the attributable proportions [ 84 ]. Overall, the inclusive nature of global CRF assumes consistent biological linkages between exposure and health effects across different populations and locations and may facilitate a more comprehensive integration of the available evidence.
On the other hand, regional CRFs could better reflect such factors as population demographics (age distribution, disease profile, health status and access to health care coverage), socioeconomic status, personal behavioural risk factors, and local environmental conditions (source contribution and pollution composition) that may influence the relationship between pollutant exposure and health outcomes. For instance, using specific European CRFs for EU regulations could be suggested as it would increase confidence in the calculated disease burden. Regional CRFs are valuable for conducting HIAs tailored to specific communities or regions, providing confidence to local communities in the estimates of the health effects of air pollution [ 60 ]. The argument for using location-specific CRFs is strongest if there is a dominant local source (e.g. a local refinery, or power plant), a particular local PM composition, and also specific population characteristics (for example, the ageing European population compared to much younger populations in other regions of the world).
The regional CRF could be used in an ad hoc analysis to show the particularities of the impact under specific conditions. Another possibility is to construct a CRF that combines the information from the global evidence with that coming from regional studies, such as a weighted mean of the regional value and the pooled estimate e.g. the shrunken estimate approach proposed in Le Tertre et al. [ 44 ]. Of course, the use of a regional CRF is possible only if studies covering a relevant population exists. For many regions, this is still not the case, so the use of the evidence gathered in other parts of the world remains the only choice for the HIA.
Shape of the CRF
The shape of the CRF should be carefully considered. Understanding how the health risk changes with varying levels of exposure (especially in the low and high concentration range) is crucial in a health impact assessment. Most health impact assessments have employed linear concentration-response functions. These relationships assign the same percentage increase in health risk for the same change in PM 2.5 over the entire ambient air pollution concentration range observed in the epidemiological studies. For example, the assessment conducted by the European Environment Agency [ 71 ] assumed a linear concentration-response function for PM 2.5 and natural mortality. However, recent epidemiologic evidence has suggested that the CRF shape at low PM 2.5 concentrations may be supralinear, meaning the change in health risk per unit change in concentration is larger at lower exposures.
In a close examination of the available studies on PM 2.5 and mortality, Vodonos et al. [ 81 ] showed that the CRF slope decreased at higher concentrations. Worth noting that the PM 2.5 contrast range was limited to < 30 µg/m 3 , except for three studies in Asia. The maximum average PM 2.5 concentration was 43.7 µg/m 3 (a study in China). They found that a specific non-linear function approximated the data well, with a larger slope at lower concentration levels, and provided a parametric estimate that fit better than a linear or logarithmic term for average PM 2.5 . In the Global Exposure Mortality Model (GEMM) developed by Burnett et al. [ 9 ], the authors proposed a non-linear CRF for PM 2.5 and mortality (calculated as the sum of noncommunicable diseases and lower respiratory infections in the adult population), based on published health risk data from 41 cohorts in 16 countries. They observed that the hazard ratio predictions increased at low PM 2.5 concentrations, indicating a supralinear association at lower exposures, meanwhile, a gradually decreasing health risk was predicted at higher concentrations [ 8 , 9 ]. The estimated European burden of mortality attributable to PM 2.5 has increased considerably because of the use of this new model in a health impact assessment [ 45 ]. Sigsgaard and Hoffmann [ 70 ] have underlined that the use of the global linear CRF underlying the 2021 WHO Air Quality Guidelines [ 12 ] resulted in a disease burden of 275,000 premature deaths attributable to PM 2.5 exposure in Europe in 2020 (Soares et al. [ 71 ]), but when applying estimates from the supralinear concentration-response functions the resulting disease burden in Europe from PM 2.5 and NO 2 would be much larger (i.e., by ∼ 40% for PM 2.5 and ∼ 110% for NO 2 ). Weichenthal et al. [ 82 ] indicated that considering a supralinear CRF for outdoor PM 2.5 and mortality at the low end of the exposure distribution results in more than 1.5 million additional attributable deaths each year globally.
The most recent evidence from the combined analysis of the “low-level” studies supported by the Health Effects Institute (HEI) should be considered. Chen et al. [ 11 ] reported that the shape of the CRFs differed substantially across the various cohorts. For the ELAPSE study in Europe [ 72 ], only two cohorts (Norway and Denmark) contributed to the shape of the CRF at PM 2.5 levels below 10 µg/m 3 , and only Norway for levels below 7 µg/m 3 . The cohorts from Norway and Canada [ 3 ] reported a supra-linear shape up to 7 µg/m 3 . Such a supra-linear pattern has not been observed in the USA Medicare study [ 23 ], which reported a sub-linear pattern below 7 µg/m 3 , and then a steep slope from 7 to 9 µg/m 3 . Overall, the preliminary conclusion is that the evidence regarding the shape of the CRF at low concentrations is not clear and regional considerations could greatly affect the results.
Since there are uncertainties on the form of the relationship and how to accurately quantify the disease burden from air pollution in areas with low (or high) exposure, it is preferable to consider, as COMEAP indicated in 2022 [ 15 ], that the evidence is not sufficient to recommend any change from the assumption of a linear CRF for long-term exposure to PM 2.5 , at least for concentration levels observed in Europe and North America. With (expected) growth of the epidemiological evidence on the shape of the CRFs at various exposure levels (in particular, in the higher concentrations), better supported decisions on the selection of CRF shape for HIA in a particular population should be possible.
The different shapes of the CRFs and the non-linearities could depend on several factors, including population characteristics, exposure assessment, spatial variation in the composition of total PM 2.5 mass, and measured and unmeasured confounders. For instance, Boogaard et al. [ 2 ] indicated that different population characteristics in rural areas of Canada with lower levels of air pollution might have contributed to the results for that country. In a simulation study, Glasgow et al. [ 29 ] found that the relationship between PM 2.5 and mortality could falsely appear to be supralinear when the fraction of the mass that is toxic is higher in areas with lower total PM 2.5 mass as compared to areas with higher total PM 2.5 mass. Despite the intensive research already conducted, the scientific question of whether some PM mixture components are more toxic than others is still a priority in research [ 2 ].
Applicability of the CRF
Several key assumptions are inherent in all the applications of health impact assessment of air pollution, including two important aspects, namely the generalisability of the CRFs to different age ranges and their applicability to various concentration levels. It is usually assumed that the CRF derived in epidemiology studies conducted in a few countries applies globally despite differences in pollution mix, ethnicity, lifestyle factors, socioeconomic status, temperature, health status, and access to medical care. However, as different populations’ susceptibility to the effects of air pollution is possible, it is at least important to restrict the age range of application of the CRFs to the same age range considered in the specific epidemiologic studies that have generated the CRF. This is why EMAPEC [ 26 ] provided specific age ranges for applying the CRFs in an HIA.
Another important consideration is the concentration range pertinent to the selected CRF. It is advisable to check the range of pollutant concentrations investigated in the original epidemiological studies and apply the CRF only over that range [ 26 ]. The range of mean concentrations in source studies indicates the range of mean exposures for which the uncertainty of the risk assessment is minimised. Figure 2 shows the risk coefficients of the association between PM 2.5 and the incidence of dementia (upper panel) and autism spectrum disorder (ASD) (lower panel) by ranges of concentrations in the various studies that have been evaluated in EMAPEC. For dementia, the bulk of the studies considered in the systematic review by Cheng et al. [ 13 ] cover the range from less than 5 µg/m 3 to 17 µg/m 3 , with two studies extending the range to 25 µg/m 3 , while only one study has been conducted for larger concentrations. For ASD, the bulk of the studies reviewed by Lin et al. [ 48 ] lie in the 5–30 µg/m 3 concentration range, with only one study exceeding this interval. Furthermore, the PM 2.5 contrast intervals (range of concentrations being compared) in most of the individual studies for both diseases was around 10 µg/m 3 . Therefore, in EMAPEC, it was recommended to apply these CRFs in an HIA within the concentration ranges 5–25 µg/m 3 for dementia and 5–30 µg/m 3 for ASD, but for changes in PM 2.5 concentration less than 10 µg/m 3 .

Risk coefficients of the association between PM 2.5 exposure and risk of dementia incidence (upper panel) and Autism Spectrum Disorder (ASD) incidence (lower panel) by ranges of concentrations in the various studies included in the systematic reviews by Cheng et al. [ 13 ] and Lin et al. [ 49 ]
Risk of Double Counting
Understanding the interplay between various CRFs and their respective health predictions is necessary to ensure accurate risk assessments. There are two possible reasons for double counting: when different pollutants cause the same health outcome (as in the well-known case of PM 2.5 and NO 2 ) and across different CRFs when one outcome predicts another outcome.
Note that an attempt to separate the effects of individual pollutants would be pertinent information in assessing the cost of mitigation, as the level of emissions of different pollutants is source-dependent (although interventions that mitigate NOx emission, also affect PM emissions, and vice versa). A potential resolution to the double counting dilemma concerning PM 2.5 and NO 2 in relation to mortality has been thoroughly deliberated by the UK Committee on the Medical Effects of Air Pollutants [ 14 ]. A majority of the Committee agreed that when adding the health effects of NO 2 to the unadjusted PM 2.5 “ it was plausible that the effects on mortality attributable to NO 2 itself lay within the range of 25–55% of the unadjusted coefficient; and that , with suitable strong caveats , this could be used as a guide for policy assessment ”.
An alternative approach is to consider the Cumulative Risk framework, initially introduced by Crouse et al. [ 17 ], which expanded previous work published by Jerrett et al. [ 38 ]. This approach considers the cumulative effects of exposure to various pollutants in the same model in a specific epidemiological study, providing a more comprehensive understanding of the overall health risks associated with air pollution exposure. The cumulative risk estimate assumes additive effects of combined pollutant exposures on the outcome and represents the relative hazard for 1-unit increases in each of the pollutants in the mix compared with no increase in any of the exposures. In the Crouse et al. [ 17 ] analysis of the CanCHEC study in Canada, for example, the single pollutant effect on mortality for PM 2.5 was 1.035 (95%CI 1.029, 1.041) for 5.0 µg/m 3 , the single pollutant effect for NO 2 was 1.052 (1.045, 1.059) for 8.1 ppb (i.e. 15.2 µg/m 3 ), and the cumulative risk estimate (for the same increments of the pollutants, i.e. 5 µg/m 3 for PM 2.5 and 8.1 ppb for NO 2 ) was 1.070 (1.062, 1.078). This example shows that there is only a small overlap of the effects as the cumulative effect (1.070) is only slightly smaller than the sum of the single pollutant effects (1.035 and 1.052). A systematic review and meta-analysis of several epidemiological studies that provide results from single pollutant models as well as from two-pollutant models could better inform the debate about the overlap, double counting, and decision-making process.
There are numerous scenarios in which a particular disease or disorder acts as an antecedent, or risk factor, for another health condition. Figure 3 illustrates the interconnection between various health outcomes commonly suggested for health impact assessments, drawing from robust evidence in established medical literature. However, a crucial question arises regarding whether these associations might lead to double counting of the health impact. For instance, when predicting the influence of air pollution on the incidence of specific disorders like diabetes and stroke, the independent counting of diseases is generally not problematic. However, if we shift our focus to prevalence instead of incidence, considering that an individual can simultaneously have diabetes and be a survivor of a stroke episode, or if we aim to evaluate the economic costs associated with these health outcomes, a more cautious approach is warranted. This necessitates careful consideration of the interplay between different health conditions and their implications for health impact assessment and economic evaluation. Emerging studies on the role of air pollution in the transition between various stages of the same disease or related diseases include, for example, Zhang et al. [ 89 ] and Zou et al. [ 91 ].

Schematic representation of the links between various air pollution-related outcomes (TIA, transient ischaemic attack)
Quantitative risk assessment requires a robust framework for choosing the relevant CRFs and their application to the population at risk. The evolving landscape of air pollution epidemiology underscores the urgency of science-based support to actions addressing global risks of air pollution through robust research, advanced modelling, and comprehensive risk assessments. Rigaud et al.‘s [ 64 ] contribution and the studies discussed in this review collectively contribute to the evolving risk assessment methodology. Addressing challenges requires a comprehensive and adaptive approach, drawing on lessons from past experiences, incorporating the latest research findings, and fostering collaboration between different disciplines involved in the health impact assessment. Finally, a robust and reliable quantitative risk assessment is critical in supporting a cost-benefit analysis of measures to mitigate air pollution.
Data availability
No datasets were generated or analysed during the current study.
https://www.epa.gov/pm-pollution/national-ambient-air-quality-standards-naaqs-pm .
https://www.europarl.europa.eu/legislative-train/theme-a-european-green-deal/file-revision-of-eu-ambient-air-quality-legislation .
Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Fischer P, Nieuwenhuijsen M, Vineis P, Xun WW, Katsouyanni K, Dimakopoulou K, Oudin A, Forsberg B, Modig L, Havulinna AS, Lanki T, Turunen A, Oftedal B, Nystad W, Nafstad P, De Faire U, Pedersen NL, Östenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Overvad K, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Krämer U, Heinrich J, de Hoogh K, Key T, Peters A, Hampel R, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Künzli N, Schindler C, Schikowski T, Adam M, Phuleria H, Vilier A, Clavel-Chapelon F, Declercq C, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Brunekreef B, Hoek G. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. 2014;383(9919):785–95. https://doi.org/10.1016/S0140-6736(13)62158-3 . Epub 2013 Dec 9. PMID: 24332274.
Article CAS Google Scholar
Boogaard H, Crouse DL, Tanner E, Mantus E, van Erp AM, Vedal S, Samet J. Assessing adverse Health effects of Long-Term exposure to low levels of Ambient Air Pollution: the HEI experience and what’s Next? Environ Sci Technol. 2024;58(29):12767–83. https://doi.org/10.1021/acs.est.3c09745 . Epub 2024 Jul 11. PMID: 38991107; PMCID: PMC11270999.
Brauer M, Brook JR, Christidis T, Chu Y, Crouse DL, Erickson A, et al. Mortality-air Pollution associations in low exposure environments (MAPLE): phase 2. Research Report 212. Boston, MA: Health Effects Institute; 2022.
Google Scholar
Briggs DJ. A framework for integrated environmental health impact assessment of systemic risks. Environ Health. 2008;7:61.
Article Google Scholar
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD, American Heart Association Council on Epidemiology and Prevention. Council on the kidney in Cardiovascular Disease, and Council on Nutrition, physical activity and metabolism. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. https://doi.org/10.1161/CIR.0b013e3181dbece1 . Epub 2010 May 10. PMID: 20458016.
Brunekreef B, Dockery DW, Krzyzanowski M. Epidemiologic studies on short-term effects of low levels of major ambient air pollution components. Environ Health Perspect. 1995;103(2):3–13. https://doi.org/10.1289/ehp.95103s23 . PMID: 7614944; PMCID: PMC1518847.
Brunekreef B, Strak M, Chen J, Andersen ZJ, Atkinson R, Bauwelinck M, et al. Mortality and Morbidity effects of Long-Term exposure to low-level PM2.5, Black Carbon, NO2, and O3: an analysis of European cohorts. Boston, MA: Health Effects Institute: Research Report; 2021.
Burnett R, Cohen A. Relative risk functions for estimating excess mortality attributable to Outdoor PM2.5 Air Pollution: evolution and state-of‐the‐art. Atmosphere. 2020;11:589. https://doi.org/10.3390/atmos11060589 .
Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA 3rd, Apte JS, Brauer M, Cohen A, Weichenthal S, Coggins J, Di Q, Brunekreef B, Frostad J, Lim SS, Kan H, Walker KD, Thurston GD, Hayes RB, Lim CC, Turner MC, Jerrett M, Krewski D, Gapstur SM, Diver WR, Ostro B, Goldberg D, Crouse DL, Martin RV, Peters P, Pinault L, Tjepkema M, van Donkelaar A, Villeneuve PJ, Miller AB, Yin P, Zhou M, Wang L, Janssen NAH, Marra M, Atkinson RW, Tsang H, Quoc Thach T, Cannon JB, Allen RT, Hart JE, Laden F, Cesaroni G, Forastiere F, Weinmayr G, Jaensch A, Nagel G, Concin H, Spadaro JV. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci U S A. 2018;115(38):9592–7. https://doi.org/10.1073/pnas.1803222115 . Epub 2018 Sep 4. PMID: 30181279; PMCID: PMC6156628.
Cesaroni G, Badaloni C, Gariazzo C, Stafoggia M, Sozzi R, Davoli M, Forastiere F. Long-term exposure to Urban Air Pollution and Mortality in a cohort of more than a million adults in Rome. Environ Health Perspect. 2013;121:324–31. https://doi.org/10.1289/ehp.1205862 .
Chen J, Hoek G. Long-term exposure to PM and all-cause and cause-specific mortality: a systematic review and meta-analysis. Environ Int. 2020;143:105974. https://doi.org/10.1016/j.envint.2020.105974 . PMID: 32703584.
Chen J, Braun D, Christidis T, Cork M, Rodopoulou S, Samoli E, Stafoggia M, Wolf K, Wu X, Yuchi W, Andersen ZJ, Atkinson R, Bauwelinck M, de Hoogh K, Janssen NAH, Katsouyanni K, Klompmaker JO, Kristoffersen DT, Lim YH, Oftedal B, Strak M, Vienneau D, Zhang J, Burnett RT, Hoek G, Dominici F, Brauer M, Brunekreef B. Long-Term Exposure to Low-Level PM2.5 and Mortality: Investigation of Heterogeneity by Harmonizing Analyses in Large Cohort Studies in Canada, United States, and Europe. Environ Health Perspect. 2023;131(12):127003. doi: 10.1289/EHP12141. Epub 2023 Dec 1. PMID: 38039140; PMCID: PMC10691665.
Cheng S, Jin Y, Dou Y, et al. Long-term particulate matter 2.5 exposure and dementia: a systematic review and meta-analysis. Public Health. 2022;212:33–41. https://doi.org/10.1016/j.puhe.2022.08.006 .
Committee on the Medical Effects of Air Pollutants (COMEAP). Associations of long-term average concentrations of nitrogen dioxide with mortality. A report by the Committee on the Medical Effects of Air Pollutants, GOV.UK (www.gov.uk) 2018.
Committee on the Medical Effects of Air Pollutants (COMEAP). Particulate air pollution: quantifying effects on mortality – appendix B: Summary of COMEAP views on the studies in populations with low-level exposures and the shape of the concentration-response curve. A report by the Committee on the Medical Effects of Air Pollutants, GOV.UK (www.gov.uk), 2022.
Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O, Khan S, Atari DO, Jerrett M, Pope CA, Brauer M, Brook JR, Martin RV, Stieb D, Burnett RT. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ Health Perspect. 2012;120(5):708–14. https://doi.org/10.1289/ehp.1104049 . Epub 2012 Feb 7. PMID: 22313724; PMCID: PMC3346774.
Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, Villeneuve PJ, Jerrett M, Goldberg MS, Pope CA 3rd, Brauer M, Brook RD, Robichaud A, Menard R, Burnett RT. Ambient PM2.5, O₃, and NO₂ exposures and associations with Mortality over 16 years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect. 2015;123(11):1180–6. https://doi.org/10.1289/ehp.1409276 . Epub 2015 Nov 1. PMID: 26528712; PMCID: PMC4629747.
de Hoogh K, Gulliver J, Donkelaar AV, Martin RV, Marshall JD, Bechle MJ, Cesaroni G, Pradas MC, Dedele A, Eeftens M, Forsberg B, Galassi C, Heinrich J, Hoffmann B, Jacquemin B, Katsouyanni K, Korek M, Künzli N, Lindley SJ, Lepeule J, Meleux F, de Nazelle A, Nieuwenhuijsen M, Nystad W, Raaschou-Nielsen O, Peters A, Peuch VH, Rouil L, Udvardy O, Slama R, Stempfelet M, Stephanou EG, Tsai MY, Yli-Tuomi T, Weinmayr G, Brunekreef B, Vienneau D, Hoek G. Development of West-European PM 2.5 and NO 2 land use regression models incorporating satellite-derived and chemical transport modelling data. Environ Res. 2016;151:1–10. https://doi.org/10.1016/j.envres.2016.07.005 . Epub 2016 Jul 20. PMID: 27447442.
Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, Dominici F, Schwartz JD. Air Pollution and Mortality in the Medicare Population. N Engl J Med. 2017;376(26):2513–22. https://doi.org/10.1056/NEJMoa1702747 . PMID: 28657878; PMCID: PMC5766848.
Diao M, Holloway T, Choi S, O’Neill SM, Al-Hamdan MZ, Van Donkelaar A, Martin RV, Jin X, Fiore AM, Henze DK, Lacey F, Kinney PL, Freedman F, Larkin NK, Zou Y, Kelly JT, Vaidyanathan A. Methods, availability, and applications of PM 2.5 exposure estimates derived from ground measurements, satellite, and atmospheric models. J Air Waste Manag Assoc. 2019;69(12):1391–414. Epub 2019 Oct 15. PMID: 31526242; PMCID: PMC7072999.
Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG Jr, Speizer FE. An association between air pollution and mortality in six US cities. N Engl J Med. 1993;329(24):1753-9. https://doi.org/10.1056/NEJM199312093292401 . PMID: 8179653.
Dominici F, Zigler C. Best practices for gauging evidence of causality in Air Pollution Epidemiology. Am J Epidemiol. 2017;186(12):1303–9. https://doi.org/10.1093/aje/kwx307 . PMID: 29020141; PMCID: PMC5860368.
Dominici F, Zanobetti A, Schwartz J, Braun D, Sabath B, Wu X. (2022). Assessing adverse health effects of long-term exposure to low levels of ambient air pollution: implementation of causal inference methods. Research Report Health Effects Institute, 2022(211), 1–56. PMID: 36193708.
Erickson AC, Brauer M, Christidis T, Pinault L, Crouse DL, van Donkelaar A, Weichenthal S, Pappin A, Tjepkema M, Martin RV, Brook JR, Hystad P, Burnett RT. Evaluation of a method to indirectly adjust for unmeasured covariates in the association between fine particulate matter and mortality. Environ Res. 2019;175:108–116. doi: 10.1016/j.envres.2019.05.010. Epub 2019 May 11. PMID: 31108354.
Fischer PH, Marra M, Ameling CB, Hoek G, Beelen R, de Hoogh K, Breugelmans O, Kruize H, Janssen NA, Houthuijs D. Air Pollution and Mortality in seven million adults: the Dutch Environmental Longitudinal Study (DUELS). Environ Health Perspect. 2015;123(7):697–704. Epub 2015 Mar 11. PMID: 25760672; PMCID: PMC4492265.
Forastiere F, Spadaro JV, Ancona C, Jovanovic Andersen Z, Cozzi I, Gumy S, Loncar D, Mudu P, Medina S, Perez Velasco R, Walton H, Zhang J, Krzyzanowski M. (2024). Choices of morbidity outcomes and concentration-response functions for Health Risk Assessment of long-term exposure to air pollution. Environmental Epidemiology, 8(4):p e314, August 2024. DOI: 10.1097/EE9.0000000000000314 .
GBD 2021 Forecasting Collaborators. Burden of disease scenarios for 204 countries and territories, 2022–2050: a forecasting analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2204–2256. https://doi.org/10.1016/S0140-6736(24)00685-8 . PMID: 38762325.
GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2162–2203. https://doi.org/10.1016/S0140-6736(24)00933-4 . PMID: 38762324.
Glasgow G, Ramkrishnan B, Smith AE. Model misspecification, measurement error, and apparent supralinearity in the concentration-response relationship between PM2.5 and mortality. PLoS ONE. 2024;19(5):e0303640. https://doi.org/10.1371/journal.pone.0303640 . PMID: 38781233; PMCID: PMC11115258.
Hammer MS, van Donkelaar A, Li C, Lyapustin A, Sayer AM, Hsu NC, Levy RC, Garay MJ, Kalashnikova OV, Kahn RA, Brauer M, Apte JS, Henze DK, Zhang L, Zhang Q, Ford B, Pierce JR, Martin RV. Global estimates and long-term trends of fine particulate matter concentrations (1998–2018). Environ Sci Technol. 2020;54(13):7879–90. https://doi.org/10.1021/acs.est.0c01764 . Epub 2020 Jun 17. PMID: 32491847.
Hao H, Wang Y, Zhu Q, Zhang H, Rosenberg A, Schwartz J, Amini H, van Donkelaar A, Martin R, Liu P, Weber R, Russel A, Yitshak-Sade M, Chang H, Shi L. National Cohort Study of Long-Term exposure to PM 2.5 components and mortality in Medicare American older adults. Environ Sci Technol. 2023;57(17):6835–43. https://doi.org/10.1021/acs.est.2c07064 . Epub 2023 Apr 19. PMID: 37074132; PMCID: PMC10157884.
Harris-Roxas B, Viliani F, Bond A, Cave B, Divall M, Furu P, Harris P, Soeberg M, Wernham A, Winkler M. Health impact assessment: the state of the art. Impact Assess Proj Apprais. 2012;30(1):43–52.
HEI (Health Effects Institute) Panel. 2022. Systematic Review and Meta-Analysis of Selected Health Effects of Long-Term Exposure to Traffic-Related Air Pollution. Special Report 23. Boston, MA, US: Health Effects Institute. https://www.healtheffects.org/publication/systematic-review-and-meta-analysis-selected-health-effects-long-term-exposure-traffic
Héroux ME, Anderson HR, Atkinson R, Brunekreef B, Cohen A, Forastiere F, Hurley F, Katsouyanni K, Krewski D, Krzyzanowski M, Künzli N, Mills I, Querol X, Ostro B, Walton H. Quantifying the health impacts of ambient air pollutants: recommendations of a WHO/Europe project. Int J Public Health. 2015;60(5):619–27. Epub 2015 May 30. PMID: 26024815; PMCID: PMC4480843.
Hoek G, Boogaard H, Knol A, de Hartog J, Slottje P, Ayres JG, Borm P, Brunekreef B, Donaldson K, Forastiere F, Holgate S, Kreyling WG, Nemery B, Pekkanen J, Stone V, Wichmann HE, van der Sluijs J. Concentration response functions for ultrafine particles and all-cause mortality and hospital admissions: results of a European expert panel elicitation. Environ Sci Technol. 2010;44(1):476–82. https://doi.org/10.1021/es9021393 .
Hoffmann B, Brunekreef B, Andersen ZJ, Forastiere F, Boogaard H. Benefits of future clean air policies in Europe: Proposed analyses of the mortality impacts of PM 2.5 and NO 2 . Environ Epidemiol. 2022;6(5):e221. https://doi.org/10.1097/EE9.0000000000000221 .
Hvidtfeldt UA, Severi G, Andersen ZJ, Atkinson R, Bauwelinck M, Bellander T, Boutron-Ruault MC, Brandt J, Brunekreef B, Cesaroni G, Chen J, Concin H, Forastiere F, van Gils CH, Gulliver J, Hertel O, Hoek G, Hoffmann B, de Hoogh K, Janssen N, Jöckel KH, Jørgensen JT, Katsouyanni K, Ketzel M, Klompmaker JO, Krog NH, Lang A, Leander K, Liu S, Ljungman PLS, Magnusson PKE, Mehta AJ, Nagel G, Oftedal B, Pershagen G, Peter RS, Peters A, Renzi M, Rizzuto D, Rodopoulou S, Samoli E, Schwarze PE, Sigsgaard T, Simonsen MK, Stafoggia M, Strak M, Vienneau D, Weinmayr G, Wolf K, Raaschou-Nielsen O, Fecht D. Long-term low-level ambient air pollution exposure and risk of lung cancer - A pooled analysis of 7 European cohorts. Environ Int. 2021;146:106249. https://doi.org/10.1016/j.envint.2020.106249 . Epub 2020 Nov 13. PMID: 33197787.
Jerrett M, Burnett RT, Beckerman BS, Turner MC, Krewski D, Thurston G, et al. Spatial analysis of air pollution and mortality in California. Am J Respir Crit Care Med. 2013;188(5):593–9.
Katsouyanni K, Touloumi G, Spix C, Schwartz J, Balducci F, Medina S, Rossi G, Wojtyniak B, Sunyer J, Bacharova L, Schouten JP, Ponka A, Anderson HR. Short-term effects of ambient sulphur dioxide and particulate matter on mortality in 12 European cities: results from time series data from the APHEA project. Air Pollution and Health: a European Approach. BMJ. 1997;314(7095):1658–63. https://doi.org/10.1136/bmj.314.7095.1658 . PMID: 9180068; PMCID: PMC2126873.
Kerr GH, van Donkelaar A, Martin RV, Brauer M, Bukart K, Wozniak S, Goldberg DL, Anenberg SC. Increasing racial and ethnic disparities in Ambient Air Pollution-Attributable Morbidity and Mortality in the United States. Environ Health Perspect. 2024;132(3):37002. https://doi.org/10.1289/EHP11900 . Epub 2024 Mar 6. PMID: 38445892; PMCID: PMC10916678.
Khomenko S, Cirach M, Pereira-Barboza E, Mueller N, Barrera-Gómez J, Rojas-Rueda D, de Hoogh K, Hoek G, Nieuwenhuijsen M. Premature mortality due to air pollution in European cities: a health impact assessment. Lancet Planet Health. 2021;5(3):e121–34. https://doi.org/10.1016/S2542-5196(20)30272-2 . Epub 2021 Jan 19. PMID: 33482109.
Khomenko S, Pisoni E, Thunis P, Bessagnet B, Cirach M, Iungman T, Barboza EP, Khreis H, Mueller N, Tonne C, de Hoogh K, Hoek G, Chowdhury S, Lelieveld J, Nieuwenhuijsen M. Spatial and sector-specific contributions of emissions to ambient air pollution and mortality in European cities: a health impact assessment. Lancet Public Health. 2023;8(7):e546–58. https://doi.org/10.1016/S2468-2667(23)00106-8 . PMID: 37393093.
Kim H, Byun G, Choi Y, Kim S, Kim S-Y, Lee J-T. Effects of long-term exposure to air pollution on all-cause mortality and cause-specific mortality in seven major cities of South Korea: Korean national health and nutritional examination surveys with mortality follow-up. Environ Res. 2021;192:110290. https://doi.org/10.1016/j.envres.2020.110290 .
Le Tertre A, Schwartz J, Touloumi G. Empirical Bayes and adjusted estimates approach to estimating the relation of mortality to exposure of PM(10). Risk Anal. 2005;25(3):711–8.
Lelieveld J, Klingmüller K, Pozzer A, Pöschl U, Fnais M, Daiber A, Münzel T. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J. 2019;40(20):1590–6. https://doi.org/10.1093/eurheartj/ehz135 . PMID: 30860255; PMCID: PMC6528157.
Li T, Zhang Y, Wang J, Xu D, Yin Z, Chen H, Lv Y, Luo J, Zeng Y, Liu Y, Kinney PL, Shi X. All-cause mortality risk associated with long-term exposure to ambient PM2·5 in China: a cohort study. Lancet Public Health. 2018;3:e470–7. https://doi.org/10.1016/S2468-2667(18)30144-0 .
Liang D, Li Z, Vlaanderen J, Tang Z, et al. A state-of-the-Science Review on High-Resolution Metabolomics Application in Air Pollution Health Research: current progress, Analytical challenges, and recommendations for future direction. Environ Health Perspect. 2023;131(5):56002. https://doi.org/10.1289/EHP11851 . Epub 2023 May 16. PMID: 37192319; PMCID: PMC10187974.
Lim S, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease study 2010. Lancet. 2012;380:2224–60. https://doi.org/10.1016/S0140-6736(12)61766-8 .
Lin LZ, Zhan XL, Jin CY, et al. The epidemiological evidence linking exposure to ambient particulate matter with neurodevelopmental disorders: a systematic review and meta-analysis. Environ Res. 2022;209:112876. https://doi.org/10.1016/j.envres.2022.112876 .
Liu S, Jørgensen JT, Ljungman P, Pershagen G, Bellander T, Leander K, Magnusson PKE, Rizzuto D, Hvidtfeldt UA, Raaschou-Nielsen O, Wolf K, Hoffmann B, Brunekreef B, Strak, Chen J, Mehta A, Atkinson RW, Bauwelinck M, Varraso R, Boutron-Ruault M-C, Brandt J, Cesaroni G, Forastiere F, Fecht D, Gulliver J, Hertel J, de Hoogh K, Janssen NAH, Katsouyanni K, Ketzel M, Klompmaker JO, Nagel G, Oftedal B, Peters A, Tjønneland A, Rodopoulou SP, Samoli E, Bekkevold T, Sigsgaard T, Stafoggia M, Vienneau D, Weinmayr G, Hoek G, Andersen ZJ. Long-term exposure to low-level air pollution and incidence of chronic obstructive pulmonary disease: The ELAPSE project. Environment International 146 (2021). (Liu 2021b).
Liu S, Jørgensen JT, Ljungman P, Pershagen G, Bellander T, Leander K, Magnusson PKE, Rizzuto D, Hvidtfeldt UA, Raaschou-Nielsen O, Wolf K, Hoffmann B, Brunekreef B, Strak M, Chen J, Mehta A, Atkinson RW, Bauwelinck M, Varraso R, Boutron-Ruault MC, Brandt J, Cesaroni G, Forastiere F, Fecht D, Gulliver J, Hertel O, de Hoogh K, Janssen NAH, Katsouyanni K, Ketzel M, Klompmaker JO, Nagel G, Oftedal B, Peters A, Tjønneland A, Rodopoulou SP, Samoli E, Kristoffersen DT, Sigsgaard T, Stafoggia M, Vienneau D, Weinmayr G, Hoek G, Andersen ZJ. Long-term exposure to low-level air pollution and incidence of asthma: the ELAPSE project. Eur Respir J. 2021;57(6):2003099. https://doi.org/10.1183/13993003.03099-2020 . (Liu et al., 2021a).
Maldonado G, Greenland S. Estimating causal effects. Int J Epidemiol. 2002;31(2):422-9. PMID: 11980807.
Mudway IS, Kelly FJ, Holgate ST. Oxidative stress in air pollution research. Free Radic Biol Med. 2020;151:2–6. https://doi.org/10.1016/j.freeradbiomed.2020.04.031 . Epub 2020 May 1. PMID: 32360613; PMCID: PMC7252129.
Murray CJL, Lopez AD, editors. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge: Harvard University Press; 1996.
Nemmar A, Hoet PH, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF, Vanbilloen H, Mortelmans L, Nemery B. Passage of inhaled particles into the blood circulation in humans. Circulation. 2002;105(4):411–4. https://doi.org/10.1161/hc0402.104118 . PMID: 11815420.
Ohlwein S, Kappeler R, Kutlar Joss M, Künzli N, Hoffmann B. Health effects of ultrafine particles: a systematic literature review update of epidemiological evidence. Int J Public Health. 2019;64(4):547–59. https://doi.org/10.1007/s00038-019-01202-7 . Epub 2019 Feb 21. PMID: 30790006.
Orellano P, Kasdagli MI, Pérez Velasco R, Samoli E. Long-term exposure to Particulate Matter and Mortality: an update of the WHO Global Air Quality Guidelines Systematic Review and Meta-analysis. Int J Public Health. 2024;69:1607683. https://doi.org/10.3389/ijph.2024.1607683 . PMID: 39399882; PMCID: PMC11466858.
Ostro B, Spadaro JV, Gumy S, Mudu P, Awe Y, Forastiere F, Peters A. Assessing the recent estimates of the global burden of disease for ambient air pollution: Methodological changes and implications for low- and middle-income countries. Environ Res. 2018;166:713–725. doi: 10.1016/j.envres.2018.03.001. Epub 2018 Jun 5. PMID: 29880237.
Owens EO, Patel MM, Kirrane E, Long TC, Brown J, Cote I, Ross MA, Dutton SJ. Regul Toxicol Pharmacol. 2017;88:332–7. https://doi.org/10.1016/j.yrtph.2017.05.014 . Epub 2017 May 17. PMID: 28526659; PMCID: PMC6613194. Framework for assessing causality of air pollution-related health effects for reviews of the National Ambient Air Quality Standards.
Pascal M, de Crouy, Chanel P, Wagner V, Corso M, Tillier C, Bentayeb M, Blanchard M, Cochet A, Pascal L, Host S, Goria S, Le Tertre A, Chatignoux E, Ung A, Beaudeau P, Medina S. The mortality impacts of fine particles in France. Sci Total Environ. 2016;571:416–25.
Pope AC 3rd, Thun MJ, Namboodiri MM, et al. Particulate air pollution as a predictor of mortality in a prospective study of US adults. Am J Respir Crit Care Med. 1995;151:669–74.
Pope CA 3rd, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, Thurston GD. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287(9):1132–41. https://doi.org/10.1001/jama.287.9.1132 . PMID: 11879110; PMCID: PMC4037163.
Rajagopalan S, Brook RD, Salerno PRVO, Bourges-Sevenier B, Landrigan P, Nieuwenhuijsen MJ, Munzel T, Deo SV, Al-Kindi S. Air pollution exposure and cardiometabolic risk. Lancet Diabetes Endocrinol. 2024;12(3):196–208. https://doi.org/10.1016/S2213-8587(23)00361-3 . Epub 2024 Feb 1. PMID: 38310921.
Rigaud M, Buekers J, Bessems J, Basagaña X, Mathy S, Nieuwenhuijsen M, Slama R. The methodology of quantitative risk assessment studies. Environ Health. 2024;23(1):13. https://doi.org/10.1186/s12940-023-01039-x . PMID: 38281011; PMCID: PMC10821313.
Samet JM, Chiu WA, Cogliano V, Jinot J, Kriebel D, Lunn RM, Beland FA, Bero L, Browne P, Fritschi L, Kanno J, Lachenmeier DW, Lan Q, Lasfargues G, Le Curieux F, Peters S, Shubat P, Sone H, White MC, Williamson J, Yakubovskaya M, Siemiatycki J, White PA, Guyton KZ, Schubauer-Berigan MK, Hall AL, Grosse Y, Bouvard V, Benbrahim-Tallaa L, El Ghissassi F, Lauby-Secretan B, Armstrong B, Saracci R, Zavadil J, Straif K, Wild CP. The IARC Monographs: Updated Procedures for Modern and Transparent Evidence Synthesis in Cancer Hazard Identification. J Natl Cancer Inst. 2020;112(1):30-7. https://doi.org/10.1093/jnci/djz169 .
Schraufnagel DE. The health effects of ultrafine particles. Exp Mol Med. 2020;52(3):311–7. https://doi.org/10.1038/s12276-020-0403-3 . Epub 2020 Mar 17. PMID: 32203102; PMCID: PMC7156741.
Schwartz J. Particulate air pollution and daily mortality in Detroit. Environ Res. 1991;56(2):204 – 13. https://doi.org/10.1016/s0013-9351(05)80009-x . PMID: 1769365.
Schwartz J. Air pollution and daily mortality: a review and meta analysis. Environ Res. 1994;64(1):36–52. https://doi.org/10.1006/enrs.1994.1005 . PMID: 8287841.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. https://doi.org/10.1136/bmj.j4008 . PMID: 28935701; PMCID: PMC5833365.
Sigsgaard T, Hoffmann B. Assessing the health burden from air pollution. Science. 2024;384(6691):33–34. https://doi.org/10.1126/science.abo3801 . Epub 2024 Apr 4. PMID: 38574150.
Soares J, González Ortiz A, Gsella A, Horálek J, Plass D, Kienzler S. Health risk assessment of air pollution and the impact of the new WHO guidelines. European Environment Agency, ETC-HE Report 2022/10, 2022.
Stafoggia M, Oftedal B, Chen J, Rodopoulou S, Renzi M, Atkinson RW, Bauwelinck M, Klompmaker JO, Mehta A, Vienneau D, Andersen ZJ, Bellander T, Brandt J, Cesaroni G, de Hoogh K, Fecht D, Gulliver J, Hertel O, Hoffmann B, Hvidtfeldt UA, Jöckel KH, Jørgensen JT, Katsouyanni K, Ketzel M, Kristoffersen DT, Lager A, Leander K, Liu S, Ljungman PLS, Nagel G, Pershagen G, Peters A, Raaschou-Nielsen O, Rizzuto D, Schramm S, Schwarze PE, Severi G, Sigsgaard T, Strak M, van der Schouw YT, Verschuren M, Weinmayr G, Wolf K, Zitt E, Samoli E, Forastiere F, Brunekreef B, Hoek G, Janssen NAH. Long-term exposure to low ambient air pollution concentrations and mortality among 28 million people: results from seven large European cohorts within the ELAPSE project. Lancet Planet Health. 2022;6(1):e9-e18. https://doi.org/10.1016/S2542-5196(21)00277-1 . PMID: 34998464.
Strak M, Janssen N, Beelen R, Schmitz O, Karssenberg D, Houthuijs D, van den Brink C, Dijst M, Brunekreef B, Hoek G. Associations between lifestyle and air pollution exposure: potential for confounding in large administrative data cohorts. Environ Res. 2017;156:364–73. Epub 2017 Apr 10. PMID: 28395240.
Strak M, Weinmayr G, Rodopoulou S, Chen J, de Hoogh K, Andersen ZJ, Atkinson R, Bauwelinck M, Bekkevold T, Bellander T, Boutron-Ruault MC, Brandt J, Cesaroni G, Concin H, Fecht D, Forastiere F, Gulliver J, Hertel O, Hoffmann B, Hvidtfeldt UA, Janssen NAH, Jöckel KH, Jørgensen JT, Ketzel M, Klompmaker JO, Lager A, Leander K, Liu S, Ljungman P, Magnusson PKE, Mehta AJ, Nagel G, Oftedal B, Pershagen G, Peters A, Raaschou-Nielsen O, Renzi M, Rizzuto D, van der Schouw YT, Schramm S, Severi G, Sigsgaard T, Sørensen M, Stafoggia M, Tjønneland A, Verschuren WMM, Vienneau D, Wolf K, Katsouyanni K, Brunekreef B, Hoek G, Samoli E. Long term exposure to low level air pollution and mortality in eight European cohorts within the ELAPSE project: pooled analysis. BMJ. 2021;374:n1904. https://doi.org/10.1136/bmj.n 1904. PMID: 34470785; PMCID: PMC8409282.
Thurston GD, Kipen H, Annesi-Maesano I, Balmes J, Brook RD, Cromar K, De Matteis S, Forastiere F, Forsberg B, Frampton MW, Grigg J, Heederik D, Kelly FJ, Kuenzli N, Laumbach R, Peters A, Rajagopalan ST, Rich D, Ritz B, Samet JM, Sandstrom T, Sigsgaard T, Sunyer J, Brunekreef B. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J. 2017;49(1):1600419. https://doi.org/10.1183/13993003.00419-2016 . PMID: 28077473; PMCID: PMC5751718.
UN Environment Assembly. (2024). Resolution adopted by the United Nations Environment Assembly on 1 March 2024: 6/10. Promoting regional cooperation on air pollution to improve air quality globally. https://www.unep.org/environmentassembly/unea6/outcomes
US EPA. (2016). Integrated Science Assessment (ISA) for oxides of nitrogen – health criteria (final report, January 2016). Washington (DC): United States Environmental Protection Agency.
US EPA. Integrated science assessment for particulate matter (Final Report, 2019). EPA/600/R-19/188. US: Environment Protection Agency, Research Triangle Park; 2019.
UN General Assembly, Transforming our world: the 2030 Agenda for Sustainable Development. A/ RES/70/1. 2015. https://sdgs.un.org/2030agenda .
van Donkelaar A, Martin RV, Brauer M, Boys BL. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ Health Perspect. 2015;123(2):135–43. https://doi.org/10.1289/ehp.1408646 .
Vodonos A, Awad YA, Schwartz J. The concentration-response between long-term PM 2.5 exposure and mortality; a meta-regression approach. Environ Res. 2018;166:677–89. https://doi.org/10.1016/j.envres.2018.06.021 . Epub 2018 Aug 1. PMID: 30077140.
Weichenthal S, Pinault L, Christidis T, Burnett RT, Brook JR, Chu Y, Crouse DL, Erickson AC, Hystad P, Li C, Martin RV, Meng J, Pappin AJ, Tjepkema M, van Donkelaar A, Weagle CL, Brauer M. How low can you go? Air pollution affects mortality at very low levels. Sci Adv. 2022;8(39):eabo3381. https://doi.org/10.1126/sciadv.abo3381 . Epub 2022 Sep 28. PMID: 36170354; PMCID: PMC9519036.
Weichenthal S, Christidis T, Olaniyan T, van Donkelaar A, Martin R, Tjepkema M, Burnett RT, Brauer M. Epidemiological studies likely need to consider PM 2.5 composition even if total outdoor PM 2.5 mass concentration is the exposure of interest. Environ Epidemiol. 2024;8(4):e317. https://doi.org/10.1097/EE9.0000000000000317 . PMID: 39022188; PMCID: PMC11254114.
WHO. Sustainable development goal indicator 3.9.1: mortality attributed to air pollution. Geneva: World Health Organization; 2024. 3.0 IGO.
WHO. (2021). WHO global air quality guidelines. Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. World Health Organization 2021. https://apps.who.int/iris/handle/10665/345329
WHO. (2006) Air quality guidelines. Global update 2005. Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. World Health Organization 2006.
WHO Regional Office for Europe. Health risk assessment of air pollution – general principles. Copenhagen: WHO Regional Office for Europe; 2016.
Wolf K, Hoffmann B, Andersen ZJ, Atkinson RW, Bauwelinck M, Bellander T, Brandt J, Brunekreef B, Cesaroni G, Chen J, de Faire U, de Hoogh K, Fecht D, Forastiere F, Gulliver J, Hertel O, Hvidtfeldt UA, Janssen NAH, Jørgensen JT, Katsouyanni K, Ketzel M, Klompmaker JO, Lager A, Liu S, MacDonald CJ, Magnusson PKE, Mehta AJ, Nagel G, Oftedal B, Pedersen NL, Pershagen G, Raaschou-Nielsen O, Renzi M, Rizzuto D, Rodopoulou S, Samoli E, van der Schouw YT, Schramm S, Schwarze P, Sigsgaard T, Sørensen M, Stafoggia M, Strak M, Tjønneland A, Verschuren WMM, Vienneau D, Weinmayr G, Hoek G, Peters A, Ljungman PLS. Long-term exposure to low-level ambient air pollution and incidence of stroke and coronary heart disease: a pooled analysis of six European cohorts within the ELAPSE project. Lancet Planet Health. 2021;5(9):e620-e632. https://doi.org/10.1016/S2542-5196(21)00195-9 . PMID: 34508683.
Zhang S, Qian ZM, Chen L, Zhao X, Cai M, Wang C, Zou H, Wu Y, Zhang Z, Li H, Lin H. Exposure to Air Pollution during Pre-Hypertension and Subsequent Hypertension, Cardiovascular Disease, and Death: A Trajectory Analysis of the UK Biobank Cohort. Environ Health Perspect. 2023;131(1):17008. doi: 10.1289/EHP10967. Epub 2023 Jan 25. Erratum in: Environ Health Perspect. 2023;131(2):29001. PMID: 36696106; PMCID: PMC9875843.
Zheng P, Afshin A, Biryukov S, Bisignano C, Brauer M, Bryazka D, Burkart K, Cercy KM, Cornaby L, Dai X, Dirac MA, Estep K, Fay KA, Feldman R, Ferrari AJ, Gakidou E, Gil GF, Griswold M, Hay SI, He J, Irvine CMS, Kassebaum NJ, LeGrand KE, Lescinsky H, Lim SS, Lo J, Mullany EC, Ong KL, Rao PC, Razo C, Reitsma MB, Roth GA, Santomauro DF, Sorensen RJD, Srinivasan V, Stanaway JD, Vollset SE, Vos T, Wang N, Welgan CA, Wozniak SS, Aravkin AY, Murray CJL. The Burden of Proof studies: assessing the evidence of risk. Nat Med. 2022;28(10):2038–44. https://doi.org/10.1038/s41591-022-01973-2 . Epub 2022 Oct 10. PMID: 36216935; PMCID: PMC9556298.
Zou H, Zhang S, Cai M, Qian ZM, Zhang Z, Chen L, Wang X, Arnold LD, Howard SW, Li H, Lin H. Ambient air pollution associated with incidence and progression trajectory of cardiometabolic diseases: a multi-state analysis of a prospective cohort. Sci Total Environ. 2023;862:160803. https://doi.org/10.1016/j.scitotenv.2022.160803 . Epub 2022 Dec 7. PMID: 36493826.
Download references
Acknowledgements
We acknowledge the scientific contribution of all the members of VALESOR (VALUATION OF ENVIRONMENTAL STRESSORS), an EU-funded project ( https://valesor.eu/ ) under HORIZON-HLTH-2022-ENVHLTH-04-01.
The work has been partially funded in the context of the EU project “VALUATION OF ENVIRONMENTAL STRESSORS, VALESOR” Project number: 101095611.
Author information
Authors and affiliations.
National Research Council, IFT, Palermo, Italy
Francesco Forastiere
Environmental Research Group, Imperial College, London, UK
Francesco Forastiere & Michal Krzyzanowski
Unit of Sustainable Health, Umea University, Umea, Sweden
Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia
Spadaro Environmental Research Consultants (SERC), Philadelphia, PA, USA
Joseph V. Spadaro
You can also search for this author in PubMed Google Scholar
Contributions
FF wrote the first draft of the main text, while HO, MK, and JVS provided noteworthy comments and substantial editing of the manuscript. All authors reviewed and approved the last version of the manuscript.
Corresponding author
Correspondence to Francesco Forastiere .
Ethics declarations
Ethics approval and consent to participate.
There was no need to consent as there are no individual data.
Consent for publication
There was no need of consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Forastiere, F., Orru, H., Krzyzanowski, M. et al. The last decade of air pollution epidemiology and the challenges of quantitative risk assessment. Environ Health 23 , 98 (2024). https://doi.org/10.1186/s12940-024-01136-5
Download citation
Received : 07 July 2024
Accepted : 21 October 2024
Published : 14 November 2024
DOI : https://doi.org/10.1186/s12940-024-01136-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Air pollution
- Concentration-response function
- Health Impact Assessment
- Nitrogen Dioxide
- Risk assessment
Environmental Health
ISSN: 1476-069X
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Air pollution and public health: emerging hazards and improved understanding of risk
Frank j kelly, julia c fussell.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2015 Feb 23; Accepted 2015 May 28; Issue date 2015.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Despite past improvements in air quality, very large parts of the population in urban areas breathe air that does not meet European standards let alone the health-based World Health Organisation Air Quality Guidelines. Over the last 10 years, there has been a substantial increase in findings that particulate matter (PM) air pollution is not only exerting a greater impact on established health endpoints, but is also associated with a broader number of disease outcomes. Data strongly suggest that effects have no threshold within the studied range of ambient concentrations, can occur at levels close to PM 2.5 background concentrations and that they follow a mostly linear concentration–response function. Having firmly established this significant public health problem, there has been an enormous effort to identify what it is in ambient PM that affects health and to understand the underlying biological basis of toxicity by identifying mechanistic pathways—information that in turn will inform policy makers how best to legislate for cleaner air. Another intervention in moving towards a healthier environment depends upon the achieving the right public attitude and behaviour by the use of optimal air pollution monitoring, forecasting and reporting that exploits increasingly sophisticated information systems. Improving air quality is a considerable but not an intractable challenge. Translating the correct scientific evidence into bold, realistic and effective policies undisputedly has the potential to reduce air pollution so that it no longer poses a damaging and costly toll on public health.
Keywords: PM toxicity, Emerging risks, Public awareness, Air quality communication
Introduction
Historical perspective.
Air pollution is now fully acknowledged to be a significant public health problem, responsible for a growing range of health effects that are well documented from the results of an extensive research effort conducted in many regions of the world. Whilst there is no doubt that rapid urbanisation means that we are now exposed to unhealthy concentrations and a more diverse variety of ambient air pollutants, palaeopathological research suggests the problem, in the form of smoke, plagued our oldest ancestors. Computerised tomography imaging studies on the bodies of ancient mummies have detected evidence of pneumonia, emphysema, pulmonary oedema and atherosclerosis (Zweifel et al. 2009 ; Thompson et al. 2013 ), whilst autopsies have described extensive carbon deposits in the lung (Zimmerman et al. 1971 ). This in turn has led to a speculative link to the daily inhalation of smoke in confined spaces from fuels used for warmth, cooking and lighting.
Leaping forward through history to Victorian London, the billowing smoke and sulphur dioxide (SO 2 ) from domestic and industrial coal burning, mixed with natural fog, famously caught the imagination of literary and visual artists. They regarded this meteorological phenomenon as a spectacular manifestation of turn-of-the-century life in a cosmopolitan city. Indeed, the unique style that Charles Dickens adopted in his description of the fogs meant that they became a romantic legend. For Claude Monet, the chromatic atmospheric effects created by the effects of smog on sunlight gave London magnificent breadth and became the predominant theme in his renditions of the city. As a consequence, to some, London’s notoriously toxic air became a world-famous institution rather than an appalling social evil. In December 1952, however, a vast and lethal smog, caused by cold stagnant weather conditions that trapped combustion products at ground level, brought about the worst air pollution disaster in history, resulting in an estimated 4000–12,000 deaths and an enormous increase in respiratory and cardiovascular complications (Logan 1953 ; Bell and Davis 2001 ). This crisis was also the direct incentive to pass the Clean Air Act in 1956, which successfully curtailed domestic coal burning in London and other major cities in the UK. At this point, the UK led the world in cleaning up air by implementing smokeless zones, imposing controls on industry, increasing the availability and use of natural gas and changing the industrial and economic structure of the country. The results were considerable reductions in the concentration of smoke and SO 2 (Wilkins 1954 ; Fig. 1 ).
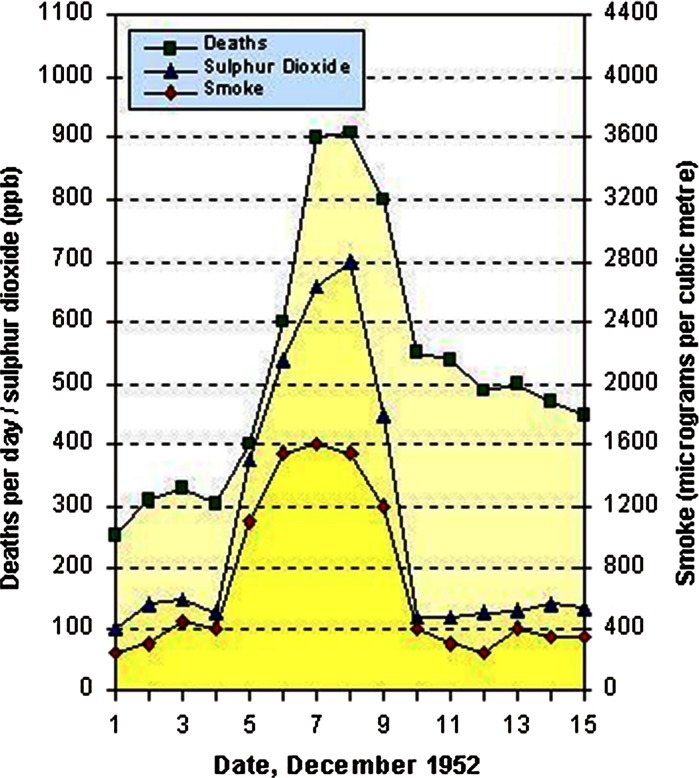
Death toll and pollution concentrations during the 1952 London Smog. Source : Wilkins ( 1954 )
Modern-day air pollution
On recounting such progress, it is especially disappointing that in recent years, improvements in air quality, not solely within the UK but in many urban areas around the world, have miserably stalled. We occasionally experience smog hanging over our cities when poor air-flow and dispersal allows pollution to build up—and it is during such episodes that susceptible individuals (e.g. those with asthma, COPD or heart disease) may undergo an acute exacerbation requiring increased medication or admission to hospital. Of greater concern, however, is the inherent, modern type of pollution in today’s urban environments, which unlike the Victorian pea-souper smog, is indiscernible at ground level but manifests in chronic health effects. This ‘invisible killer’ contains nitrogen oxides, ozone (O 3 ) and exceptionally small particulate matter (PM). PM 10 and the more abundant PM 2.5 constitute particles with diameters less than 10 and 2.5 µm, respectively—the latter being approximately 30 times less than the width of human hair. Of the modern-day air pollutants, PM has been held responsible for the majority of health effects. In urban areas, the major source is fossil fuel combustion, primarily from road transport, as well as power stations and factories. In rural and semi-urban areas of developing countries, the burning of biomass fuels on open fires or traditional stoves creates indoor concentrations of PM that far exceed those considered safe in outdoor air.
Over the last 10 years, there has been a substantial increase in findings from many research disciplines (e.g. population exposure, observational epidemiology, controlled exposure studies, animal toxicology and in vitro mechanistic work) that these modern-day ambient pollutants are not only exerting a greater impact on established health endpoints, but are also associated with a broader number of disease outcomes. The aim of this brief review article is to summarise the increased health hazards to emerge from PM air pollution research in recent years, drawing upon findings published in international projects (WHO 2012 , 2013a ), Health Effects Institute (HEI) research reports (HEI 2010 , 2013a , b ), authoritative reviews (Brook et al. 2010 ) and important individual publications. We will also discuss how the increased evidence base of risk relates to current public awareness and understanding of the problem. Indeed, focused education and continued evolution of sophisticated information systems have the potential to achieve a durable change in public attitude and behaviour, in a way that improves people’s health as well as the quality of the air they breathe.
Health effects of PM air pollution
The ultimate effect of air pollution on public health is to bring about premature death. Epidemiological evidence first emerged from American research, which arguably began as a consequence of the 1952 air pollution episode in London. The reported associations between increased respiratory and cardiovascular mortality and acute and chronic exposures to particulate air pollution (Schwartz and Dockery 1992 ; Dockery et al. 1993 ) were subsequently confirmed outside of the USA, in many cities around the world (Katsouyanni et al. 2001 ; Hoek et al. 2002 ; Filleul et al. 2005 ). Of particular note, recent long-term studies show associations between PM and mortality at levels well below the current annual World health Organisation (WHO) air quality guideline level for PM 2.5 . Several updates to the Havard Six Cities Study and the study of the American Cancer Society cohort continue to cite consistent and significant associations between long-term exposure to PM 2.5 and mortality (Lepeule et al. 2012 ; Krewski et al. 2009 ). In addition, new prospective cohorts provide additional evidence of this association, including effects observed at lower concentrations (mean 8.7 μg/m 3 ; interquartile range 6.2 μg/m 3 ), whilst the emerging multicity cities have confirmed previously reported increases in daily mortality (Ostro et al. 2006 ; Naess et al. 2007 ; Crouse et al. 2012 ; Meister et al. 2012 ).
We now understand that air pollution has overtaken poor sanitation and a lack of drinking water to become the main environmental cause of premature death (OECD 2014 ). The latest estimate from the WHO reported that in 2012, approximately 3.7 million people died from outdoor urban and rural sources (WHO 2014 ). The cause of deaths was broken down as follows: ischaemic heart disease (40 %), stroke (40 %); chronic obstructive pulmonary disease (COPD) (11 %), lung cancer (6 %) and acute lower respiratory infections in children (3 %). These figures are based not only on a greater understanding of the diseases caused by poor air quality, but also more accurate exposure assessment that utilises sophisticated measurement and modelling technology. Of note, the overall mortality estimate more than doubles previous ones and reveals that the vast majority of deaths stem from cardiovascular disease.
By region, the largest outdoor air pollution burden is found in the low- and middle-income countries of the Western Pacific and South-East Asia, with 2.6 million linked deaths in 2012 (WHO 2014 ), reflecting the heavy industry and air pollution hotspots within the developing nations of these areas. However, the problem is very much a global one. Focusing on Europe, air pollution is again the biggest environment risk factor behind premature death (EEA 2014 ). In 2012, mortality numbers related to outdoor air pollution in the low- to middle-income, and high-income countries were estimated at 203,000 and 280,000, respectively (WHO 2014 ). In recent years (2010–2012) the proportion of the urban population in the 28 European Union (EU) Member States who live in areas where the EU daily limit value for PM 10 and PM 2.5 concentrations exceeded that was 21 and 10 %, respectively (EEA 2014 ). The percentage of the EU urban population exposure to PM concentrations above the WHO AQG (WHO 2006 ) is significantly higher, reaching 64 and 92 % for PM 10 and PM 2.5, respectively (EEA 2014 ). Life expectancy of Europeans is reduced, on average, by about 8.6 months owing to PM 2.5 pollution (WHO 2013b ), whilst traditional health impact assessment methods used in the project Improving Knowledge and Communication for Decision-making on Air Pollution and Health in Europe (Aphekom 2011 ), estimates that potential exists to increase average life expectancy in the most polluted cities by approximately 22 months if PM 2.5 concentrations were reduced to the WHO AQG annual level (Fig. 2 ).
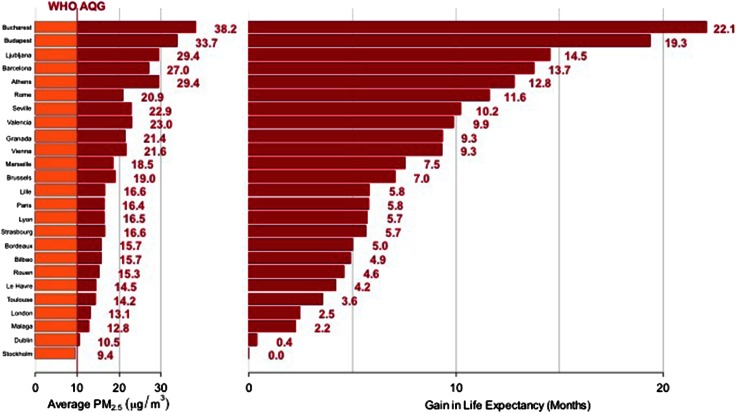
Predicted average gain in life expectancy (months) for persons 30 years of age and older in 25 Aphekom cities for a decrease in average annual level of PM 2.5 to 10 µg/m 3 . Source : Aphekom project, InVS (Aphekom 2011 )
In the UK, outdoor air pollution also makes a significant contribution to mortality. Current (2008) data estimate that if the effect of PM 2.5 air pollution is considered by itself, it is responsible for at least 29,000 premature deaths, alternatively represented as an average loss of life expectancy from birth of approximately 6 months (COMEAP 2010 ). A more recent activity by Public Health England (PHE) has investigated the burden at a more local level in the UK, with mortality rate estimates from long-term PM 2.5 pollution ranging from around 2.5 % in some in rural areas of Scotland and Northern Ireland, between 3 and 5 % in Wales, to over 8 % in certain London boroughs (PHE 2014 ). Upon comparing commonly acknowledged mortality risks, it has been estimated that a 10 µg/m 3 reduction in ambient PM 2.5 pollution (roughly equivalent to eradicating all anthropogenic particles) would have a larger impact on life expectancy in England and Wales than eliminating road traffic accidents or passive smoking (IOM 2006 ).
Cardiopulmonary morbidity
The impact of particulate air pollution on morbidity endpoints has been subject to intense study, resulting in strong scientific consensus on the independent associations of airborne PM 2.5 and PM 10 , with negative impacts on respiratory and cardiovascular health following both short-term and chronic exposures. Furthermore, data strongly suggest that effects have no threshold within the studied range of ambient concentrations, can occur at levels close to PM 2.5 background concentrations and that they follow a mostly linear concentration–response function (WHO 2013a ). Evidence is now well-established and particularly strong for reduced lung function, heightened severity of symptoms in individuals with asthmatics, COPD and ischaemic heart disease which includes heart attacks. We refer to previous reviews on cardiovascular effects (Brook et al. 2010 ) and respiratory disease (Kelly and Fussell 2011 ).
More recent evidence to emerge has now linked long-term exposure to PM 2.5 to atherosclerosis—a condition that underlies many cardiovascular diseases. Indeed, the promotion and vulnerability of atherosclerotic plaques is a potential mechanism by which PM air pollution could trigger cardiovascular mortality and morbidity. In support of this, long-term exposure to PM 2.5 concentrations, as well as proximity to traffic, is associated with preclinical markers (carotid intima media thickness [CIMT] and coronary artery calcification) of atherosclerosis (Künzli et al. 2005 ; Hoffmann et al. 2007 ; Bauer et al. 2010 ) and also with progression of this pathology (Künzli et al. 2010 ).
Emerging respiratory data now link long-term exposure to PM to childhood respiratory disease. Birth cohort studies have suggested associations between PM during pregnancy and higher respiratory need, airway inflammation and an increased susceptibility to respiratory infections (Latzin et al. 2009 ; Jedrychowski et al. 2013 ). The latest meta-analysis of 10 European birth cohorts from the ESCAPE project also provides robust evidence that post-natal PM 10 (but notably not PM 2.5 ), and traffic exposure is associated with an increased risk of pneumonia in early childhood as well as some evidence for an association with otitis media (MacIntyre et al. 2013 ). In a birth cohort in the Netherlands, further associations have been reported between long-term exposure to traffic-related air pollution at the birth address and both symptoms of asthma and low lung function in young children (Gehring et al. 2010 ; Eenhuizen et al. 2013 ; Molter et al. 2013 ). Another interesting epidemiological observation includes a possible link between chronic PM exposure during childhood and vulnerability to COPD in adulthood (Grigg 2009 ).
New health outcomes
Other than the well-documented effects on respiratory and cardiovascular health, an increasing number of studies have investigated the potential of PM air pollution to negatively influence several new health outcomes. We now have evidence linking long-term exposure to PM 2.5 with adverse birth outcomes, whilst emerging data suggest possible effects of long-term PM 2.5 exposure on diabetes, neurodevelopment, cognitive function. The number of studies linking maternal exposure to air pollutants, including particulates, during pregnancy to various birth outcomes is steadily increasing and is of particular interest owing to the crucial time span of biological development and as such, the potential to have long-term consequences on overall health. Harmful effects have been shown for low birth weight, small for gestational age and preterm birth (Ritz and Wilhelm 2008 ; Sapkota et al. 2012 ; Proietti et al. 2013 ). A small number of studies have investigated traffic-related air pollution exposure at participants’ residential address as a novel risk factor for type 2 diabetes mellitus (T2DM). Although not conclusive, results suggest an association between risk of T2DM and exposure to PM (Kramer et al. 2010 ; Puett et al. 2011a ; Coogan et al. 2012 ); however, evidence is stronger for NO 2 and distance to road (Raaschou-Nielsen et al. 2013 ). That the deleterious effects of PM air pollution may extend to the brain have only recently been discovered and research in this area is currently limited and results inconclusive (Guxens and Sunyer 2012 ). For example, a study of women (68–79 years old) who lived for more than 20 years in the same residence showed a significant reduction in mild cognitive function (associated with a high risk of progression to Alzheimer’s Disease) in those who were 74 years old or younger and lived within 50 m to the next busy road with a traffic density of more than 10,000 cars per day (Ranft et al. 2009 ). However, no effect in cognitive function was found for PM 10 concentrations.
Improved air quality and improved health
We now also have consistent evidence that a reduction in the level of particulate pollution following a sustained intervention (mainly regulatory actions) is associated with improvements in public health. In the USA, Pope et al. ( 2009 ) used data from the 51 cities from the American Cancer Society study for which long-term PM 2.5 data are available. It was reported that after adjustment for changes in other risk factors, the reduction in PM 2.5 concentration between 1980 and 2000 was strongly associated with 2.7 year overall increases in life expectancy that occurred during that period (Fig. 3 ). Evidence has also been demonstrated in the Swiss Study on Air Pollution and Lung Diseases in Adults (SAPALIDIA) that assessed lung diseases in adults in eight communities in 1991 and again in 2002—a period when the annual average PM 10 concentration decreased by 5–6 µg/m 3 . This reduction in particle levels was associated with attenuation in the annual rate of decline of lung function (Downs et al. 2007 ). Using the same cohort, Schindler et al. ( 2009 ) reported that fewer reports of regular cough, chronic cough or phlegm, and wheezing and breathlessness could also be attributed to the observed decrease in PM 10 . In a separate Swiss investigation following children from nine Swiss communities between 1992 and 2001, declining concentrations in ambient PM 10 was associated with improved respiratory health (reduced incidence of chronic cough, bronchitis, common cold, nocturnal dry cough and conjunctivitis symptoms; Bayer-Oglesby et al. 2005 ). The results suggest that health improvements can be expected to appear almost immediately and can be seen following almost any decrease in the concentration of PM (for example, the observed beneficial effects in respiratory health of the Swiss children occurred following relatively small changes of rather moderate air pollution levels) enormously strengthens the argument for optimal air quality management.
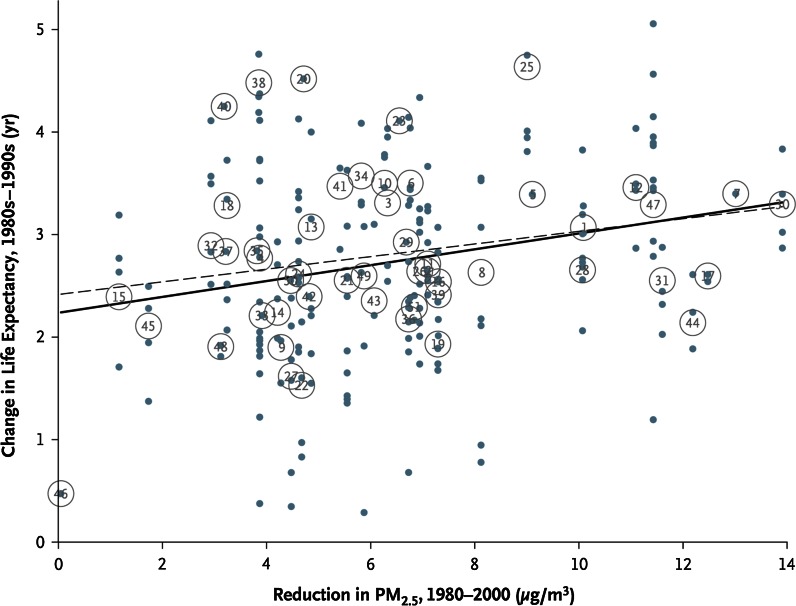
Changes in life expectancy for the 1980s–1990s plotted against reductions in PM 2.5 concentrations for 1980–2000. Dots and circles labelled with numbers represent changes in population-weighted mean life expectancies at the county level and metropolitan area level, respectively. The solid and broken lines represent regression lines with the use of county-level and metropolitan-area-level observations, respectively. Reproduced with permission from Pope et al. ( 2009 )
Differential toxicity of PM
Epidemiological and toxicological research findings have shown that PM mass (PM 2.5 and PM 10 ) comprises fractions and sources with varying types and degrees of health effects (Kelly and Fussell 2012 ). The subject of relative toxicity represents one of the most challenging areas of environmental health research in that PM is not a single entity. It is a complex, heterogeneous mixture that can exist as solids or liquids. These particles vary not only in chemical composition, mass, size (few nanometres to tens of micrometres), number, shape and surface area, but also source, reactivity, solubility and reactivity. In London, particulate pollution is predominantly diesel exhaust particles (DEPs) mixed with resuspended particles of tyre rubber and brake dust (Yanosky et al. 2012 ). This compares with combinations of traffic-derived PM and desert sand in parts of Ghana, biomass smoke Ethiopia and soot from coal fired power stations in the eastern provinces of China. All of the many characteristics of PM have the potential to influence the toxicity of ambient PM. Current knowledge does not, however, allow individual characteristics or sources to be definitely identified as being closely related to specific health effects and likewise, no specific source, component or size category can be excluded as having no adverse effects (EPA 2009 ; WHO 2013a ; HEI 2013a ). Rather, the capability of PM to induce disease may be the result of multiple components acting on different physiological mechanisms.
Below is a brief overview of current evidence on the contribution to adverse health effects played by chemical constituents (black carbon [BC], organic carbon [OC], inorganic secondary aerosols), size (coarse PM, ultrafine particles [UFP) and source (road transport). The findings discussed have arisen from the WHO REVIHAAP Project (Review of Evidence on Health Aspects of Air Pollution) (WHO 2013a ), together with other recent critical reviews and systematic research efforts on the subject (WHO 2012 ; HEI 2010 , 2013a , b ).
Black carbon
In addition to the WHO REVIHAAP project (WHO 2013a ), the health effects of BC particles have also undergone a recent systematic review by the WHO Regional Office for Europe (WHO 2012 ). These initiatives have confirmed that sufficient epidemiological evidence exists to link short-term (daily) variations in BC particles with all-cause and cardiovascular mortality and cardiopulmonary hospital admissions. Evidence is also conclusive that long-term (annual) BC exposure is associated with all-cause and cardiopulmonary mortality. Although distinct mechanistic effects have not been identified from toxicological studies, suggesting that BC may not be a direct toxic component of fine PM, it is hypothesised that these particles may operate as a universal carrier of combustion-derived chemicals (semi-volatile organic fractions, transition metals) of varying toxicity to not only the lungs, but to systemic circulation and beyond. Furthermore, in that short-term studies show that health effect associations with BC were more robust than those with PM 2.5 or PM 10 , although BC particles may not constitute a causal agent, it is the opinion that they may well serve as a better indicator of harmful particulate substances (e.g. organics) from primary traffic-related combustion particles compared to undifferentiated PM mass (WHO 2012 ).
Organic carbon
OC is a very complex and heterogenous mixture of primary and secondary organic aerosols and owing to the common combustion source, can co-exist with BC. As a consequence, it is a huge challenge to identify the potential toxicity of specific OC constituents and in fact evidence is currently insufficient to distinguish between the toxicity of primary and secondary organic aerosols. Studies are, however, generating increasing amounts of data on associations between total organic carbon and a variety of health effects including short-term perturbations in both respiratory (Kim et al. 2008 ; Hildebrandt et al. 2009 ) and cardiovascular (Delfino et al. 2010 ; Ito et al. 2011 ; Kim et al. 2012 ; Son et al. 2012 ; Zanobetti and Schwartz 2009 ) endpoints. Ostro et al. ( 2010 ) has also observed associations between long-term exposure to organic carbon and both ischaemic heart disease and pulmonary mortality.
Inorganic secondary aerosols
Epidemiological evidence continues to accumulate on the short-term effects of sulphate on cardiovascular mortality as well as both respiratory and cardiovascular hospital admissions (Ito et al. 2011 ; Kim et al. 2012 ). Data have also emerged on associations between daily increments in ambient sulphate and physiological changes to the cardiovasculature, namely ventricular arrhythmias (Anderson et al. 2010 ) and markets of endothelial dysfunction (Bind et al. 2012 ). The HEI’s comprehensive National Particle Component (NPACT) initiative also identified significant associations in the epidemiological studies between secondary inorganic sulphate and health effects and moreover, these were backed up by complimentary findings in the toxicological element of the project (HEI 2013a ). Historically, toxicological evidence has been seemingly consistent that the components of inorganic secondary aerosols (ammonium, sulphates or nitrates) pose little threat, but uncertainties do exist. For example, the cations (metals, hydrogen) associated with sulphates/nitrates and/or other absorbed components (metals, organic particles) may have an underlying toxic role or else secondary inorganic components may influence bioavailability and as a consequence, toxicity of other particulate components (Oakes et al. 2012 ).
Accumulating epidemiological evidence suggests that short-term exposures to coarse particles (between 2.5 and 10 μm) are associated with effects on adverse cardiovascular health, respiratory endpoints health, including premature mortality (Peng et al. 2008 ; Atkinson et al. 2010 ; Mann et al. 2010 ; Meister et al. 2012 ; Qiu et al. 2012 ). Overall opinions made by various systematic reviews and assessments are variable as to whether such effect estimates are higher or lower than those for fine PM (Brunekreef and Forsberg 2005 ; EPA 2009 ). Investigations into long-term effects of coarse PM are fewer and have reported no or limited evidence that this size fraction has an effect on mortality or cardiovascular health (Puett et al. 2009 , 2011b ). Toxicological studies comparing coarse and fine PM have reported that coarse particles can be as toxic as PM 2.5 on a mass basis (Graff et al. 2009 ; Wegesser et al. 2009 ). Data, however, are not only scarce, but also difficult to interpret owing differences in the inhalability and deposition efficiency of these size fractions.

Ultrafine particles
UFPs (smaller than 0.1 μm) have many unique properties that have led scientists to hypothesise that this size fraction may have specific or enhanced toxicity relative to fine (PM 2.5 ) or coarse PM. Apart from the relationship between particle diameter and penetration within the lung and to extrapulmonary sites, on a mass basis, smaller particles have a much greater surface area and with that, a high capacity to adsorb toxic chemicals. In addition, the finer the particles, the greater the likelihood of penetration to indoor environments, being suspended in the atmosphere for longer periods and being transported over large distances. As a consequence, a substantial body of literature has now been published on the mechanisms of UFP toxicity and adverse effects in animals and in humans, including a recent HEI review (HEI 2013b ). Epidemiological data, however, are still limited and provide suggestive rather than strong and consistent evidence of adverse effects of UFPs [reviewed by Rückerl et al. ( 2011 ), Weichenthal ( 2012 )]. The HEI review noted that “The current evidence does not support a conclusion that exposure to UFPs alone can account in substantial ways for the adverse effects of PM 2.5 ” (HEI 2013b ). Toxicological studies have certainly advanced our understanding of the action of UFPs, showing the potential of this size fraction to adopt differential patterns of deposition, clearance and translocation (Kreyling et al. 2010 ).
Many PM pollution sources, namely coal combustion, shipping, power generation, the metal industry, biomass combustion, desert dust episodes and road transport have been associated with different types of health effects (EPA 2009 ; WHO 2013a ). Of these, the main source of urban pollution—road transport—is also the source associated with the most serious health outcomes. A critical review of the literature on the health effects of traffic-related air pollution concluded that sufficient evidence had accumulated to support a causal relationship between exposure to traffic-related air pollution and exacerbation of asthma. Further evidence was found to be suggestive of a causal relationship with onset of childhood asthma, non-asthma respiratory symptoms, impaired lung function, total and cardiovascular mortality, and cardiovascular morbidity (HEI 2010 ).
The PM components from road traffic include engine emissions, comprising largely of EC and OC, plus non-exhaust sources that are often characterised by elevated concentrations of transition metals (brake wear [copper, antimony], tyre abrasion [zinc], dust from road surfaces [iron]). The largest single source is derived from diesel exhaust (DE). Indeed, owing to the increased domestic market penetration of diesel engines, the fuel powering the majority of our buses and taxis in many industrialised countries and the fact that they generate up to 100 times more particles than comparable gasoline engines with 3-way catalytic convertors (Quality of urban air review group 1996 ), diesel exhaust particles (DEPs) contribute significantly to the air shed in many of the world’s largest cities. DEPs have also been shown to have substantial toxicological capacity, facilitated by the size (80 % of DEPs have an aerodynamic diameter of <1 µm) of such particles as well as their surface chemistry characteristics. For instance, DEPs have a highly adsorptive carbon core that act as a vector for the delivery, deep into the lung, of redox active metals, polyaromatic hydrocarbons and quinones. In addition to traffic density per se, it is not surprising therefore that the greatest health impacts appear to be associated with proximity to roads carrying a high proportion of diesel powered heavy and light good vehicles (Janssen et al. 2003 ; Gowers et al. 2012 ). In 2012, the International Agency for Research on Cancer (IARC) classified particulates in diesel fumes as carcinogenic to humans based on sufficient evidence that it is linked to an increased risk of lung cancer, as well as limited evidence linking it to an increased risk of bladder cancer (IARC 2012 ). Although most studies into the toxicity and health consequences of roadside PM have focused on DEPs, the non-exhaust sources are attracting interest and deservedly so (van der Gon et al. 2013 ). Whilst contributions from brake/tyre wear and road surface abrasion in the wake of passing traffic will become more important with progressive reductions in exhaust emissions, their potential to elicit health effects is largely ignored at the regulatory level despite links with cardiopulmonary toxicity (Gasser et al. 2009 ; Gottipolu et al. 2008 ; Mantecca et al. 2009 ; Riediker et al. 2004 ).
Mechanisms of PM toxicity
The well-established evidence that PM pollution contributes to an array of health outcomes has resulted in an enormous research effort to understand the underlying biological basis of toxicity by identifying mechanistic pathways. Although there remains much to be understood, our appreciation of the physiological effects and plausible biological mechanisms that link short- and long-term PM 2.5 exposure with mortality and morbidity has evolved rapidly and continues to do so. For example, in investigating subclinical physiological changes, epidemiological research has reported variations in cardiovascular biomarkers of systemic inflammation such as C-reactive protein and fibrinogen—subtle responses that have been consistently linked to subsequent cardiovascular disease and death (Brook et al. 2010 ). A particularly powerful tool to study mechanistic pathways and physiological endpoints related to adverse effects following DEP exposure is the use of controlled exposure studies in healthy volunteers (Salvi et al. 1999 , 2000 ; Mudway et al. 2004 ; Pourazar et al. 2004 , 2005 ; Mills et al. 2005 ; Behndig et al. 2006 ; Peretz et al. 2007 ; Tornqvist et al. 2007 ; Lucking et al. 2008 ; Lundback et al. 2009 ) as well as mild asthmatics (Stenfors et al. 2004 ) and individuals with stable coronary heart disease (Mills et al. 2007 ). Carefully characterised and environmentally relevant DE exposure experiments, combined with cardiovascular measurements, BAL and bronchial biopsy have revealed well-defined systemic, pulmonary and cardiac responses involving a variety of cellular and molecular perturbations. It is probable that associations between the various constituents of PM and health effects are the result of multiple, complex and interdependent mechanistic pathways acting on different physiological mechanisms. Current evidence does, however, support a chain of events involving pollution-induced pulmonary and systemic oxidative stress and inflammation, translocation of particle constituents and an associated risk of vascular dysfunction, atherosclerosis, altered cardiac autonomic function and ischaemic cardiovascular and obstructive pulmonary diseases (Kelly and Fussell 2015 ; Fig. 4 ).
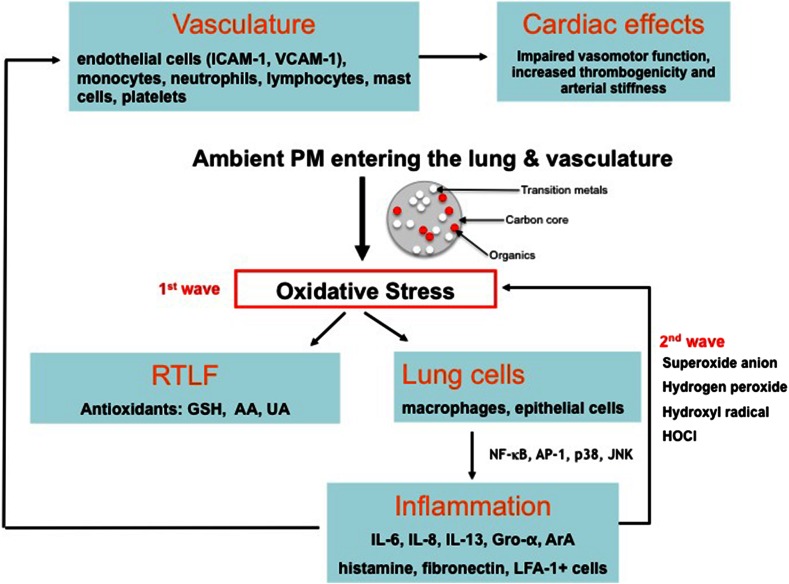
Biological pathways linking PM exposure with oxidative and inflammatory pathways in the lung and cardiovasculature
Since oxidative stress is widely believed to play a key role in the harmful effects of a range of particles at the cellular level, the oxidative potential (OP) of PM (their capacity to cause damaging oxidative reactions) is regarded as an attractive exposure metric in our bid to identify the toxic components and sources within an ambient PM mix (Ayres et al. 2008 ; HEI 2010 ). The OP of ambient PM collected at busy roadside sites is clearly enhanced relative to urban background and rural sites, and this appears to be associated with an enrichment of metals (copper, barium) linked with abrasion and brake wear processes (Godri et al. 2011 ; Kelly et al. 2011 ; Boogaard et al. 2012 ). Concern surrounding these findings is well founded in that they highlight a toxic contribution by non-exhaust pollutants and as such, by a currently unregulated source. Oxidative stress is linked to several DNA lesions and the formation of bulky adducts—mechanisms by which traffic-related pollution could elicit mutagenesis and in turn cause cancer (Loeb 2001 ). Of the biomarkers of oxidatively damaged DNA, urinary excretion of 8-oxo-7,8-dihydro-2-deoxyguanosine (8oxodG) has now been validated to evaluate the pro-oxidant effects of vehicle exhaust emissions on the DNA of exposed subjects (Barbato et al. 2010 ). DNA adduct levels in non-smoking workers have been found to reflect average levels of exposure to PM 10 in high-traffic urban areas (Palli et al. 2008 ) and were also reported to be increased in cord blood after maternal exposures to traffic-related air pollution (Pedersen et al. 2009 )—the latter demonstrating the potential for transplacental environmental exposures to induce DNA damage early in newborns and with that, increased risk for adverse effects later in life.
Public awareness and education
That poor air quality can have such a significant impact on human health is undisputed, and the previous sections have drawn upon research conducted over recent years that supports the notion that risks are increasing as new hazards emerge. How then does this translate to public awareness of the problem? The general consensus is that society would benefit from being better engaged and educated about the complex relationship between air quality and ill health (Kelly et al. 2012 ). If people are aware of variations in the quality of the air they breathe, the effect of pollutants on health as well as concentrations likely to cause adverse effects and actions to curtail pollution, there follows a greater likelihood of motivating changes in both individual behaviour and public policy. In turn, such awareness has the potential to create a cleaner environment and a healthier population.
Studies and initiatives examining public awareness and understanding in this area have yielded mixed results, with some acknowledging a significant amount of concern within the public over poor air quality, an awareness of air quality warnings, and a positive relationship between alerts and a change in outdoor activities (DEFRA 2002 ; Wen et al. 2009 ; McDermott et al. 2006 ). In fact, following findings that air quality warnings associated with ground level O 3 do have a significant impact on attendance at outdoor facilities in Southern California, Neidell and Kinney ( 2010 ) suggested that ambient air quality measurements from monitors may not reflect personal exposure if individuals intentionally limit their exposure in response poor air quality. Bell et al. ( 2004 ) have also hypothesised that deliberate avoidance in time spent outdoors could contribute to the considerable heterogeneity in O 3 -induced mortality observed across US communities. Other research has concluded that both awareness of the links between air pollution and ill health and an understanding of air quality information are lacking amongst the public (Bickerstaff and Walker 2001 ; Semenza et al. 2008 ; COMEAP 2011 ). In 2013, the European Commission (EC) conducted a flash Eurobarometer to gain a greater insight into the views of the European public on matters of air quality and air pollution (EC 2013 ). Six out of ten Europeans responded that they did not feel informed about air quality issues in their country. When asked how serious they considered a range of air quality related problems to be in their country, responses for respiratory disorders, cardiovascular diseases and asthma/allergy were 87, 92 and 87 % respectively.
Factors determining awareness
Other than the availability of sufficient information that will be covered in the following section, factors governing how aware individuals are about the quality of their air and potential repercussions for their health are likely to include understanding, perception and a vested interest. Individuals may choose not to concern themselves about air quality owing to a poor understanding of what is undoubtedly a complex science. Unlike other environmental risks that are routinely communicated such as UV and heat, overall air quality encompasses several primary pollutants as well as secondary products owing to atmospheric transformation. Rural areas for example are very often considered safe places to escape from pollution. However, at times, O 3 concentrations can be as high or greater than urban locations owing to the presence of lower concentrations of nitrogen oxides to sequester rural O 3 . A lack of vested interest in the topic is also possible amongst ‘healthy’ people, less likely to have any personal experience of the benefits that lessoning pollution and/or increasing medication may bring. Indeed, where research has indicated that individuals are aware of air quality warnings and take responsive actions, larger responses were observed for more susceptible groups or carers thereof (McDermott et al. 2006 ; Wen et al. 2009 ). Within a cross-sectional study of 33,888 adults participating in the 2005 Behavioral Risk Factor Surveillance System, 31 % with asthma versus 16 % without changed outdoor activity in response to media alerts (Wen et al. 2009 ). Perception is another factor influencing the public understanding of the importance of healthy air, as attitudes and behaviour can be driven by a person’s immediate locality and own understanding rather than accurate data generated by monitoring sites and communicated via an advisory service (Shooter and Brimblecombe 2009 ). Several studies have investigated the relationship between perceived and measured outdoor air quality provided by monitoring stations and whilst some studies found a significant association between the perception of air quality and specific air pollutants (Atari et al. 2009 ), others have found little or no association (Rotko et al. 2002 ). Of relevance, Semenza et al. ( 2008 ) not only reported a low (10–15 %) level of behavioural change during an air pollution episode, but that the personal perception of poor air quality rather than the advisory service, drove the response. Some epidemiological researchers have also indicated that self-reported health status is associated with perceived air pollution rather than measured air pollution (Lercher et al. 1995 ; Yen et al. 2006 ; Piro et al. 2008 ).
Information services
Public awareness is fundamentally dependent upon optimal air pollution monitoring, forecasting and reporting. Many countries have air quality monitoring networks that are structured around a particular country’s regulatory obligation to report monitored air quality data and modelled predictions (Kelly et al. 2012 ). Output from measured concentrations of pollutants, air quality modelling systems and meteorological data are also processed to create a national air quality index (AQI). Again in line with national legislation, an AQI communicates pollution levels and health effects likely to be experienced on the day described by the index or days soon afterwards (i.e. the short term; Table 1 ). These data are used by the public and organisations (health services and governments) to reduce the health impacts of predicted air pollution. For example, people susceptible to high levels of pollution may be prompted to take actions (reduce exposure and/or increase use of inhaled reliever medication) to reduce their symptoms, and the general public may be encouraged to use public rather than private transport during periods of poor air quality. Another information tool is provided by accessible air pollution alert services that provide real-time data and proactively alert registered users of impending pollution events via a computer/tablet (websites, email, social media) or phone (texts, apps) (London Air Quality Network; City of London). These are becoming increasingly informative and engaging, allowing people to sign up to specific user groups (e.g. cyclist, jogger, business, at risk) and receive notifications when pollution exceeds concentrations at a site(s) of their choice. These services also offer tailored advice on how specific groups can reduce emissions by for example, providing low pollution journey planners to reduce exposure (Fig. 5 ).
Health advice for the general population to accompany the UK AQI
a Adults and children with heart or lung problems are at greater risk of symptoms
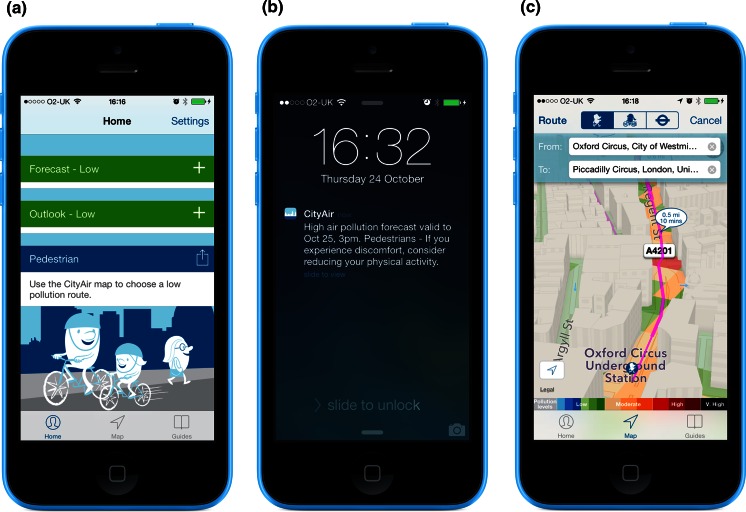
City Air iPhone app. a Advice tailored to specific user groups. b Notification alert when pollution levels change. c 3-D low pollution journey planners
New developments
Whilst monitoring, forecasting and reporting of air quality have become increasingly sophisticated and accurate, the future use of more individualised exposure measurements holds a great deal more potential. Air pollution levels can vary dramatically over short distances and time scales and in addition people’s daily mobility and activities will result in variability in exposure and inhalation. As such, AQIs and alert systems sourced by fixed site monitoring stations are always going to be limited by location, spacing and density. Up until recently, the use of personal pollution monitors was primarily limited to industries associated with high occupational exposures and researchers assessing individual exposures in vulnerable groups such as cyclists (Nwokoro et al. 2012 ) and asthmatic children (Spira-Cohen et al. 2011 ). Now we are witnessing an emerging role for inexpensive, portable, easy-to-use personal monitoring devices (Austen 2015 ). Although the quality of information generated by such sensors is not currently robust enough to compliment data for official monitoring networks, there is undoubtedly a need for more dynamic measures of time-activity patterns in relation to exposures. In an initiative to better understand in real time the impacts of harmful air pollutants, the US Environmental Protection Agency awarded a $100,000 prize to designers of a low-cost wearable breathing analysis tool that calculates the amount of polluted air a person breathes and transmits the data to any Bluetooth-enabled device such as a mobile phone (EPA 2013 ). Smart phone technology, integrated with low-cost air quality sensors, also has the potential to produce dynamic, temporally and spatially more precise exposure measures for the mass population. Added to their ubiquitous technology, the penetration of these phones is unrivalled in demographics, geographic coverage, acceptance and presence in everyday life (Pratt et al. 2012 ). This opens up new possibilities in the communication of individual exposure and activity data, tailored to locations where people commute and reside. In the environmental research setting, novel smartphone-based software that records people’s movements and physical activity levels in the urban environment and is integrated with spatial–temporal maps of air pollution is already being developed to enhance large-scale air pollution exposure data collection in a cost-effective, accurate unobtrusive way (de Nazelle et al. 2013 ).
Despite past improvements in air quality, very large parts of the population in urban areas breathe air that does not meet European standards let alone WHO Air Quality Guidelines. It should not be surprising therefore that health effects of PM—one of the pollutants deemed most dangerous to health—are well documented. Airborne PM has been the focus of extensive research and debate around the world for several decades and as a consequence, the evidence base for the association between short- and long-term exposure to PM and cardiopulmonary mortality and morbidity has become much larger and broader. DEPs are now classified as carcinogenic, and an increasing number of studies are investigating the potential for particulate air pollution to negatively influence birth outcomes, diabetes, neurodevelopment and cognitive function. We now also appreciate that there is no evidence of a safe level of exposure or a threshold below which no adverse health effects occur, with recent long-term studies are showing associations between PM and mortality at levels well below the current annual WHO air quality guideline level for PM 2.5 . Correspondingly, reductions in population exposure to air pollution expressed as annual average PM 2.5 or PM 10 have appreciable benefits in terms of increased life expectancy and improvements to respiratory health.
Having firmly established associations between ambient PM and adverse health effects, there has been an enormous effort to identify what it is in ambient PM that affects health—information that in turn will inform policy makers how best to legislate for cleaner air. The topic of relative toxicity has been the subject of several critical reviews over recent years but despite this the general conclusion remains that the current database of experimental and epidemiologic studies precludes individual characteristics or sources to be definitely identified as critical for toxicity. A better understanding of exposure and health effects plus further progress in comparing and synthesising data from existing studies is therefore needed before concluding that additional indicators (be they BC or UFPs) have a role in protecting public health more effectively than the targeting total PM mass. Another challenge has been to unravel the underlying biological basis of toxicity by identifying pathways that ultimately link pollution-induced pulmonary and systemic oxidative stress with an associated risk of cardiovascular and obstructive pulmonary diseases.
Evidence has emerged that (a) the burden of ambient PM pollution on health is significant at relatively low concentrations, (b) there is no safe lower limit and (c) effects follow a mostly linear concentration–response function, suggesting that public health benefits will result from any reduction in concentrations. As has been advocated many times before, interventions to reduce levels of particulate pollution require a concerted action by a host of sectors with a vested interest in air quality management (environment, transport, energy, health, housing) at regional, national and international levels. The significant toll of ill health brought about by traffic-related particulates means that forward-looking and integrated transport policies are critical for the improvement of urban environments. Traffic must be reduced and we must ensure a cleaner and greener element to what remains on the road. This can be achieved through an expansion of low emission zones, investment in clean and affordable public transport and incentives for its use, a move back from diesel to petrol or at least a ban on all highly polluting diesel vehicles, lowering speed limits and enhancing cycle routes.
Another intervention in moving towards a cleaner and healthier environment necessitates behavioural changes by the public, which in turn requires continued education and optimal communication. Engagement must be blatant and put in the context of other public health risks such as passive smoking, it must also utilise compelling messages such as premature death. In an ideal world, people, and especially susceptible individuals, should be aware of their air quality by regularly checking the AQI or targeted notifications for real-time data before going to work, school or to pursue leisure activities, enabling them to take action in the event of increased pollution. Improving air quality is a considerable but not an intractable challenge. Translating the correct scientific evidence into bold, realistic and effective policies undisputedly has the potential to reduce air pollution so that it no longer poses a damaging and costly toll on public health.
Acknowledgments
This work was supported by the UK’s cross-research council Environmental Exposures and Health Initiative (NE/I007806/1) and the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Health Impact of Environmental Hazards at King’s College London in partnership with Public Health England (PHE). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health or Public Health England.
- Anderson HR, Armstrong B, Hajat S, Harrison R, Monk V, Poloniecki J, et al. Air pollution and activation of implantable cardioverter defibrillators in London. Epidemiology. 2010;21(3):405–413. doi: 10.1097/EDE.0b013e3181d61600. [ DOI ] [ PubMed ] [ Google Scholar ]
- Aphekom. (2011). Improving knowledge and communication for decision making on air pollution and health in Europe. Summary report of the Aphekom project 2008–2011. http://www.endseurope.com/docs/110302b.pdf . Accessed 11 February 2015.
- Atari DO, Luginaah IN, Fung K. The relationship between odour annoyance scores and modelled ambient air pollution in Sarnia, “Chemical Valley”, Ontario. International Journal of Environmental Research and Public Health. 2009;6(10):2655–2675. doi: 10.3390/ijerph6102655. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Atkinson RW, Fuller GW, Anderson HR, Harrison RM, Armstrong B. Urban ambient particle metrics and health: A time-series analysis. Epidemiology. 2010;21(4):501–511. doi: 10.1097/EDE.0b013e3181debc88. [ DOI ] [ PubMed ] [ Google Scholar ]
- Austen K. Environmental science. Pollution patrol. Nature. 2015;517:136–138. doi: 10.1038/517136a. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ayres JG, Borm P, Cassee FR, Castranova V, Donaldson K, Ghio A, et al. Evaluating the toxicity of airborne particulate matter and nanoparticles by measuring oxidative stress potential-a workshop report and consensus statement. Inhalation Toxicology. 2008;20(1):75–99. doi: 10.1080/08958370701665517. [ DOI ] [ PubMed ] [ Google Scholar ]
- Barbato DL, Tomei G, Tomei F, Sancini A. Traffic air pollution and oxidatively generated DNA damage: can urinary 8-oxo-7,8-dihydro-2-deoxyguanosine be considered a good biomarker? A meta-analysis. Biomarkers. 2010;15(6):538–545. doi: 10.3109/1354750X.2010.493974. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bauer M, Moebus S, Möhlenkamp S, Dragano N, Nonnemacher M, Fuchsluger M, et al. Urban particulate matter air pollution is associated with subclinical atherosclerosis. Results from the HNR (Heinz Nixdorf Recall) Study. Journal of the American College of Cardiology. 2010;56(22):1803–1808. doi: 10.1016/j.jacc.2010.04.065. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bayer-Oglesby L, Grize L, Gassner M, Takken-Sahli K, Sennhauser FH, Neu U, et al. Decline of ambient air pollution levels and improved respiratory health in Swiss children. Environmental Health Perspectives. 2005;113(11):1632–1637. doi: 10.1289/ehp.8159. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Behndig AF, Mudway IS, Brown JL, Stenfors N, Heleday R, Duggan ST, et al. Airway antioxidant and inflammatory responses to diesel exhaust exposure in healthy humans. European Respiratory Journal. 2006;27(2):359–365. doi: 10.1183/09031936.06.00136904. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bell ML, Davis DL. Reassessment of the lethal London fog of 1952: Novel indicators of acute and chronic consequences of acute exposure to air pollution. Environmental Health Perspectives. 2001;109(Suppl 3):389–394. doi: 10.1289/ehp.01109s3389. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F, et al. Ozone and short-term mortality in 95 US urban communities, 1987–2000. Journal of the American Medical Association. 2004;292(19):2372–2378. doi: 10.1001/jama.292.19.2372. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bickerstaff K, Walker G. Public understandings of air pollution: The ‘localisation’ of environmental risk. Global Environmental Change. 2001;11(2):133–145. [ Google Scholar ]
- Bind MA, Baccarelli A, Zanobetti A, Tarantini L, Suh H, Vokonas P, et al. Air pollution and markers of coagulation, inflammation, and endothelial function: Associations and epigene-environment interactions in an elderly cohort. Epidemiology. 2012;23(2):332–340. doi: 10.1097/EDE.0b013e31824523f0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boogaard H, Janssen NA, Fischer PH, Kos GP, Weijers EP, Cassee FR, et al. Contrasts in oxidative potential and other particulate matter characteristics collected near major streets and background locations. Environmental Health Perspectives. 2012;120(2):185–191. doi: 10.1289/ehp.1103667. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brook RD, Rajagopalan S, Pope CA, III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease. An update to the Scientific Statement from the American Heart Association. Circulation. 2010;121(21):2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brunekreef B, Forsberg B. Epidemiological evidence of effects of coarse airborne particles on health. European Respiratory Journal. 2005;26(2):309–318. doi: 10.1183/09031936.05.00001805. [ DOI ] [ PubMed ] [ Google Scholar ]
- CityAir. http://cityairapp.com/ . Accessed 13 February 2015.
- Committee on the Medical Effects of Air Pollutants (COMEAP). (2010). The mortality effects of long-term exposure to particulate air pollution in the United Kingdom. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/304641/COMEAP_mortality_effects_of_long_term_exposure.pdf . Accessed 10 February 2010.
- Committee on the Medical Effects of Air Pollutants (COMEAP). (2011). Review of the UK Air Quality Index. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/304633/COMEAP_review_of_the_uk_air_quality_index.pdf . Accessed 21 February 2015.
- Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation. 2012;125(6):767–772. doi: 10.1161/CIRCULATIONAHA.111.052753. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O, et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environmental Health Perspectives. 2012;120(5):708–714. doi: 10.1289/ehp.1104049. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De Nazelle A, Seto E, Donaire-Gonzalez D. Improving estimates of air pollution exposure through ubiquitous sensing technologies. Environmental Pollution. 2013;176:92–99. doi: 10.1016/j.envpol.2012.12.032. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Delfino RJ, Tjoa T, Gillen DL, Staimer N, Polidori A, Arhami M, et al. Traffic-related air pollution and blood pressure in elderly subjects with coronary artery disease. Epidemiology. 2010;21(3):396–404. doi: 10.1097/EDE.0b013e3181d5e19b. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Department for Environment, Food and Rural Affairs (DEFRA). (2002). Survey of public attitudes to quality of life and to the environment. http://archive.defra.gov.uk/evidence/statistics/environment/pubatt/download/survey2001.pdf . Accessed 21 February 2015.
- Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. New England Journal of Medicine. 1993;329(24):1753–1759. doi: 10.1056/NEJM199312093292401. [ DOI ] [ PubMed ] [ Google Scholar ]
- Downs SH, Schindler C, Liu LJ, Keidel D, Bayer-Oglesby L, Brutsche MH, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. New England Journal of Medicine. 2007;357(23):2338–2347. doi: 10.1056/NEJMoa073625. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eenhuizen E, Gehring U, Wijga AH, Smit HA, Fischer PH, Brauer M, et al. Traffic related air pollution is related to interrupter resistance in four-year old children. European Respiratory Journal. 2013;41:1257–1263. doi: 10.1183/09031936.00020812. [ DOI ] [ PubMed ] [ Google Scholar ]
- Environmental Protection Agency (EPA). (2009). Integrated science assessment for particulate matter (final report). Washington, DC: United States Environmental Protection Agency. http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=216546#Download . Accessed 15 February 2015.
- Environmental Protection Agency (EPA). (2013). EPA and NIH announce the winning team in my air, my health challenge/winners developed a low cost, real time personal digital device that measures health effects of harmful air pollution. http://blog.epa.gov/science/2013/06/visualizing-the-invisible-with-the-my-air-my-health-challenge-winners/ . Accessed 12 February 2015.
- European Commission (EC). (2013). Attitudes of Europeans towards air quality. http://ec.europa.eu/public_opinion/flash/fl_360_en.pdf . Accessed 17 February 2015.
- European Environment Agency (EEA). (2014). Air quality in Europe. http://www.eea.europa.eu/publications/air-quality-in-europe-2014 . Accessed 9 February 2015.
- Filleul L, Rondeau V, Vandentorren S, Le Moual N, Cantagrel A, Annesi-Maesano I, et al. Twenty five year mortality and air pollution: Results from the French PAARC survey. Occupational and Environmental Medicine. 2005;62(7):453–460. doi: 10.1136/oem.2004.014746. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gasser M, Riediker M, Mueller L, Perrenoud A, Blank F, Gehr P, et al. Toxic effects of brake wear particles on epithelial lung cells in vitro. Particle and Fibre Toxicology. 2009;6:30. doi: 10.1186/1743-8977-6-30. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. American Journal of Respiratory and Critical Care Medicine. 2010;181(6):596–603. doi: 10.1164/rccm.200906-0858OC. [ DOI ] [ PubMed ] [ Google Scholar ]
- Godri KJ, Harrison RM, Evans T, Baker T, Dunster C, Mudway IS, et al. Increased oxidative burden associated with traffic component of ambient particulate matter at roadside and urban background school sites in London. RM, Evans T, Baker T, Dunster C, Mudway IS et al. 2011. PLoS ONE. 2011;6:e21961. doi: 10.1371/journal.pone.0021961. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gottipolu RR, Landa ER, Schladweiler MC, McGee JK, Ledbetter AD, Richards JH, et al. Cardiopulmonary responses of intratracheally instilled tire particles and constituent metal components. Inhalation Toxicology. 2008;20(5):473–484. doi: 10.1080/08958370701858427. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, et al. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence. Respirology. 2012;17(6):887–898. doi: 10.1111/j.1440-1843.2012.02195.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Graff DW, Cascio WE, Rappold A, Zhou H, Huang YC, Devlin RB, et al. Exposure to concentrated coarse air pollution particles causes mild cardiopulmonary effects in healthy young adults. Environmental Health Perspectives. 2009;117(7):1089–1094. doi: 10.1289/ehp0900558. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grigg J. Particulate matter exposure in children. Relevance to chronic obstructive pulmonary disease. Proceedings of the American Thoracic Society. 2009;6(7):564–569. doi: 10.1513/pats.200905-026RM. [ DOI ] [ PubMed ] [ Google Scholar ]
- Guxens M, Sunyer J. A review of epidemiological studies on neuropsychological effects of air pollution. Swiss Medical Weekly. 2012;141:w13322. doi: 10.57187/smw.2012.13322. [ DOI ] [ PubMed ] [ Google Scholar ]
- Health Effects Institute (HEI) National Particle Component Toxicity (NPACT) Review Panel. (2013a). NPACT Initiative. http://pubs.healtheffects.org/getfile.php?u=934 . Accessed 16 February 2015.
- Health Effects Institute (HEI) Panel on the Health Effects of Traffic-Related Air Pollution. Special Report 17. (2010). Traffic-related air pollution: a critical review of the literature on emissions, exposure and health effects. http://pubs.healtheffects.org/getfile.php?u=553 . Accessed 21 February 2015.
- Health Effects Institute (HEI) Review Panel on Ultrafine Particles. (2013b). Understanding the health effects of ambient ultrafine particles. http://pubs.healtheffects.org/getfile.php?u=893 . Accessed 16 February 2015.
- Hildebrandt K, Rückerl R, Koenig W, Schneider A, Pitz M, Heinrich J, et al. Short-term effects of air pollution: A panel study of blood markers in patients with chronic pulmonary disease. Particle and Fibre Toxicology. 2009;6:25. doi: 10.1186/1743-8977-6-25. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA. Association between mortality and indicators of traffic-related air pollution in the Netherlands: A cohort study. The Lancet. 2002;360(9341):1203–1209. doi: 10.1016/S0140-6736(02)11280-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation. 2007;116(5):489–496. doi: 10.1161/CIRCULATIONAHA.107.693622. [ DOI ] [ PubMed ] [ Google Scholar ]
- International Agency for Research on Cancer (IARC). (2012). Diesel engine exhaust carcinogenic. http://www.iarc.fr/en/media-centre/pr/2012/pdfs/pr213_E.pdf . Accessed 10 February 2015.
- IOM. (2006). Comparing estimated risks for air pollution with risks for other health effects. http://www.iom-world.org/pubs/IOM_TM0601.pdf . Accessed 10 February 2015.
- Ito K, Mathes R, Ross Z, Nádas A, Thurston G, Matte T. Fine particulate matter constituents associated with cardiovascular hospitalizations and mortality in New York City. Environmental Health Perspectives. 2011;119(4):467–473. doi: 10.1289/ehp.1002667. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Janssen NA, Brunekreef B, van Vliet P, Aarts F, Meliefste K, Harssema H, et al. The relationship between air pollution from heavy traffic and allergic sensitization, bronchial hyperresponsiveness, and respiratory symptoms in Dutch schoolchildren. Environmental Health Perspectives. 2003;111(12):1512–1518. doi: 10.1289/ehp.6243. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jedrychowski WA, Perera FP, Spengler JD, Mroz E, Stigter L, Flak E, et al. Intrauterine exposure to fine particulate matter as a risk factor for increased susceptibility to acute bronchopulmonary infections in early childhood. International Journal of Hygiene and Environmental Health. 2013;216(4):395–401. doi: 10.1016/j.ijheh.2012.12.014. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Katsouyanni K, Touloumi G, Samoli E, Gryparis A, Le Tertre A, Monopolis Y, et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: results from 29 European cities within the APHEA2 project. Epidemiology. 2001;12(5):521–531. doi: 10.1097/00001648-200109000-00011. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kelly FJ, Anderson HR, Armstrong B, Atkinson R, Barratt B, Beevers S, et al. Impact of the congestion charging scheme on air quality in London. Part 2. Analysis of the oxidative potential of particulate matter. Research Report. (Health Effects Institute) 2011;155:73–144. [ PubMed ] [ Google Scholar ]
- Kelly FJ, Fuller GW, Walton HA, Fussell JC. Monitoring air pollution: Use of early warning systems for public health. Respirology. 2012;17(1):7–19. doi: 10.1111/j.1440-1843.2011.02065.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kelly FJ, Fussell JC. Air pollution and airway disease. Clinical and Exerimental Allergy. 2011;41(8):1059–1071. doi: 10.1111/j.1365-2222.2011.03776.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kelly FJ, Fussell JC. Size, source and chemical composition as determinants of toxicity attributable to ambient particular matter. Atmospheric Environment. 2012;60:504–526. [ Google Scholar ]
- Kelly, F. J., & Fussell, J. C. (2015). Linking ambient particulate matter pollution effects with oxidative biology and immune responses. Annals of the New York Academy of Science , 1340 , 84–94. [ DOI ] [ PubMed ]
- Kim JJ, Huen K, Adams S, Smorodinsky S, Hoats A, Malig B, et al. Residential traffic and children’s respiratory health. Environmental Health Perspectives. 2008;116(9):1274–1279. doi: 10.1289/ehp.10735. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kim SY, Peel JL, Hannigan MP, Dutton SJ, Sheppard L, Clark ML, et al. The temporal lag structure of short-term associations of fine particulate matter chemical constituents and cardiovascular and respiratory hospitalizations. Environmental Health Perspectives. 2012;120(8):1094–1099. doi: 10.1289/ehp.1104721. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kramer U, Herder C, Sugiri D, Strassburger K, Schikowski T, Ranft U, et al. Traffic-related air pollution and incident type 2 diabetes: Results from the SALIA cohort study. Environmental Health Perspectives. 2010;118(9):1273–1279. doi: 10.1289/ehp.0901689. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, et al. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Research Report. (Health Effects Institute) 2009;140:5–114. [ PubMed ] [ Google Scholar ]
- Kreyling WG, Hirn S, Schleh C. Nanoparticles in the lung. Nature Biotechnology. 2010;28(12):1275–1276. doi: 10.1038/nbt.1735. [ DOI ] [ PubMed ] [ Google Scholar ]
- Künzli N, Jerrett M, Garcia-Esteban R, Basagaña X, Beckermann B, Gilliland F, et al. Ambient air pollution and the progression of atherosclerosis in adults. PLoS ONE. 2010;5(2):e9096. doi: 10.1371/journal.pone.0009096. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Künzli N, Jerrett M, Mack WJ, Beckerman B, LaBree L, Gilliland F, et al. Ambient air pollution and atherosclerosis in Los Angeles. Environmental Health Perspectives. 2005;113(2):201–206. doi: 10.1289/ehp.7523. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Latzin P, Röösli M, Huss A, Kuehni CE, Frey U. Air pollution during pregnancy and lung function in newborns: A birth cohort study. European Respiratory Journal. 2009;33(3):594–603. doi: 10.1183/09031936.00084008. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lepeule J, Laden F, Dockery D, Schwartz J. Chronic exposure to fine particles and mortality: An extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environmental Health Perspectives. 2012;120(7):965–970. doi: 10.1289/ehp.1104660. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lercher P, Schmitzberger R, Kofler W. Perceived traffic air pollution, associated behaviour and health in an alpine area. Science of the Total Environment. 1995;169(1–3):71–74. doi: 10.1016/0048-9697(95)04634-d. [ DOI ] [ PubMed ] [ Google Scholar ]
- Loeb LA. A mutator phenotype in cancer. Cancer Research. 2001;61(8):3230–3239. [ PubMed ] [ Google Scholar ]
- Logan WP. Mortality in the London fog incident, 1952. The Lancet. 1953;1(6755):336–338. doi: 10.1016/s0140-6736(53)91012-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- London Air Quality Network (LAQN). London air applications. http://www.londonair.org.uk/LondonAir/MobileApps/ . Accessed 13 February 2015.
- Lucking AJ, Lundback M, Mills NL, Faratian D, Barath SL, Pourazar J, et al. Diesel exhaust inhalation increases thrombus formation in man. European Heart Journal. 2008;29(24):3043–3051. doi: 10.1093/eurheartj/ehn464. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lundback M, Mills NL, Lucking A, Barath S, Donaldson K, Newby DE, et al. Experimental exposure to diesel exhaust increases arterial stiffness in man. Particle and Fibre Toxicology. 2009;6:7. doi: 10.1186/1743-8977-6-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Macintyre EA, Gehring U, Molter A, Fuertes E, Klümper C, Krämer U, et al. Air pollution and respiratory infections during early childhood: An analysis of 10 European birth cohorts within the escape project. Environmental Health Perspectives. 2013;122(1):107–113. doi: 10.1289/ehp.1306755. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mann JK, Balmes JR, Bruckner TA, Mortimer KM, Margolis HG, Pratt B, et al. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environmental Health Perspectives. 2010;118(10):1497–1502. doi: 10.1289/ehp.0901292. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mantecca P, Sancini G, Moschini E, Farina F, Gualtieri M, Rohr A, et al. Lung toxicity induced by intratracheal instillation of size-fractionated tire particles. Toxicology Letters. 2009;189(3):206–214. doi: 10.1016/j.toxlet.2009.05.023. [ DOI ] [ PubMed ] [ Google Scholar ]
- McDermott M, Srivastava R, Croskell S. Awareness of and compliance with air pollution advisories: A comparison of parents of asthmatics with other parents. Journal of Asthma. 2006;43(3):235–239. doi: 10.1080/02770900600567114. [ DOI ] [ PubMed ] [ Google Scholar ]
- Meister K, Johansson C, Forsberg B. Estimated short-term effects of coarse particles on daily mortality in Stockholm, Sweden. Environmental Health Perspectives. 2012;120(3):431–436. doi: 10.1289/ehp.1103995. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mills NL, Tornqvist H, Gonzalez MC, Vink E, Robinson SD, Söderberg S, et al. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. New England Journal of Medicine. 2007;357(11):1075–1082. doi: 10.1056/NEJMoa066314. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mills NL, Tornqvist H, Robinson SD, Gonzalez M, Darnley K, MacNee W, et al. Diesel exhaust inhalation causes vascular dysfunction and impaired endogenous fibrinolysis. Circulation. 2005;112(25):3930–3936. doi: 10.1161/CIRCULATIONAHA.105.588962. [ DOI ] [ PubMed ] [ Google Scholar ]
- Molter A, Agius RM, de Vocht F, Lindley S, Gerrard W, Lowe L, et al. Long-term Exposure to PM10 and NO2 in association with lung volume and airway resistance in the MAAS birth cohort. Environmental Health Perspectives. 2013;121(10):1232–1238. doi: 10.1289/ehp.1205961. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mudway IS, Stenfors N, Duggan ST, Roxborough H, Zielinski H, Marklund SL, et al. An in vitro and in vivo investigation of the effects of diesel exhaust on human airway lining fluid antioxidants. Archives of Biochemistry and Biophysics. 2004;423(1):200–212. doi: 10.1016/j.abb.2003.12.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- Naess Ø, Nafstad P, Aamodt G, Claussen B, Rosland P. Relation between concentration of air pollution and cause-specific mortality: Four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo, Norway. American Journal of Epidemiology. 2007;165(4):435–443. doi: 10.1093/aje/kwk016. [ DOI ] [ PubMed ] [ Google Scholar ]
- Neidell M, Kinney PL. Estimates of the association between ozone and asthma hospitalizations that account for behavioural responses to air quality information. Environmental Science & Policy. 2010;13(2):97–103. [ Google Scholar ]
- Nwokoro C, Ewin C, Harrison C, Ibrahim M, Dundas I, Dickson I. Cycling to work in London and inhaled dose of black carbon. European Respiratory Journal. 2012;40(5):1091–1097. doi: 10.1183/09031936.00195711. [ DOI ] [ PubMed ] [ Google Scholar ]
- Oakes M, Ingall ED, Lai B, Shafer MM, Hays MD, Liu ZG, et al. Iron solubility related to particle sulfur content in source emission and ambient fine particles. Environmental Science and Technology. 2012;46(12):6637–6644. doi: 10.1021/es300701c. [ DOI ] [ PubMed ] [ Google Scholar ]
- OECD (Organisation for Economic Co-operation and development). (2014). The cost of air pollution. Health impacts of road transport. http://www.keepeek.com/Digital-Asset-Management/oecd/environment/the-cost-of-air-pollution_9789264210448-en#page1 . Accessed 9 February 2015.
- Ostro B, Broadwin R, Green S, Feng WY, Lipsett M. Fine particulate air pollution and mortality in nine California counties: Results from CALFINE. Environmental Health Perspectives. 2006;114(1):29–33. doi: 10.1289/ehp.8335. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ostro B, Lipsett M, Reynolds P, Goldberg D, Hertz A, Garcia C, et al. Long-term exposure to constituents of fine particulate air pollution and mortality: Results from the California Teachers Study. Environmental Health Perspectives. 2010;118(3):363–369. doi: 10.1289/ehp.0901181. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Palli D, Saieva C, Munnia A, Peluso M, Grechi D, Zanna I, et al. DNA adducts and PM(10) exposure in traffic-exposed workers and urban residents from the EPIC-Florence City study. Science of the Total Environment. 2008;403(1–3):105–112. doi: 10.1016/j.scitotenv.2008.05.041. [ DOI ] [ PubMed ] [ Google Scholar ]
- Pedersen M, Wichmann J, Autrup H, Dang DA, Decordier I, Hvidberg M, et al. Increased micronuclei and bulky DNA adducts in cord blood after maternal exposures to traffic-related air pollution. Environmental Research. 2009;109(8):1012–1020. doi: 10.1016/j.envres.2009.08.011. [ DOI ] [ PubMed ] [ Google Scholar ]
- Peng RD, Chang HH, Bell ML, McDermott A, Zeger SL, Samet JM, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. Journal of the American Medical Association. 2008;299(18):2172–2179. doi: 10.1001/jama.299.18.2172. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peretz A, Peck EC, Bammler TK, Beyer RP, Sullivan JH, Trenga CA, et al. Diesel exhaust inhalation and assessment of peripheral blood mononuclear cell gene transcription effects: An exploratory study of healthy human volunteers. Inhalation Toxicology. 2007;19(14):1107–1119. doi: 10.1080/08958370701665384. [ DOI ] [ PubMed ] [ Google Scholar ]
- Piro FN, Madsen C, Naess O, Nafstad P, Claussen B. A comparison of self reported air pollution problems and GIS-modeled levels of air pollution in people with and without chronic diseases. Environmental Health. 2008;7:9. doi: 10.1186/1476-069X-7-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pope CA, III, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. New England Journal of Medicine. 2009;360(4):376–386. doi: 10.1056/NEJMsa0805646. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pourazar J, Frew AJ, Blomberg A, Helleday R, Kelly FJ, Wilson S, et al. Diesel exhaust exposure enhances the expression of IL-13 in the bronchial epithelium of healthy subjects. Respiratory Medicine. 2004;98(9):821–825. doi: 10.1016/j.rmed.2004.02.025. [ DOI ] [ PubMed ] [ Google Scholar ]
- Pourazar J, Mudway IS, Samet JM, Helleday R, Blomberg A, Wilson SJ, et al. Diesel exhaust activates redox-sensitive transcription factors and kinases in human airways. American Journal of Physiology. Lung Cellular and Molecular Physiology. 2005;289(5):L724–L730. doi: 10.1152/ajplung.00055.2005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Pratt, M., Sarmiento, O. L., Montes, F., Ogilvie, D., Marcus, B. H., Perez, L. G., et al. for the Lancet Physical Activity Series Working Group. (2012). The implications of megatrends in information and communication technology and transportation for changes in global physical activity. Lancet, 380 (9838), 282–293. [ DOI ] [ PMC free article ] [ PubMed ]
- Proietti E, Röösli M, Frey U, Latzin P. Air pollution during pregnancy and neonatal outcome: A review. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2013;26(1):9–23. doi: 10.1089/jamp.2011.0932. [ DOI ] [ PubMed ] [ Google Scholar ]
- Public Health England (PHE). (2014). Estimating local mortality burdens associated with particulate air pollution. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/332854/PHE_CRCE_010.pdf . Accessed 10 February 2015.
- Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F. Are particulate matter exposures associated with risk of type 2 diabetes? Environmental Health Perspectives. 2011;119(3):384–389. doi: 10.1289/ehp.1002344. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Puett RC, Hart JE, Suh H, Mittleman M, Laden F, et al. Particulate matter exposures, mortality, and cardiovascular disease in the health professionals follow-up study. Environmental Health Perspectives. 2011;119(8):1130–1135. doi: 10.1289/ehp.1002921. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Puett RC, Hart JE, Yanosky JD, Paciorek C, Schwartz J, Suh H, et al. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the Nurses’ Health Study. Environmental Health Perspectives. 2009;117(11):1697–1701. doi: 10.1289/ehp.0900572. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Qiu H, Yu IT, Tian L, Wang X, Tse LA, Tam W, et al. Effects of coarse particulate matter on emergency hospital admissions for respiratory diseases: A time-series analysis in Hong Kong. Environmental Health Perspectives. 2012;120(4):572–576. doi: 10.1289/ehp.1104002. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Quality of urban air review group. (1996). Airborne particulate matter in the UK. http://uk-air.defra.gov.uk/assets/documents/reports/empire/quarg/quarg_11.pdf . Accessed 18 February 2015.
- Raaschou-Nielsen O, Sørensen M, Ketzel M, Hertel O, Loft S, Tjønneland A, et al. Long-term exposure to traffic-related air pollution and diabetes-associated mortality: A cohort study. Diabetologia. 2013;56(1):36–46. doi: 10.1007/s00125-012-2698-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ranft U, Schikowski T, Sugiri D, Krutmann J, Krämer U, et al. Long-term exposure to traffic-related particulate matter impairs cognitive function in the elderly. Environmental Research. 2009;109(8):1004–1011. doi: 10.1016/j.envres.2009.08.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- Riediker M, Devlin RB, Griggs TR, Herbst MC, Bromberg PA, Williams RW, et al. Cardiovascular effects in patrol officers are associated with fine particulate matter from brake wear and engine emissions. Particle and Fibre Toxicology. 2004;1:2. doi: 10.1186/1743-8977-1-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ritz B, Wilhelm M. Ambient air pollution and adverse birth outcomes: methodologic issues in an emerging field. Basic & Clinical Pharmacology & Toxicology. 2008;102(2):182–190. doi: 10.1111/j.1742-7843.2007.00161.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rotko T, Oglesby L, Künzli N, Carrer P, Nieuwenhuijsen MJ, Jantunen M. Determinants of perceived air pollution annoyance and association between annoyance scores and air pollution (PM2.5, NO2) concentrations in the European EXPOLIS study. Atmospheric Environment. 2002;36(29):4593–4602. [ Google Scholar ]
- Rückerl R, Schneider A, Breitner S, Cyrys J, Peters A, et al. Health effects of particulate air pollution: A review of epidemiological evidence. Inhalation Toxicology. 2011;23(10):555–592. doi: 10.3109/08958378.2011.593587. [ DOI ] [ PubMed ] [ Google Scholar ]
- Salvi SS, Blomberg A, Rudell B, Kelly F, Sandström T, Holgate ST, Frew A, et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. American Journal of Respiratory and Critical Care Medicine. 1999;159(3):702–709. doi: 10.1164/ajrccm.159.3.9709083. [ DOI ] [ PubMed ] [ Google Scholar ]
- Salvi SS, Nordenhall C, Blomberg A, Rudell B, Pourazar J, Kelly FJ, et al. Acute exposure to diesel exhaust increases IL-8 and GRO-α production in healthy human airways. American Journal of Respiratory and Critical Care Medicine. 2000;161((2 pt1)):550–557. doi: 10.1164/ajrccm.161.2.9905052. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sapkota A, Chelikowsky AP, Nachman KE, Cohen AJ, Ritz B, et al. Exposure to particulate matter and adverse birth outcomes: A comprehensive review and meta-analysis. Air Quality, Atmosphere and Health. 2012;5(4):369–381. [ Google Scholar ]
- Schindler C, Keidel D, Gerbase MW, Zemp E, Bettschart R, Brändli O, et al. Improvements in PM10 exposure and reduced rates of respiratory symptoms in a cohort of Swiss adults (SAPALDIA) American Journal of Respiratory and Critical Care Medicine. 2009;179(7):579–587. doi: 10.1164/rccm.200803-388OC. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schwartz J, Dockery DW. Increased mortality in Philadelphia associated with daily air pollution concentrations. American Review of Respiratory Diseases. 1992;145(3):600–604. doi: 10.1164/ajrccm/145.3.600. [ DOI ] [ PubMed ] [ Google Scholar ]
- Semenza JC, Wilson DJ, Parra J, Bontempo BD, Sailor DJ, George LA. Public perception and behaviour change in relationship to hot weather and air pollution. Environmental Research. 2008;107(3):401–411. doi: 10.1016/j.envres.2008.03.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Shooter D, Brimblecombe P. Air quality indexing. International Journal of Environmental Pollution. 2009;36(1–3):305–323. [ Google Scholar ]
- Son JY, Lee JT, Kim KH, Jung K, Bell ML. Characterization of fine particulate matter and associations between particulate chemical constituents and mortality in Seoul, Korea. Environmental Health Perspectives. 2012;120(6):872–878. doi: 10.1289/ehp.1104316. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spira-Cohen A, Chen LC, Kendall M, Lall R, Thurston GD. Personal exposures to traffic-related air pollution and acute respiratory health among bronx school-children with asthma. Environmental Health Perspectives. 2011;119(4):559–565. doi: 10.1289/ehp.1002653. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stenfors N, Nordenhall C, Salvi SS, Mudway I, Söderberg M, Blomberg A, et al. Different airway inflammatory responses in asthmatic and healthy humans exposed to diesel. European Respiratory Journal. 2004;23(1):82–86. doi: 10.1183/09031936.03.00004603. [ DOI ] [ PubMed ] [ Google Scholar ]
- Thompson RC, Allam AH, Lombardi GP, Wann LS, Sutherland ML, Sutherland JD, et al. Atherosclerosis across 4000 years of human history: The Horus study of four ancient populations. The Lancet. 2013;381(9873):1211–1222. doi: 10.1016/S0140-6736(13)60598-X. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tornqvist H, Mills NL, Gonzalez M, Miller MR, Robinson SD, Megson IL, et al. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. American Journal of Respiratory and Critical Care Medicine. 2007;176(4):395–400. doi: 10.1164/rccm.200606-872OC. [ DOI ] [ PubMed ] [ Google Scholar ]
- van der Gon HA, Gerlofs-Nijland ME, Gehrig R, Gustafsson M, Janssen N, Harrison RM, et al. The policy relevance of wear emissions from road transport, now and in the future—an international workshop report and consensus statement. Journal of the Air and Waste Management Association. 2013;63(2):136–149. doi: 10.1080/10962247.2012.741055. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wegesser TC, Pinkerton KE, Last JA. California wildfires of 2008: Coarse and fine particulate matter toxicity. Environmental Health Perspectives. 2009;117(6):893–897. doi: 10.1289/ehp.0800166. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weichenthal S. Selected physiological effects of ultrafine particles in acute cardiovascular morbidity. Environmental Research. 2012;115:26–36. doi: 10.1016/j.envres.2012.03.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wen X-J, Balluz L, Mokdad A. Association between media alerts of air quality index and change of outdoor activity among adult asthma in six states, BRFSS, 2005. Journal of Community Health. 2009;34(1):40–46. doi: 10.1007/s10900-008-9126-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wilkins ET. Air pollution aspects of the London fog of December 1952. Quarterly Journal of the Royal Meteorological Society. 1954;80(344):267–271. [ Google Scholar ]
- World Health Organisation (WHO). (2014). Burden of disease from air pollution. http://www.who.int/phe/health_topics/outdoorair/databases/FINAL_HAP_AAP_BoD_24March2014.pdf?ua=1 . Accessed 9 February 2015.
- World Health Organisation (WHO) Regional Office for Europe. (2006). Air quality guidelines global update 2005: Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Copenhagen. http://www.euro.who.int/__data/assets/pdf_file/0005/78638/E90038.pdf . Accessed 9 February 2015.
- World Health Organisation (WHO) Regional Office for Europe. (2012). Health effects of black carbon. http://www.euro.who.int/__data/assets/pdf_file/0004/162535/e96541.pdf?ua=1 . Accessed 16 February 2015.
- World Health Organisation (WHO) Regional Office for Europe. (2013a). Review of evidence on health aspects of air pollution—REVIHAAP project, technical report. http://www.euro.who.int/__data/assets/pdf_file/0004/193108/REVIHAAP-Final-technical-report-final-version.pdf?ua=1 . Accessed 16 February 2015. [ PubMed ]
- World Health Organisation (WHO) Regional Office for Europe. (2013b). Health effects of particulate matter: Policy implications for countries in Eastern Europe, Caucasus and central Asia. http://www.euro.who.int/__data/assets/pdf_file/0006/189051/Health-effects-of-particulate-matter-final-Eng.pdf . Accessed 9 February 2015.
- Yanosky JD, Tonne CC, Beevers SD, Wilkinson P, Kelly FJ. Modeling exposures to the oxidative potential of PM10. Environmental Science and Technology. 2012;46(14):7612–7620. doi: 10.1021/es3010305. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yen IH, Yelin EH, Katz P, Eisner MD, Blanc PD. Perceived neighborhood problems and quality of life, physical functioning, and depressive symptoms among adults with asthma. American Journal of Public Health. 2006;96(5):873–879. doi: 10.2105/AJPH.2004.059253. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zanobetti A, Schwartz J. The effect of fine and coarse particulate air pollution on mortality: A national analysis. Environmental Health Perspectives. 2009;117(6):898–903. doi: 10.1289/ehp.0800108. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zimmerman MR, Yeatman GW, Spinz H. Examination of an Aleutian mummy. Bulletin of the New York Academy of Medicine. 1971;47(1):80–103. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zweifel L, Böni T, Ruhli FJ. Evidence-based palaeopathology: Meta-analysis of PubMed-listed scientific studies on ancient Egyptian mummies. Journal of Comparative Human Biology. 2009;60(5):405–427. doi: 10.1016/j.jchb.2009.07.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.8 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 October 2021
Clean air for a sustainable world
Nature Communications volume 12 , Article number: 5824 ( 2021 ) Cite this article
21k Accesses
7 Citations
15 Altmetric
Metrics details
Air pollution is a cause of disease for millions around the world and now more than ever urgent action is required to tackle the burden of its impacts. Doing so will not only improve both life expectancy and quality of life, but will also lead to a more just and sustainable world.
Recently, we announced that we will publish a new series of collections focused on issues related to the Sustainable Development Goals (SDGs). We start this series with a multidisciplinary collection on air pollution. As tackling air pollution is not one of the core SDGs, this may seem like an unusual choice. It is, however, a pressing environmental hazard affecting an ever increasing part of the world’s population. Currently, 91% of the world’s population live in locations where pollution levels exceed WHO guidelines, and in a recent announcement the WHO have further cut the recommended limits. Air pollution kills around 6.7 million people per year mainly through respiratory and cardiovascular diseases 1 , and has significant impacts on mental health. The main pollutants are sourced from fossil fuel combustion for transport, industry, agriculture and cooking stoves and, therefore, air pollution is linked directly with fulfilling many of our basic needs. As the SDGs aim to tackle the issue of how humanity can live sustainably, it is thus no surprise that addressing air pollution is related to the SDGs in many different ways. Promoting specific SDGs will lead to improved air quality as a side-effect, while reducing emissions will also progress a number of SDGs directly.
The high air pollution levels that we live with today is another demonstration of how our unsustainable lifestyles are one of the key challenges that needs to be overcome to create a more just and liveable world, which is the ultimate goal of the SDGs.

Although air pollution is a global issue, exposure is often not distributed equally. Industrial processes related to the production, trade and consumption of goods is a key source of air pollution. Much of this pollution is released in low- and middle-income countries while they manufacture goods that are traded abroad, allowing rich countries to outsource the air pollution and health effects of their consumption. Hence, global implementation of responsible consumption and sustainable production practices—the focus of SDG9 (“Industry, Innovation and Infrastructure”) and SDG12 (“Responsible Consumption and Production”)—will be key to reduce this unequal responsibility and exposure to dangerous environmental conditions.
Inequality in exposure does not only occur at an international level, but also within countries. Systematic and historical forms of discrimination often translate into higher exposure levels and, hence, enhanced health burdens to marginalized groups around the world. This is probably best studied in the US, where people of colour are shown to live under poorer air quality, independent of other factors like income 2 . In a commentary for our collection Viniece Jennings highlights that whilst green infrastructure has the potential to reduce air pollution, unequal access can limit improvements for marginalised communities 3 . While we often think of air pollution as an outdoor issue, much of the exposure to harmful particles actually happens inside houses. Household air pollution is mainly related to cooking, heating or lighting, often through the combustion of solid fuels. This exposure affects women and children disproportionately, especially in the developing world 4 . Consequently, targeting SDG10 (“Reduce inequality within and among countries”) and SDG 7 (“Ensure access to affordable, reliable, sustainable and modern energy for all.”) will be of vital importance to tackle embedded inequalities within and among countries to reduce air pollution exposure.
Air pollution and climate change are closely intertwined as they share the same root cause of human emissions. Even though ambitious climate mitigation policies do not come for free, they will in many cases also lead to improved air quality and lower health costs. The societal costs of air pollution avoided through reduced exposure levels as a result of climate mitigation measures alone are thought to outweigh the initial costs of these policies 5 . Air pollution also physically interacts with the climate system; particles in the atmosphere affect surface temperatures as well as clouds and precipitation. Climate change thus has the potential to “worsen air pollution, even in areas where it has been improving”, as pointed out by Denise Mauzarell in a Q&A for our Clean Air collection 6 . An example of this are the dangerous pollutants released by wildfires that are expected to become ever more frequent and intense in many parts of the world.
Similarly, to climate mitigation, improving air quality depends on strict and ambitious regulatory policies and controls, which must be implemented equitably. In this regard, there are reasons to be optimistic, as strict air quality policies like the Clean Air Act in the US and similar policies in Europe have resulted in reductions in pollution since the 1970s even though levels are still too high and continued efforts are crucial. These efforts show that ambitious policy supported by technological advances like improved filtering and modernization can be successful. These efforts should not only be done at national levels, but also need international collaboration, technology and knowledge transfer in order to acknowledge the shared responsibilities of air pollution. As part of the Clean Air collection we highlight papers Nature Communications has published that look at how policy and technology can be part of the solution to air pollution.
The high air pollution levels that we live with today is another demonstration of how our unsustainable lifestyles are one of the key challenges that needs to be overcome to create a more just and liveable world, which is the ultimate goal of the SDGs. Of course, reducing air pollution on its own will not meet the aims of all the other SDGs. Still, it is an illustrative example of how an interdisciplinary focus on a measurable and technologically approachable issue can help to also achieve other goals. It is in this spirit that our collection brings together research from different disciplines, such as applied scientists, economists, political scientists, health scientists and climate scientists as it is this interdisciplinary collaboration that Nature Communications wants to support will be vital in informing policy and decision makers. We envision that our collection on Clean Air will continue to grow and we welcome submissions across disciplines in this area.
GBD Global Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396 , 1223–1249 (2020).
Tessum, C. W. et al. PM 2.5 polluters disproportionately and systemically affect people of color in the United States. Sci. Adv. 7 , 18 (2021).
Jennings, V., Reid C. E., & Fuller C. H. Green infrastructure can limit but not solve air pollution injustice. Nat. Commun. 12 , 4681 (2021).
Gordon, S. B., et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2 , 823–860 (2014).
Vandyck, T. et al. Air quality co-benefits for human health and agriculture counterbalance costs to meet Paris Agreement pledges. Nat. Commun. 9 , 4939 (2018).
Nat. Commun. (2021). https://doi.org/10.1038/s41467-021-25491-w .
Download references
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Clean air for a sustainable world. Nat Commun 12 , 5824 (2021). https://doi.org/10.1038/s41467-021-25885-w
Download citation
Published : 04 October 2021
DOI : https://doi.org/10.1038/s41467-021-25885-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Processing nomex nanofibers by ionic solution blow-spinning for efficient high-temperature exhausts treatment.
- Zekun Cheng
- Haiyang Wang
Advanced Fiber Materials (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
REVIEW article
Environmental and health impacts of air pollution: a review.

- 1 Delphis S.A., Kifisia, Greece
- 2 Laboratory of Hygiene and Environmental Protection, Faculty of Medicine, Democritus University of Thrace, Alexandroupolis, Greece
- 3 Centre Hospitalier Universitaire Vaudois (CHUV), Service de Médicine Interne, Lausanne, Switzerland
- 4 School of Social and Political Sciences, University of Glasgow, Glasgow, United Kingdom
One of our era's greatest scourges is air pollution, on account not only of its impact on climate change but also its impact on public and individual health due to increasing morbidity and mortality. There are many pollutants that are major factors in disease in humans. Among them, Particulate Matter (PM), particles of variable but very small diameter, penetrate the respiratory system via inhalation, causing respiratory and cardiovascular diseases, reproductive and central nervous system dysfunctions, and cancer. Despite the fact that ozone in the stratosphere plays a protective role against ultraviolet irradiation, it is harmful when in high concentration at ground level, also affecting the respiratory and cardiovascular system. Furthermore, nitrogen oxide, sulfur dioxide, Volatile Organic Compounds (VOCs), dioxins, and polycyclic aromatic hydrocarbons (PAHs) are all considered air pollutants that are harmful to humans. Carbon monoxide can even provoke direct poisoning when breathed in at high levels. Heavy metals such as lead, when absorbed into the human body, can lead to direct poisoning or chronic intoxication, depending on exposure. Diseases occurring from the aforementioned substances include principally respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and also lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases. Last but not least, climate change resulting from environmental pollution affects the geographical distribution of many infectious diseases, as do natural disasters. The only way to tackle this problem is through public awareness coupled with a multidisciplinary approach by scientific experts; national and international organizations must address the emergence of this threat and propose sustainable solutions.
Approach to the Problem
The interactions between humans and their physical surroundings have been extensively studied, as multiple human activities influence the environment. The environment is a coupling of the biotic (living organisms and microorganisms) and the abiotic (hydrosphere, lithosphere, and atmosphere).
Pollution is defined as the introduction into the environment of substances harmful to humans and other living organisms. Pollutants are harmful solids, liquids, or gases produced in higher than usual concentrations that reduce the quality of our environment.
Human activities have an adverse effect on the environment by polluting the water we drink, the air we breathe, and the soil in which plants grow. Although the industrial revolution was a great success in terms of technology, society, and the provision of multiple services, it also introduced the production of huge quantities of pollutants emitted into the air that are harmful to human health. Without any doubt, the global environmental pollution is considered an international public health issue with multiple facets. Social, economic, and legislative concerns and lifestyle habits are related to this major problem. Clearly, urbanization and industrialization are reaching unprecedented and upsetting proportions worldwide in our era. Anthropogenic air pollution is one of the biggest public health hazards worldwide, given that it accounts for about 9 million deaths per year ( 1 ).
Without a doubt, all of the aforementioned are closely associated with climate change, and in the event of danger, the consequences can be severe for mankind ( 2 ). Climate changes and the effects of global planetary warming seriously affect multiple ecosystems, causing problems such as food safety issues, ice and iceberg melting, animal extinction, and damage to plants ( 3 , 4 ).
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. Short-term exposure to air pollutants is closely related to COPD (Chronic Obstructive Pulmonary Disease), cough, shortness of breath, wheezing, asthma, respiratory disease, and high rates of hospitalization (a measurement of morbidity).
The long-term effects associated with air pollution are chronic asthma, pulmonary insufficiency, cardiovascular diseases, and cardiovascular mortality. According to a Swedish cohort study, diabetes seems to be induced after long-term air pollution exposure ( 5 ). Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ).
National reports have mentioned the increased risk of morbidity and mortality ( 1 ). These studies were conducted in many places around the world and show a correlation between daily ranges of particulate matter (PM) concentration and daily mortality. Climate shifts and global planetary warming ( 3 ) could aggravate the situation. Besides, increased hospitalization (an index of morbidity) has been registered among the elderly and susceptible individuals for specific reasons. Fine and ultrafine particulate matter seems to be associated with more serious illnesses ( 6 ), as it can invade the deepest parts of the airways and more easily reach the bloodstream.
Air pollution mainly affects those living in large urban areas, where road emissions contribute the most to the degradation of air quality. There is also a danger of industrial accidents, where the spread of a toxic fog can be fatal to the populations of the surrounding areas. The dispersion of pollutants is determined by many parameters, most notably atmospheric stability and wind ( 6 ).
In developing countries ( 7 ), the problem is more serious due to overpopulation and uncontrolled urbanization along with the development of industrialization. This leads to poor air quality, especially in countries with social disparities and a lack of information on sustainable management of the environment. The use of fuels such as wood fuel or solid fuel for domestic needs due to low incomes exposes people to bad-quality, polluted air at home. It is of note that three billion people around the world are using the above sources of energy for their daily heating and cooking needs ( 8 ). In developing countries, the women of the household seem to carry the highest risk for disease development due to their longer duration exposure to the indoor air pollution ( 8 , 9 ). Due to its fast industrial development and overpopulation, China is one of the Asian countries confronting serious air pollution problems ( 10 , 11 ). The lung cancer mortality observed in China is associated with fine particles ( 12 ). As stated already, long-term exposure is associated with deleterious effects on the cardiovascular system ( 3 , 5 ). However, it is interesting to note that cardiovascular diseases have mostly been observed in developed and high-income countries rather than in the developing low-income countries exposed highly to air pollution ( 13 ). Extreme air pollution is recorded in India, where the air quality reaches hazardous levels. New Delhi is one of the more polluted cities in India. Flights in and out of New Delhi International Airport are often canceled due to the reduced visibility associated with air pollution. Pollution is occurring both in urban and rural areas in India due to the fast industrialization, urbanization, and rise in use of motorcycle transportation. Nevertheless, biomass combustion associated with heating and cooking needs and practices is a major source of household air pollution in India and in Nepal ( 14 , 15 ). There is spatial heterogeneity in India, as areas with diverse climatological conditions and population and education levels generate different indoor air qualities, with higher PM 2.5 observed in North Indian states (557–601 μg/m 3 ) compared to the Southern States (183–214 μg/m 3 ) ( 16 , 17 ). The cold climate of the North Indian areas may be the main reason for this, as longer periods at home and more heating are necessary compared to in the tropical climate of Southern India. Household air pollution in India is associated with major health effects, especially in women and young children, who stay indoors for longer periods. Chronic obstructive respiratory disease (CORD) and lung cancer are mostly observed in women, while acute lower respiratory disease is seen in young children under 5 years of age ( 18 ).
Accumulation of air pollution, especially sulfur dioxide and smoke, reaching 1,500 mg/m3, resulted in an increase in the number of deaths (4,000 deaths) in December 1952 in London and in 1963 in New York City (400 deaths) ( 19 ). An association of pollution with mortality was reported on the basis of monitoring of outdoor pollution in six US metropolitan cities ( 20 ). In every case, it seems that mortality was closely related to the levels of fine, inhalable, and sulfate particles more than with the levels of total particulate pollution, aerosol acidity, sulfur dioxide, or nitrogen dioxide ( 20 ).
Furthermore, extremely high levels of pollution are reported in Mexico City and Rio de Janeiro, followed by Milan, Ankara, Melbourne, Tokyo, and Moscow ( 19 ).
Based on the magnitude of the public health impact, it is certain that different kinds of interventions should be taken into account. Success and effectiveness in controlling air pollution, specifically at the local level, have been reported. Adequate technological means are applied considering the source and the nature of the emission as well as its impact on health and the environment. The importance of point sources and non-point sources of air pollution control is reported by Schwela and Köth-Jahr ( 21 ). Without a doubt, a detailed emission inventory must record all sources in a given area. Beyond considering the above sources and their nature, topography and meteorology should also be considered, as stated previously. Assessment of the control policies and methods is often extrapolated from the local to the regional and then to the global scale. Air pollution may be dispersed and transported from one region to another area located far away. Air pollution management means the reduction to acceptable levels or possible elimination of air pollutants whose presence in the air affects our health or the environmental ecosystem. Private and governmental entities and authorities implement actions to ensure the air quality ( 22 ). Air quality standards and guidelines were adopted for the different pollutants by the WHO and EPA as a tool for the management of air quality ( 1 , 23 ). These standards have to be compared to the emissions inventory standards by causal analysis and dispersion modeling in order to reveal the problematic areas ( 24 ). Inventories are generally based on a combination of direct measurements and emissions modeling ( 24 ).
As an example, we state here the control measures at the source through the use of catalytic converters in cars. These are devices that turn the pollutants and toxic gases produced from combustion engines into less-toxic pollutants by catalysis through redox reactions ( 25 ). In Greece, the use of private cars was restricted by tracking their license plates in order to reduce traffic congestion during rush hour ( 25 ).
Concerning industrial emissions, collectors and closed systems can keep the air pollution to the minimal standards imposed by legislation ( 26 ).
Current strategies to improve air quality require an estimation of the economic value of the benefits gained from proposed programs. These proposed programs by public authorities, and directives are issued with guidelines to be respected.
In Europe, air quality limit values AQLVs (Air Quality Limit Values) are issued for setting off planning claims ( 27 ). In the USA, the NAAQS (National Ambient Air Quality Standards) establish the national air quality limit values ( 27 ). While both standards and directives are based on different mechanisms, significant success has been achieved in the reduction of overall emissions and associated health and environmental effects ( 27 ). The European Directive identifies geographical areas of risk exposure as monitoring/assessment zones to record the emission sources and levels of air pollution ( 27 ), whereas the USA establishes global geographical air quality criteria according to the severity of their air quality problem and records all sources of the pollutants and their precursors ( 27 ).
In this vein, funds have been financing, directly or indirectly, projects related to air quality along with the technical infrastructure to maintain good air quality. These plans focus on an inventory of databases from air quality environmental planning awareness campaigns. Moreover, pollution measures of air emissions may be taken for vehicles, machines, and industries in urban areas.
Technological innovation can only be successful if it is able to meet the needs of society. In this sense, technology must reflect the decision-making practices and procedures of those involved in risk assessment and evaluation and act as a facilitator in providing information and assessments to enable decision makers to make the best decisions possible. Summarizing the aforementioned in order to design an effective air quality control strategy, several aspects must be considered: environmental factors and ambient air quality conditions, engineering factors and air pollutant characteristics, and finally, economic operating costs for technological improvement and administrative and legal costs. Considering the economic factor, competitiveness through neoliberal concepts is offering a solution to environmental problems ( 22 ).
The development of environmental governance, along with technological progress, has initiated the deployment of a dialogue. Environmental politics has created objections and points of opposition between different political parties, scientists, media, and governmental and non-governmental organizations ( 22 ). Radical environmental activism actions and movements have been created ( 22 ). The rise of the new information and communication technologies (ICTs) are many times examined as to whether and in which way they have influenced means of communication and social movements such as activism ( 28 ). Since the 1990s, the term “digital activism” has been used increasingly and in many different disciplines ( 29 ). Nowadays, multiple digital technologies can be used to produce a digital activism outcome on environmental issues. More specifically, devices with online capabilities such as computers or mobile phones are being used as a way to pursue change in political and social affairs ( 30 ).
In the present paper, we focus on the sources of environmental pollution in relation to public health and propose some solutions and interventions that may be of interest to environmental legislators and decision makers.
Sources of Exposure
It is known that the majority of environmental pollutants are emitted through large-scale human activities such as the use of industrial machinery, power-producing stations, combustion engines, and cars. Because these activities are performed at such a large scale, they are by far the major contributors to air pollution, with cars estimated to be responsible for approximately 80% of today's pollution ( 31 ). Some other human activities are also influencing our environment to a lesser extent, such as field cultivation techniques, gas stations, fuel tanks heaters, and cleaning procedures ( 32 ), as well as several natural sources, such as volcanic and soil eruptions and forest fires.
The classification of air pollutants is based mainly on the sources producing pollution. Therefore, it is worth mentioning the four main sources, following the classification system: Major sources, Area sources, Mobile sources, and Natural sources.
Major sources include the emission of pollutants from power stations, refineries, and petrochemicals, the chemical and fertilizer industries, metallurgical and other industrial plants, and, finally, municipal incineration.
Indoor area sources include domestic cleaning activities, dry cleaners, printing shops, and petrol stations.
Mobile sources include automobiles, cars, railways, airways, and other types of vehicles.
Finally, natural sources include, as stated previously, physical disasters ( 33 ) such as forest fire, volcanic erosion, dust storms, and agricultural burning.
However, many classification systems have been proposed. Another type of classification is a grouping according to the recipient of the pollution, as follows:
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2 , NO, NO 2 , SO 3 , etc.
Water pollution is organic and inorganic charge and biological charge ( 10 ) at high levels that affect the water quality ( 34 , 35 ).
Soil pollution occurs through the release of chemicals or the disposal of wastes, such as heavy metals, hydrocarbons, and pesticides.
Air pollution can influence the quality of soil and water bodies by polluting precipitation, falling into water and soil environments ( 34 , 36 ). Notably, the chemistry of the soil can be amended due to acid precipitation by affecting plants, cultures, and water quality ( 37 ). Moreover, movement of heavy metals is favored by soil acidity, and metals are so then moving into the watery environment. It is known that heavy metals such as aluminum are noxious to wildlife and fishes. Soil quality seems to be of importance, as soils with low calcium carbonate levels are at increased jeopardy from acid rain. Over and above rain, snow and particulate matter drip into watery ' bodies ( 36 , 38 ).
Lastly, pollution is classified following type of origin:
Radioactive and nuclear pollution , releasing radioactive and nuclear pollutants into water, air, and soil during nuclear explosions and accidents, from nuclear weapons, and through handling or disposal of radioactive sewage.
Radioactive materials can contaminate surface water bodies and, being noxious to the environment, plants, animals, and humans. It is known that several radioactive substances such as radium and uranium concentrate in the bones and can cause cancers ( 38 , 39 ).
Noise pollution is produced by machines, vehicles, traffic noises, and musical installations that are harmful to our hearing.
The World Health Organization introduced the term DALYs. The DALYs for a disease or health condition is defined as the sum of the Years of Life Lost (YLL) due to premature mortality in the population and the Years Lost due to Disability (YLD) for people living with the health condition or its consequences ( 39 ). In Europe, air pollution is the main cause of disability-adjusted life years lost (DALYs), followed by noise pollution. The potential relationships of noise and air pollution with health have been studied ( 40 ). The study found that DALYs related to noise were more important than those related to air pollution, as the effects of environmental noise on cardiovascular disease were independent of air pollution ( 40 ). Environmental noise should be counted as an independent public health risk ( 40 ).
Environmental pollution occurs when changes in the physical, chemical, or biological constituents of the environment (air masses, temperature, climate, etc.) are produced.
Pollutants harm our environment either by increasing levels above normal or by introducing harmful toxic substances. Primary pollutants are directly produced from the above sources, and secondary pollutants are emitted as by-products of the primary ones. Pollutants can be biodegradable or non-biodegradable and of natural origin or anthropogenic, as stated previously. Moreover, their origin can be a unique source (point-source) or dispersed sources.
Pollutants have differences in physical and chemical properties, explaining the discrepancy in their capacity for producing toxic effects. As an example, we state here that aerosol compounds ( 41 – 43 ) have a greater toxicity than gaseous compounds due to their tiny size (solid or liquid) in the atmosphere; they have a greater penetration capacity. Gaseous compounds are eliminated more easily by our respiratory system ( 41 ). These particles are able to damage lungs and can even enter the bloodstream ( 41 ), leading to the premature deaths of millions of people yearly. Moreover, the aerosol acidity ([H+]) seems to considerably enhance the production of secondary organic aerosols (SOA), but this last aspect is not supported by other scientific teams ( 38 ).
Climate and Pollution
Air pollution and climate change are closely related. Climate is the other side of the same coin that reduces the quality of our Earth ( 44 ). Pollutants such as black carbon, methane, tropospheric ozone, and aerosols affect the amount of incoming sunlight. As a result, the temperature of the Earth is increasing, resulting in the melting of ice, icebergs, and glaciers.
In this vein, climatic changes will affect the incidence and prevalence of both residual and imported infections in Europe. Climate and weather affect the duration, timing, and intensity of outbreaks strongly and change the map of infectious diseases in the globe ( 45 ). Mosquito-transmitted parasitic or viral diseases are extremely climate-sensitive, as warming firstly shortens the pathogen incubation period and secondly shifts the geographic map of the vector. Similarly, water-warming following climate changes leads to a high incidence of waterborne infections. Recently, in Europe, eradicated diseases seem to be emerging due to the migration of population, for example, cholera, poliomyelitis, tick-borne encephalitis, and malaria ( 46 ).
The spread of epidemics is associated with natural climate disasters and storms, which seem to occur more frequently nowadays ( 47 ). Malnutrition and disequilibration of the immune system are also associated with the emerging infections affecting public health ( 48 ).
The Chikungunya virus “took the airplane” from the Indian Ocean to Europe, as outbreaks of the disease were registered in Italy ( 49 ) as well as autochthonous cases in France ( 50 ).
An increase in cryptosporidiosis in the United Kingdom and in the Czech Republic seems to have occurred following flooding ( 36 , 51 ).
As stated previously, aerosols compounds are tiny in size and considerably affect the climate. They are able to dissipate sunlight (the albedo phenomenon) by dispersing a quarter of the sun's rays back to space and have cooled the global temperature over the last 30 years ( 52 ).
Air Pollutants
The World Health Organization (WHO) reports on six major air pollutants, namely particle pollution, ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. Air pollution can have a disastrous effect on all components of the environment, including groundwater, soil, and air. Additionally, it poses a serious threat to living organisms. In this vein, our interest is mainly to focus on these pollutants, as they are related to more extensive and severe problems in human health and environmental impact. Acid rain, global warming, the greenhouse effect, and climate changes have an important ecological impact on air pollution ( 53 ).
Particulate Matter (PM) and Health
Studies have shown a relationship between particulate matter (PM) and adverse health effects, focusing on either short-term (acute) or long-term (chronic) PM exposure.
Particulate matter (PM) is usually formed in the atmosphere as a result of chemical reactions between the different pollutants. The penetration of particles is closely dependent on their size ( 53 ). Particulate Matter (PM) was defined as a term for particles by the United States Environmental Protection Agency ( 54 ). Particulate matter (PM) pollution includes particles with diameters of 10 micrometers (μm) or smaller, called PM 10 , and extremely fine particles with diameters that are generally 2.5 micrometers (μm) and smaller.
Particulate matter contains tiny liquid or solid droplets that can be inhaled and cause serious health effects ( 55 ). Particles <10 μm in diameter (PM 10 ) after inhalation can invade the lungs and even reach the bloodstream. Fine particles, PM 2.5 , pose a greater risk to health ( 6 , 56 ) ( Table 1 ).
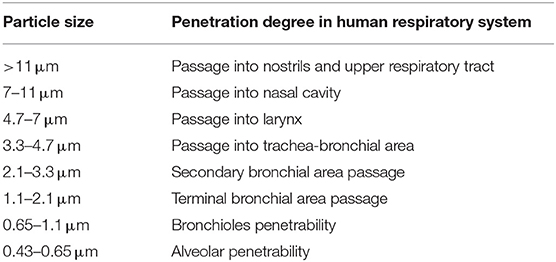
Table 1 . Penetrability according to particle size.
Multiple epidemiological studies have been performed on the health effects of PM. A positive relation was shown between both short-term and long-term exposures of PM 2.5 and acute nasopharyngitis ( 56 ). In addition, long-term exposure to PM for years was found to be related to cardiovascular diseases and infant mortality.
Those studies depend on PM 2.5 monitors and are restricted in terms of study area or city area due to a lack of spatially resolved daily PM 2.5 concentration data and, in this way, are not representative of the entire population. Following a recent epidemiological study by the Department of Environmental Health at Harvard School of Public Health (Boston, MA) ( 57 ), it was reported that, as PM 2.5 concentrations vary spatially, an exposure error (Berkson error) seems to be produced, and the relative magnitudes of the short- and long-term effects are not yet completely elucidated. The team developed a PM 2.5 exposure model based on remote sensing data for assessing short- and long-term human exposures ( 57 ). This model permits spatial resolution in short-term effects plus the assessment of long-term effects in the whole population.
Moreover, respiratory diseases and affection of the immune system are registered as long-term chronic effects ( 58 ). It is worth noting that people with asthma, pneumonia, diabetes, and respiratory and cardiovascular diseases are especially susceptible and vulnerable to the effects of PM. PM 2.5 , followed by PM 10 , are strongly associated with diverse respiratory system diseases ( 59 ), as their size permits them to pierce interior spaces ( 60 ). The particles produce toxic effects according to their chemical and physical properties. The components of PM 10 and PM 2.5 can be organic (polycyclic aromatic hydrocarbons, dioxins, benzene, 1-3 butadiene) or inorganic (carbon, chlorides, nitrates, sulfates, metals) in nature ( 55 ).
Particulate Matter (PM) is divided into four main categories according to type and size ( 61 ) ( Table 2 ).
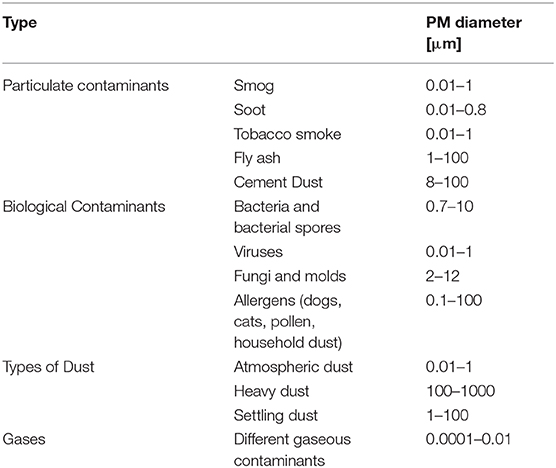
Table 2 . Types and sizes of particulate Matter (PM).
Gas contaminants include PM in aerial masses.
Particulate contaminants include contaminants such as smog, soot, tobacco smoke, oil smoke, fly ash, and cement dust.
Biological Contaminants are microorganisms (bacteria, viruses, fungi, mold, and bacterial spores), cat allergens, house dust and allergens, and pollen.
Types of Dust include suspended atmospheric dust, settling dust, and heavy dust.
Finally, another fact is that the half-lives of PM 10 and PM 2.5 particles in the atmosphere is extended due to their tiny dimensions; this permits their long-lasting suspension in the atmosphere and even their transfer and spread to distant destinations where people and the environment may be exposed to the same magnitude of pollution ( 53 ). They are able to change the nutrient balance in watery ecosystems, damage forests and crops, and acidify water bodies.
As stated, PM 2.5 , due to their tiny size, are causing more serious health effects. These aforementioned fine particles are the main cause of the “haze” formation in different metropolitan areas ( 12 , 13 , 61 ).
Ozone Impact in the Atmosphere
Ozone (O 3 ) is a gas formed from oxygen under high voltage electric discharge ( 62 ). It is a strong oxidant, 52% stronger than chlorine. It arises in the stratosphere, but it could also arise following chain reactions of photochemical smog in the troposphere ( 63 ).
Ozone can travel to distant areas from its initial source, moving with air masses ( 64 ). It is surprising that ozone levels over cities are low in contrast to the increased amounts occuring in urban areas, which could become harmful for cultures, forests, and vegetation ( 65 ) as it is reducing carbon assimilation ( 66 ). Ozone reduces growth and yield ( 47 , 48 ) and affects the plant microflora due to its antimicrobial capacity ( 67 , 68 ). In this regard, ozone acts upon other natural ecosystems, with microflora ( 69 , 70 ) and animal species changing their species composition ( 71 ). Ozone increases DNA damage in epidermal keratinocytes and leads to impaired cellular function ( 72 ).
Ground-level ozone (GLO) is generated through a chemical reaction between oxides of nitrogen and VOCs emitted from natural sources and/or following anthropogenic activities.
Ozone uptake usually occurs by inhalation. Ozone affects the upper layers of the skin and the tear ducts ( 73 ). A study of short-term exposure of mice to high levels of ozone showed malondialdehyde formation in the upper skin (epidermis) but also depletion in vitamins C and E. It is likely that ozone levels are not interfering with the skin barrier function and integrity to predispose to skin disease ( 74 ).
Due to the low water-solubility of ozone, inhaled ozone has the capacity to penetrate deeply into the lungs ( 75 ).
Toxic effects induced by ozone are registered in urban areas all over the world, causing biochemical, morphologic, functional, and immunological disorders ( 76 ).
The European project (APHEA2) focuses on the acute effects of ambient ozone concentrations on mortality ( 77 ). Daily ozone concentrations compared to the daily number of deaths were reported from different European cities for a 3-year period. During the warm period of the year, an observed increase in ozone concentration was associated with an increase in the daily number of deaths (0.33%), in the number of respiratory deaths (1.13%), and in the number of cardiovascular deaths (0.45%). No effect was observed during wintertime.
Carbon Monoxide (CO)
Carbon monoxide is produced by fossil fuel when combustion is incomplete. The symptoms of poisoning due to inhaling carbon monoxide include headache, dizziness, weakness, nausea, vomiting, and, finally, loss of consciousness.
The affinity of carbon monoxide to hemoglobin is much greater than that of oxygen. In this vein, serious poisoning may occur in people exposed to high levels of carbon monoxide for a long period of time. Due to the loss of oxygen as a result of the competitive binding of carbon monoxide, hypoxia, ischemia, and cardiovascular disease are observed.
Carbon monoxide affects the greenhouses gases that are tightly connected to global warming and climate. This should lead to an increase in soil and water temperatures, and extreme weather conditions or storms may occur ( 68 ).
However, in laboratory and field experiments, it has been seen to produce increased plant growth ( 78 ).
Nitrogen Oxide (NO 2 )
Nitrogen oxide is a traffic-related pollutant, as it is emitted from automobile motor engines ( 79 , 80 ). It is an irritant of the respiratory system as it penetrates deep in the lung, inducing respiratory diseases, coughing, wheezing, dyspnea, bronchospasm, and even pulmonary edema when inhaled at high levels. It seems that concentrations over 0.2 ppm produce these adverse effects in humans, while concentrations higher than 2.0 ppm affect T-lymphocytes, particularly the CD8+ cells and NK cells that produce our immune response ( 81 ).It is reported that long-term exposure to high levels of nitrogen dioxide can be responsible for chronic lung disease. Long-term exposure to NO 2 can impair the sense of smell ( 81 ).
However, systems other than respiratory ones can be involved, as symptoms such as eye, throat, and nose irritation have been registered ( 81 ).
High levels of nitrogen dioxide are deleterious to crops and vegetation, as they have been observed to reduce crop yield and plant growth efficiency. Moreover, NO 2 can reduce visibility and discolor fabrics ( 81 ).
Sulfur Dioxide (SO 2 )
Sulfur dioxide is a harmful gas that is emitted mainly from fossil fuel consumption or industrial activities. The annual standard for SO 2 is 0.03 ppm ( 82 ). It affects human, animal, and plant life. Susceptible people as those with lung disease, old people, and children, who present a higher risk of damage. The major health problems associated with sulfur dioxide emissions in industrialized areas are respiratory irritation, bronchitis, mucus production, and bronchospasm, as it is a sensory irritant and penetrates deep into the lung converted into bisulfite and interacting with sensory receptors, causing bronchoconstriction. Moreover, skin redness, damage to the eyes (lacrimation and corneal opacity) and mucous membranes, and worsening of pre-existing cardiovascular disease have been observed ( 81 ).
Environmental adverse effects, such as acidification of soil and acid rain, seem to be associated with sulfur dioxide emissions ( 83 ).
Lead is a heavy metal used in different industrial plants and emitted from some petrol motor engines, batteries, radiators, waste incinerators, and waste waters ( 84 ).
Moreover, major sources of lead pollution in the air are metals, ore, and piston-engine aircraft. Lead poisoning is a threat to public health due to its deleterious effects upon humans, animals, and the environment, especially in the developing countries.
Exposure to lead can occur through inhalation, ingestion, and dermal absorption. Trans- placental transport of lead was also reported, as lead passes through the placenta unencumbered ( 85 ). The younger the fetus is, the more harmful the toxic effects. Lead toxicity affects the fetal nervous system; edema or swelling of the brain is observed ( 86 ). Lead, when inhaled, accumulates in the blood, soft tissue, liver, lung, bones, and cardiovascular, nervous, and reproductive systems. Moreover, loss of concentration and memory, as well as muscle and joint pain, were observed in adults ( 85 , 86 ).
Children and newborns ( 87 ) are extremely susceptible even to minimal doses of lead, as it is a neurotoxicant and causes learning disabilities, impairment of memory, hyperactivity, and even mental retardation.
Elevated amounts of lead in the environment are harmful to plants and crop growth. Neurological effects are observed in vertebrates and animals in association with high lead levels ( 88 ).
Polycyclic Aromatic Hydrocarbons(PAHs)
The distribution of PAHs is ubiquitous in the environment, as the atmosphere is the most important means of their dispersal. They are found in coal and in tar sediments. Moreover, they are generated through incomplete combustion of organic matter as in the cases of forest fires, incineration, and engines ( 89 ). PAH compounds, such as benzopyrene, acenaphthylene, anthracene, and fluoranthene are recognized as toxic, mutagenic, and carcinogenic substances. They are an important risk factor for lung cancer ( 89 ).
Volatile Organic Compounds(VOCs)
Volatile organic compounds (VOCs), such as toluene, benzene, ethylbenzene, and xylene ( 90 ), have been found to be associated with cancer in humans ( 91 ). The use of new products and materials has actually resulted in increased concentrations of VOCs. VOCs pollute indoor air ( 90 ) and may have adverse effects on human health ( 91 ). Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ). Predictable assessment of the toxic effects of complex VOC mixtures is difficult to estimate, as these pollutants can have synergic, antagonistic, or indifferent effects ( 91 , 93 ).
Dioxins originate from industrial processes but also come from natural processes, such as forest fires and volcanic eruptions. They accumulate in foods such as meat and dairy products, fish and shellfish, and especially in the fatty tissue of animals ( 94 ).
Short-period exhibition to high dioxin concentrations may result in dark spots and lesions on the skin ( 94 ). Long-term exposure to dioxins can cause developmental problems, impairment of the immune, endocrine and nervous systems, reproductive infertility, and cancer ( 94 ).
Without any doubt, fossil fuel consumption is responsible for a sizeable part of air contamination. This contamination may be anthropogenic, as in agricultural and industrial processes or transportation, while contamination from natural sources is also possible. Interestingly, it is of note that the air quality standards established through the European Air Quality Directive are somewhat looser than the WHO guidelines, which are stricter ( 95 ).
Effect of Air Pollution on Health
The most common air pollutants are ground-level ozone and Particulates Matter (PM). Air pollution is distinguished into two main types:
Outdoor pollution is the ambient air pollution.
Indoor pollution is the pollution generated by household combustion of fuels.
People exposed to high concentrations of air pollutants experience disease symptoms and states of greater and lesser seriousness. These effects are grouped into short- and long-term effects affecting health.
Susceptible populations that need to be aware of health protection measures include old people, children, and people with diabetes and predisposing heart or lung disease, especially asthma.
As extensively stated previously, according to a recent epidemiological study from Harvard School of Public Health, the relative magnitudes of the short- and long-term effects have not been completely clarified ( 57 ) due to the different epidemiological methodologies and to the exposure errors. New models are proposed for assessing short- and long-term human exposure data more successfully ( 57 ). Thus, in the present section, we report the more common short- and long-term health effects but also general concerns for both types of effects, as these effects are often dependent on environmental conditions, dose, and individual susceptibility.
Short-term effects are temporary and range from simple discomfort, such as irritation of the eyes, nose, skin, throat, wheezing, coughing and chest tightness, and breathing difficulties, to more serious states, such as asthma, pneumonia, bronchitis, and lung and heart problems. Short-term exposure to air pollution can also cause headaches, nausea, and dizziness.
These problems can be aggravated by extended long-term exposure to the pollutants, which is harmful to the neurological, reproductive, and respiratory systems and causes cancer and even, rarely, deaths.
The long-term effects are chronic, lasting for years or the whole life and can even lead to death. Furthermore, the toxicity of several air pollutants may also induce a variety of cancers in the long term ( 96 ).
As stated already, respiratory disorders are closely associated with the inhalation of air pollutants. These pollutants will invade through the airways and will accumulate at the cells. Damage to target cells should be related to the pollutant component involved and its source and dose. Health effects are also closely dependent on country, area, season, and time. An extended exposure duration to the pollutant should incline to long-term health effects in relation also to the above factors.
Particulate Matter (PMs), dust, benzene, and O 3 cause serious damage to the respiratory system ( 97 ). Moreover, there is a supplementary risk in case of existing respiratory disease such as asthma ( 98 ). Long-term effects are more frequent in people with a predisposing disease state. When the trachea is contaminated by pollutants, voice alterations may be remarked after acute exposure. Chronic obstructive pulmonary disease (COPD) may be induced following air pollution, increasing morbidity and mortality ( 99 ). Long-term effects from traffic, industrial air pollution, and combustion of fuels are the major factors for COPD risk ( 99 ).
Multiple cardiovascular effects have been observed after exposure to air pollutants ( 100 ). Changes occurred in blood cells after long-term exposure may affect cardiac functionality. Coronary arteriosclerosis was reported following long-term exposure to traffic emissions ( 101 ), while short-term exposure is related to hypertension, stroke, myocardial infracts, and heart insufficiency. Ventricle hypertrophy is reported to occur in humans after long-time exposure to nitrogen oxide (NO 2 ) ( 102 , 103 ).
Neurological effects have been observed in adults and children after extended-term exposure to air pollutants.
Psychological complications, autism, retinopathy, fetal growth, and low birth weight seem to be related to long-term air pollution ( 83 ). The etiologic agent of the neurodegenerative diseases (Alzheimer's and Parkinson's) is not yet known, although it is believed that extended exposure to air pollution seems to be a factor. Specifically, pesticides and metals are cited as etiological factors, together with diet. The mechanisms in the development of neurodegenerative disease include oxidative stress, protein aggregation, inflammation, and mitochondrial impairment in neurons ( 104 ) ( Figure 1 ).
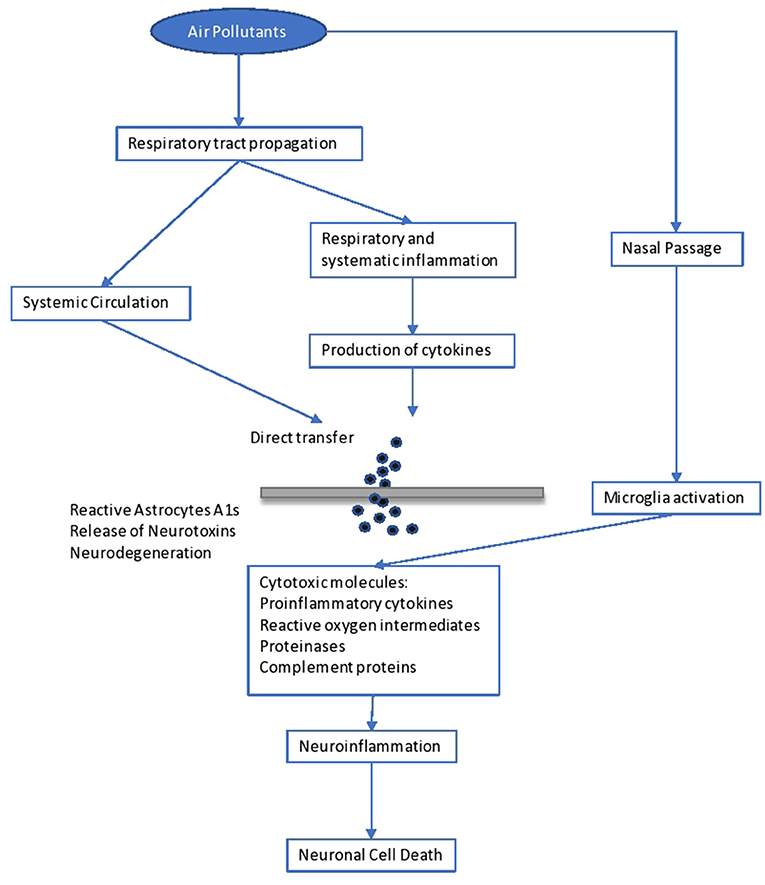
Figure 1 . Impact of air pollutants on the brain.
Brain inflammation was observed in dogs living in a highly polluted area in Mexico for a long period ( 105 ). In human adults, markers of systemic inflammation (IL-6 and fibrinogen) were found to be increased as an immediate response to PNC on the IL-6 level, possibly leading to the production of acute-phase proteins ( 106 ). The progression of atherosclerosis and oxidative stress seem to be the mechanisms involved in the neurological disturbances caused by long-term air pollution. Inflammation comes secondary to the oxidative stress and seems to be involved in the impairment of developmental maturation, affecting multiple organs ( 105 , 107 ). Similarly, other factors seem to be involved in the developmental maturation, which define the vulnerability to long-term air pollution. These include birthweight, maternal smoking, genetic background and socioeconomic environment, as well as education level.
However, diet, starting from breast-feeding, is another determinant factor. Diet is the main source of antioxidants, which play a key role in our protection against air pollutants ( 108 ). Antioxidants are free radical scavengers and limit the interaction of free radicals in the brain ( 108 ). Similarly, genetic background may result in a differential susceptibility toward the oxidative stress pathway ( 60 ). For example, antioxidant supplementation with vitamins C and E appears to modulate the effect of ozone in asthmatic children homozygous for the GSTM1 null allele ( 61 ). Inflammatory cytokines released in the periphery (e.g., respiratory epithelia) upregulate the innate immune Toll-like receptor 2. Such activation and the subsequent events leading to neurodegeneration have recently been observed in lung lavage in mice exposed to ambient Los Angeles (CA, USA) particulate matter ( 61 ). In children, neurodevelopmental morbidities were observed after lead exposure. These children developed aggressive and delinquent behavior, reduced intelligence, learning difficulties, and hyperactivity ( 109 ). No level of lead exposure seems to be “safe,” and the scientific community has asked the Centers for Disease Control and Prevention (CDC) to reduce the current screening guideline of 10 μg/dl ( 109 ).
It is important to state that impact on the immune system, causing dysfunction and neuroinflammation ( 104 ), is related to poor air quality. Yet, increases in serum levels of immunoglobulins (IgA, IgM) and the complement component C3 are observed ( 106 ). Another issue is that antigen presentation is affected by air pollutants, as there is an upregulation of costimulatory molecules such as CD80 and CD86 on macrophages ( 110 ).
As is known, skin is our shield against ultraviolet radiation (UVR) and other pollutants, as it is the most exterior layer of our body. Traffic-related pollutants, such as PAHs, VOCs, oxides, and PM, may cause pigmented spots on our skin ( 111 ). On the one hand, as already stated, when pollutants penetrate through the skin or are inhaled, damage to the organs is observed, as some of these pollutants are mutagenic and carcinogenic, and, specifically, they affect the liver and lung. On the other hand, air pollutants (and those in the troposphere) reduce the adverse effects of ultraviolet radiation UVR in polluted urban areas ( 111 ). Air pollutants absorbed by the human skin may contribute to skin aging, psoriasis, acne, urticaria, eczema, and atopic dermatitis ( 111 ), usually caused by exposure to oxides and photochemical smoke ( 111 ). Exposure to PM and cigarette smoking act as skin-aging agents, causing spots, dyschromia, and wrinkles. Lastly, pollutants have been associated with skin cancer ( 111 ).
Higher morbidity is reported to fetuses and children when exposed to the above dangers. Impairment in fetal growth, low birth weight, and autism have been reported ( 112 ).
Another exterior organ that may be affected is the eye. Contamination usually comes from suspended pollutants and may result in asymptomatic eye outcomes, irritation ( 112 ), retinopathy, or dry eye syndrome ( 113 , 114 ).
Environmental Impact of Air Pollution
Air pollution is harming not only human health but also the environment ( 115 ) in which we live. The most important environmental effects are as follows.
Acid rain is wet (rain, fog, snow) or dry (particulates and gas) precipitation containing toxic amounts of nitric and sulfuric acids. They are able to acidify the water and soil environments, damage trees and plantations, and even damage buildings and outdoor sculptures, constructions, and statues.
Haze is produced when fine particles are dispersed in the air and reduce the transparency of the atmosphere. It is caused by gas emissions in the air coming from industrial facilities, power plants, automobiles, and trucks.
Ozone , as discussed previously, occurs both at ground level and in the upper level (stratosphere) of the Earth's atmosphere. Stratospheric ozone is protecting us from the Sun's harmful ultraviolet (UV) rays. In contrast, ground-level ozone is harmful to human health and is a pollutant. Unfortunately, stratospheric ozone is gradually damaged by ozone-depleting substances (i.e., chemicals, pesticides, and aerosols). If this protecting stratospheric ozone layer is thinned, then UV radiation can reach our Earth, with harmful effects for human life (skin cancer) ( 116 ) and crops ( 117 ). In plants, ozone penetrates through the stomata, inducing them to close, which blocks CO 2 transfer and induces a reduction in photosynthesis ( 118 ).
Global climate change is an important issue that concerns mankind. As is known, the “greenhouse effect” keeps the Earth's temperature stable. Unhappily, anthropogenic activities have destroyed this protecting temperature effect by producing large amounts of greenhouse gases, and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. A report states that global warming is adding to the health risks of poor people ( 119 ).
People living in poorly constructed buildings in warm-climate countries are at high risk for heat-related health problems as temperatures mount ( 119 ).
Wildlife is burdened by toxic pollutants coming from the air, soil, or the water ecosystem and, in this way, animals can develop health problems when exposed to high levels of pollutants. Reproductive failure and birth effects have been reported.
Eutrophication is occurring when elevated concentrations of nutrients (especially nitrogen) stimulate the blooming of aquatic algae, which can cause a disequilibration in the diversity of fish and their deaths.
Without a doubt, there is a critical concentration of pollution that an ecosystem can tolerate without being destroyed, which is associated with the ecosystem's capacity to neutralize acidity. The Canada Acid Rain Program established this load at 20 kg/ha/yr ( 120 ).
Hence, air pollution has deleterious effects on both soil and water ( 121 ). Concerning PM as an air pollutant, its impact on crop yield and food productivity has been reported. Its impact on watery bodies is associated with the survival of living organisms and fishes and their productivity potential ( 121 ).
An impairment in photosynthetic rhythm and metabolism is observed in plants exposed to the effects of ozone ( 121 ).
Sulfur and nitrogen oxides are involved in the formation of acid rain and are harmful to plants and marine organisms.
Last but not least, as mentioned above, the toxicity associated with lead and other metals is the main threat to our ecosystems (air, water, and soil) and living creatures ( 121 ).
In 2018, during the first WHO Global Conference on Air Pollution and Health, the WHO's General Director, Dr. Tedros Adhanom Ghebreyesus, called air pollution a “silent public health emergency” and “the new tobacco” ( 122 ).
Undoubtedly, children are particularly vulnerable to air pollution, especially during their development. Air pollution has adverse effects on our lives in many different respects.
Diseases associated with air pollution have not only an important economic impact but also a societal impact due to absences from productive work and school.
Despite the difficulty of eradicating the problem of anthropogenic environmental pollution, a successful solution could be envisaged as a tight collaboration of authorities, bodies, and doctors to regularize the situation. Governments should spread sufficient information and educate people and should involve professionals in these issues so as to control the emergence of the problem successfully.
Technologies to reduce air pollution at the source must be established and should be used in all industries and power plants. The Kyoto Protocol of 1997 set as a major target the reduction of GHG emissions to below 5% by 2012 ( 123 ). This was followed by the Copenhagen summit, 2009 ( 124 ), and then the Durban summit of 2011 ( 125 ), where it was decided to keep to the same line of action. The Kyoto protocol and the subsequent ones were ratified by many countries. Among the pioneers who adopted this important protocol for the world's environmental and climate “health” was China ( 3 ). As is known, China is a fast-developing economy and its GDP (Gross Domestic Product) is expected to be very high by 2050, which is defined as the year of dissolution of the protocol for the decrease in gas emissions.
A more recent international agreement of crucial importance for climate change is the Paris Agreement of 2015, issued by the UNFCCC (United Nations Climate Change Committee). This latest agreement was ratified by a plethora of UN (United Nations) countries as well as the countries of the European Union ( 126 ). In this vein, parties should promote actions and measures to enhance numerous aspects around the subject. Boosting education, training, public awareness, and public participation are some of the relevant actions for maximizing the opportunities to achieve the targets and goals on the crucial matter of climate change and environmental pollution ( 126 ). Without any doubt, technological improvements makes our world easier and it seems difficult to reduce the harmful impact caused by gas emissions, we could limit its use by seeking reliable approaches.
Synopsizing, a global prevention policy should be designed in order to combat anthropogenic air pollution as a complement to the correct handling of the adverse health effects associated with air pollution. Sustainable development practices should be applied, together with information coming from research in order to handle the problem effectively.
At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. Legislation concerning air pollution must be aligned and updated, and policy makers should propose the design of a powerful tool of environmental and health protection. As a result, the main proposal of this essay is that we should focus on fostering local structures to promote experience and practice and extrapolate these to the international level through developing effective policies for sustainable management of ecosystems.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
IM is employed by the company Delphis S.A.
The remaining authors declare that the present review paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. WHO. Air Pollution . WHO. Available online at: http://www.who.int/airpollution/en/ (accessed October 5, 2019).
Google Scholar
2. Moores FC. Climate change and air pollution: exploring the synergies and potential for mitigation in industrializing countries. Sustainability . (2009) 1:43–54. doi: 10.3390/su1010043
CrossRef Full Text | Google Scholar
3. USGCRP (2009). Global Climate Change Impacts in the United States. In: Karl TR, Melillo JM, Peterson TC, editors. Climate Change Impacts by Sectors: Ecosystems . New York, NY: United States Global Change Research Program. Cambridge University Press.
4. Marlon JR, Bloodhart B, Ballew MT, Rolfe-Redding J, Roser-Renouf C, Leiserowitz A, et al. (2019). How hope and doubt affect climate change mobilization. Front. Commun. 4:20. doi: 10.3389/fcomm.2019.00020
5. Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long- term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int . (2014) 70:95–105. doi: 10.1016/j.envint.2014.05.014
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Kelishadi R, Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci . (2010) 6:483–95. doi: 10.5114/aoms.2010.14458
7. Manucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health . (2017) 14:1048. doi: 10.3390/ijerph14091048
8. Burden of Disease from Ambient and Household Air Pollution . Available online: http://who.int/phe/health_topics/outdoorair/databases/en/ (accessed August 15, 2017).
9. Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health . (2014) 80:393–411. doi: 10.1016/j.aogh.2014.10.002
10. Guo Y, Zeng H, Zheng R, Li S, Pereira G, Liu Q, et al. The burden of lung cancer mortality attributable to fine particles in China. Total Environ Sci . (2017) 579:1460–6. doi: 10.1016/j.scitotenv.2016.11.147
11. Hou Q, An XQ, Wang Y, Guo JP. An evaluation of resident exposure to respirable particulate matter and health economic loss in Beijing during Beijing 2008 Olympic Games. Sci Total Environ . (2010) 408:4026–32. doi: 10.1016/j.scitotenv.2009.12.030
12. Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int . (2012) 42:10–9. doi: 10.1016/j.envint.2011.03.003
13. Burroughs Peña MS, Rollins A. Environmental exposures and cardiovascular disease: a challenge for health and development in low- and middle-income countries. Cardiol Clin . (2017) 35:71–86. doi: 10.1016/j.ccl.2016.09.001
14. Kankaria A, Nongkynrih B, Gupta S. Indoor air pollution in india: implications on health and its control. Indian J Comm Med . 39:203–7. doi: 10.4103/0970-0218.143019
15. Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sust Built Env . (2016) 5:301–11. doi: 10.1016/j.ijsbe.2016.08.003
16. Saud T, Gautam R, Mandal TK, Gadi R, Singh DP, Sharma SK. Emission estimates of organic and elemental carbon from household biomass fuel used over the Indo-Gangetic Plain (IGP), India. Atmos Environ . (2012) 61:212–20. doi: 10.1016/j.atmosenv.2012.07.030
17. Singh DP, Gadi R, Mandal TK, Saud T, Saxena M, Sharma SK. Emissions estimates of PAH from biomass fuels used in rural sector of Indo-Gangetic Plains of India. Atmos Environ . (2013) 68:120–6. doi: 10.1016/j.atmosenv.2012.11.042
18. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M BN. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ . (2008) 86:390–4. doi: 10.2471/BLT.07.044529
19. Kassomenos P, Kelessis A, Petrakakis M, Zoumakis N, Christides T, Paschalidou AK. Air Quality assessment in a heavily-polluted urban Mediterranean environment through Air Quality indices. Ecol Indic . (2012) 18:259–68. doi: 10.1016/j.ecolind.2011.11.021
20. Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med . (1993) 329:1753–9. doi: 10.1056/NEJM199312093292401
21. Schwela DH, Köth-Jahr I. Leitfaden für die Aufstellung von Luftreinhalteplänen [Guidelines for the Implementation of Clean Air Implementation Plans]. Landesumweltamt des Landes Nordrhein Westfalen. State Environmental Service of the State of North Rhine-Westphalia (1994).
22. Newlands M. Environmental Activism, Environmental Politics, and Representation: The Framing of the British Environmental Activist Movement . Ph.D. thesis. University of East London, United Kingdom (2015).
23. NEPIS (National Service Center for Environmental Publications) US EPA (Environmental Protection Agency) (2017). Available online at: https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges (accessed August 15, 2017).
24. NRC (National Research Council). Available online at: https://www.nap.edu/read/10728/chapter/1,2014 (accessed September 17, 2019).
25. Bull A. Traffic Congestion: The Problem and How to Deal With It . Santiago: Nationes Unidas, Cepal (2003).
26. Spiegel J, Maystre LY. Environmental Pollution Control, Part VII - The Environment, Chapter 55, Encyclopedia of Occupational Health and Safety . Available online at: http://www.ilocis.org/documents/chpt55e.htm (accessed September 17, 2019).
27. European Community Reports. Assessment of the Effectiveness of European Air Quality Policies and Measures: Case Study 2; Comparison of the EU and US Air Quality Standards and Planning Requirements. (2004). Available online at: https://ec.europa.eu/environment/archives/cafe/activities/pdf/case_study2.pdf (accessed September 22, 2019).
28. Gibson R, Ward S. Parties in the digital age; a review. J Represent Democracy . (2009) 45:87–100. doi: 10.1080/00344890802710888
29. Kaun A, Uldam J. Digital activism: after the hype. New Media Soc. (2017) 20:2099–106. doi: 10.1177/14614448177319
30. Sivitanides M, Shah V. The era of digital activism. In: 2011 Conference for Information Systems Applied Research(CONISAR) Proceedings Wilmington North Carolina, USA . Available online at: https://www.arifyildirim.com/ilt510/marcos.sivitanides.vivek.shah.pdf (accessed September 22, 2019).
31. Möller L, Schuetzle D, Autrup H. Future research needs associated with the assessment of potential human health risks from exposure to toxic ambient air pollutants. Environ Health Perspect . (1994) 102(Suppl. 4):193–210. doi: 10.1289/ehp.94102s4193
32. Jacobson MZ, Jacobson PMZ. Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press (2002). p. 206. doi: 10.1256/wea.243.02
33. Stover RH. Flooding of soil for disease control. In: Mulder D, editor. Chapter 3. Developments in Agricultural and Managed Forest Ecology . Elsevier (1979). p. 19–28. Available online at: http://www.sciencedirect.com/science/article/pii/B9780444416926500094 doi: 10.1016/B978-0-444-41692-6.50009-4 (accessed July 1, 2019).
34. Maipa V, Alamanos Y, Bezirtzoglou E. Seasonal fluctuation of bacterial indicators in coastal waters. Microb Ecol Health Dis . (2001) 13:143–6. doi: 10.1080/089106001750462687
35. Bezirtzoglou E, Dimitriou D, Panagiou A. Occurrence of Clostridium perfringens in river water by using a new procedure. Anaerobe . (1996) 2:169–73. doi: 10.1006/anae.1996.0022
36. Kjellstrom T, Lodh M, McMichael T, Ranmuthugala G, Shrestha R, Kingsland S. Air and Water Pollution: Burden and Strategies for Control. DCP, Chapter 43. 817–32 p. Available online at: https://www.dcp-3.org/sites/default/files/dcp2/DCP43.pdf (accessed September 17, 2017).
37. Pathak RK, Wang T, Ho KF, Lee SC. Characteristics of summertime PM2.5 organic and elemental carbon in four major Chinese cities: implications of high acidity for water- soluble organic carbon (WSOC). Atmos Environ . (2011) 45:318–25. doi: 10.1016/j.atmosenv.2010.10.021
38. Bonavigo L, Zucchetti M, Mankolli H. Water radioactive pollution and related environmental aspects. J Int Env Appl Sci . (2009) 4:357–63
39. World Health Organization (WHO). Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease . 1106 p. Available online at: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed September 22, 2019).
40. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health . (2015) 12:12735–60. doi: 10.3390/ijerph121012735
41. Ethical Unicorn. Everything You Need To Know About Aerosols & Air Pollution. (2019). Available online at: https://ethicalunicorn.com/2019/04/29/everything-you-need-to-know-about-aerosols-air-pollution/ (accessed October 4, 2019).
42. Colbeck I, Lazaridis M. Aerosols and environmental pollution. Sci Nat . (2009) 97:117–31. doi: 10.1007/s00114-009-0594-x
43. Incecik S, Gertler A, Kassomenos P. Aerosols and air quality. Sci Total Env . (2014) 355, 488–9. doi: 10.1016/j.scitotenv.2014.04.012
44. D'Amato G, Pawankar R, Vitale C, Maurizia L. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res . (2016) 8:391–5. doi: 10.4168/aair.2016.8.5.391
45. Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe . (2011) 17:337–40. doi: 10.1016/j.anaerobe.2011.05.016
46. Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect . (2017) 23:283–9. doi: 10.1016/j.cmi.2017.03.012
47. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis . (2007) 13:1–5. doi: 10.3201/eid1301.060779
48. Fenn B. Malnutrition in Humanitarian Emergencies . Available online at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_malnutrition_fenn.pdf . (accessed August 15, 2017).
49. Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak Chikungunya virus belongs to an emerging Aedes albopictus –adapted virus cluster introduced from the Indian subcontinent. Open Forum Infect Dis. (2019) 6:ofy321. doi: 10.1093/ofid/ofy321
50. Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, Pigaglio L, Decoppet A, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Eur Surveill . (2017) 22:17-00647. doi: 10.2807/1560-7917.ES.2017.22.39.17-00647
51. Menne B, Murray V. Floods in the WHO European Region: Health Effects and Their Prevention . Copenhagen: WHO; Weltgesundheits organisation, Regionalbüro für Europa (2013). Available online at: http://www.euro.who.int/data/assets/pdf_file/0020/189020/e96853.pdf (accessed 15 August 2017).
52. Schneider SH. The greenhouse effect: science and policy. Science . (1989) 243:771–81. doi: 10.1126/science.243.4892.771
53. Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc . (1997) 47:1238–49. doi: 10.1080/10473289.1997.10464074
54. US EPA (US Environmental Protection Agency) (2018). Available online at: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed September 22, 2018).
55. Cheung K, Daher N, Kam W, Shafer MM, Ning Z, Schauer JJ, et al. Spatial and temporal variation of chemical composition and mass closure of ambient coarse particulate matter (PM10–2.5) in the Los Angeles area. Atmos Environ . (2011) 45:2651–62. doi: 10.1016/j.atmosenv.2011.02.066
56. Zhang L, Yang Y, Li Y, Qian ZM, Xiao W, Wang X, et al. Short-term and long-term effects of PM2.5 on acute nasopharyngitis in 10 communities of Guangdong, China. Sci Total Env. (2019) 688:136–42. doi: 10.1016/j.scitotenv.2019.05.470.
57. Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and short-term exposure to PM2.5 and mortality using novel exposure models, Epidemiology . (2013) 24:555–61. doi: 10.1097/EDE.0b013e318294beaa
58. New Hampshire Department of Environmental Services. Current and Forecasted Air Quality in New Hampshire . Environmental Fact Sheet (2019). Available online at: https://www.des.nh.gov/organization/commissioner/pip/factsheets/ard/documents/ard-16.pdf (accessed September 22, 2019).
59. Kappos AD, Bruckmann P, Eikmann T, Englert N, Heinrich U, Höppe P, et al. Health effects of particles in ambient air. Int J Hyg Environ Health . (2004) 207:399–407. doi: 10.1078/1438-4639-00306
60. Boschi N (Ed.). Defining an educational framework for indoor air sciences education. In: Education and Training in Indoor Air Sciences . Luxembourg: Springer Science & Business Media (2012). 245 p.
61. Heal MR, Kumar P, Harrison RM. Particles, air quality, policy and health. Chem Soc Rev . (2012) 41:6606–30. doi: 10.1039/c2cs35076a
62. Bezirtzoglou E, Alexopoulos A. Ozone history and ecosystems: a goliath from impacts to advance industrial benefits and interests, to environmental and therapeutical strategies. In: Ozone Depletion, Chemistry and Impacts. (2009). p. 135–45.
63. Villányi V, Turk B, Franc B, Csintalan Z. Ozone Pollution and its Bioindication. In: Villányi V, editor. Air Pollution . London: Intech Open (2010). doi: 10.5772/10047
64. Massachusetts Department of Public Health. Massachusetts State Health Assessment . Boston, MA (2017). Available online at: https://www.mass.gov/files/documents/2017/11/03/2017%20MA%20SHA%20final%20compressed.pdf (accessed October 30, 2017).
65. Lorenzini G, Saitanis C. Ozone: A Novel Plant “Pathogen.” In: Sanitá di Toppi L, Pawlik-Skowrońska B, editors. Abiotic Stresses in Plant Springer Link (2003). p. 205–29. doi: 10.1007/978-94-017-0255-3_8
66. Fares S, Vargas R, Detto M, Goldstein AH, Karlik J, Paoletti E, et al. Tropospheric ozone reduces carbon assimilation in trees: estimates from analysis of continuous flux measurements. Glob Change Biol . (2013) 19:2427–43. doi: 10.1111/gcb.12222
67. Harmens H, Mills G, Hayes F, Jones L, Norris D, Fuhrer J. Air Pollution and Vegetation . ICP Vegetation Annual Report 2006/2007. (2012)
68. Emberson LD, Pleijel H, Ainsworth EA, den Berg M, Ren W, Osborne S, et al. Ozone effects on crops and consideration in crop models. Eur J Agron . (2018) 100:19–34. doi: 10.1016/j.eja.2018.06.002
69. Alexopoulos A, Plessas S, Ceciu S, Lazar V, Mantzourani I, Voidarou C, et al. Evaluation of ozone efficacy on the reduction of microbial population of fresh cut lettuce ( Lactuca sativa ) and green bell pepper ( Capsicum annuum ). Food Control . (2013) 30:491–6. doi: 10.1016/j.foodcont.2012.09.018
70. Alexopoulos A, Plessas S, Kourkoutas Y, Stefanis C, Vavias S, Voidarou C, et al. Experimental effect of ozone upon the microbial flora of commercially produced dairy fermented products. Int J Food Microbiol . (2017) 246:5–11. doi: 10.1016/j.ijfoodmicro.2017.01.018
71. Maggio A, Fagnano M. Ozone damages to mediterranean crops: physiological responses. Ital J Agron . (2008) 13–20. doi: 10.4081/ija.2008.13
72. McCarthy JT, Pelle E, Dong K, Brahmbhatt K, Yarosh D, Pernodet N. Effects of ozone in normal human epidermal keratinocytes. Exp Dermatol . (2013) 22:360–1. doi: 10.1111/exd.12125
73. WHO. Health Risks of Ozone From Long-Range Transboundary Air Pollution . Available online at: http://www.euro.who.int/data/assets/pdf_file/0005/78647/E91843.pdf (accessed August 15, 2019).
74. Thiele JJ, Traber MG, Tsang K, Cross CE, Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic Biol Med. (1997) 23:365–91. doi: 10.1016/S0891-5849(96)00617-X
75. Hatch GE, Slade R, Harris LP, McDonnell WF, Devlin RB, Koren HS, et al. Ozone dose and effect in humans and rats. A comparison using oxygen- 18 labeling and bronchoalveolar lavage. Am J Respir Crit Care Med . (1994) 150:676–83. doi: 10.1164/ajrccm.150.3.8087337
76. Lippmann M. Health effects of ozone. A critical review. JAPCA . (1989) 39:672–95. doi: 10.1080/08940630.1989.10466554
77. Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am J Respir Crit Care Med . (2004) 170:1080–7. doi: 10.1164/rccm.200403-333OC
78. Soon W, Baliunas SL, Robinson AB, Robinson ZW. Environmental effects of increased atmospheric carbon dioxide. Climate Res . (1999) 13:149–64 doi: 10.1260/0958305991499694
79. Richmont-Bryant J, Owen RC, Graham S, Snyder M, McDow S, Oakes M, et al. Estimation of on-road NO2 concentrations, NO2/NOX ratios, and related roadway gradients from near-road monitoring data. Air Qual Atm Health . (2017) 10:611–25. doi: 10.1007/s11869-016-0455-7
80. Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA. Critical review of the human data on short-term nitrogen dioxide (NO 2 ) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol . (2009) 39:743–81. doi: 10.3109/10408440903294945
81. Chen T-M, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci . (2007) 333:249–56. doi: 10.1097/MAJ.0b013e31803b900f
82. US EPA. Table of Historical SO 2 NAAQS, Sulfur US EPA . Available online at: https://www3.epa.gov/ttn/naaqs/standards/so2/s_so2_history.html (accessed October 5, 2019).
83. WHO Regional Office of Europe (2000). Available online at: https://euro.who.int/_data/assets/pdf_file/0020/123086/AQG2ndEd_7_4Sulfuroxide.pdf
84. Pruss-Ustun A, Fewrell L, Landrigan PJ, Ayuso-Mateos JL. Lead exposure. Comparative Quantification of Health Risks . World Health Organization. p. 1495–1542. Available online at: https://www.who.int/publications/cra/chapters/volume2/1495-1542.pdf?ua=1
PubMed Abstract | Google Scholar
85. Goyer RA. Transplacental transport of lead. Environ Health Perspect . (1990) 89:101–5. doi: 10.1289/ehp.9089101
86. National Institute of Environmental Health Sciences (NIH). Lead and Your Health . (2013). 1–4 p. Available online at: https://www.niehs.nih.gov/health/materials/lead_and_your_health_508.pdf (accessed September 17, 2019).
87. Farhat A, Mohammadzadeh A, Balali-Mood M, Aghajanpoor-Pasha M, Ravanshad Y. Correlation of blood lead level in mothers and exclusively breastfed infants: a study on infants aged less than six months. Asia Pac J Med Toxicol . (2013) 2:150–2.
88. Assi MA, Hezmee MNM, Haron AW, Sabri MYM, Rajion MA. The detrimental effects of lead on human and animal health. Vet World . (2016) 9:660–71. doi: 10.14202/vetworld.2016.660-671
89. Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet . (2016) 25:107–23. doi: 10.1016/j.ejpe.2015.03.011
90. Kumar A, Singh BP, Punia M, Singh D, Kumar K, Jain VK. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ Sci Pollut Res Int . (2014) 21:2240–8. doi: 10.1007/s11356-013-2150-7
91. Molhave L, Clausen G, Berglund B, Ceaurriz J, Kettrup A, Lindvall T, et al. Total Volatile Organic Compounds (TVOC) in Indoor Air Quality Investigations. Indoor Air . 7:225–240. doi: 10.1111/j.1600-0668.1997.00002.x
92. Gibb T. Indoor Air Quality May be Hazardous to Your Health . MSU Extension. Available online at: https://www.canr.msu.edu/news/indoor_air_quality_may_be_hazardous_to_your_health (accessed October 5, 2019).
93. Ebersviller S, Lichtveld K, Sexton KG, Zavala J, Lin Y-H, Jaspers I, et al. Gaseous VOCs rapidly modify particulate matter and its biological effects – Part 1: simple VOCs and model PM. Atmos Chem Phys Discuss . (2012) 12:5065–105. doi: 10.5194/acpd-12-5065-2012
94. WHO (World Health Organization). Dioxins and Their Effects on Human Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/dioxins-and-their-effects-on-human-health (accessed October 5, 2019).
95. EEA (European Environmental Agency). Air Quality Standards to the European Union and WHO . Available online at: https://www.eea.europa.eu/themes/data-and-maps/figures/air-quality-standards-under-the
96. Nakano T, Otsuki T. [Environmental air pollutants and the risk of cancer]. (Japanese). Gan To Kagaku Ryoho . (2013) 40:1441–5.
97. Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med . (2016) 22:138–43. doi: 10.1097/MCP.0000000000000248
98. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet . (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
99. Jiang X-Q, Mei X-D, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis . (2016) 8:E31–40.
100. Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis . (2017) 110:634–42. doi: 10.1016/j.acvd.2017.05.003
101. Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation . (2007) 116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622
102. Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens . (2011) 2011:495349. doi: 10.4061/2011/495349
103. Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic- related air pollution and the right ventricle. the multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med . (2014) 189:1093–100. doi: 10.1164/rccm.201312-2298OC
104. Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol . (2012) 2012:782462. doi: 10.1155/2012/782462
105. Calderon-Garciduenas L, Azzarelli B, Acuna H, et al. Air pollution and brain damage. Toxicol Pathol. (2002) 30:373–89. doi: 10.1080/01926230252929954
106. Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect . (2007) 115:1072–80. doi: 10.1289/ehp.10021
107. Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol . (2006) 3:13–8. doi: 10.1186/1743-8977-3-13
108. Kelly FJ. Dietary antioxidants and environmental stress. Proc Nutr Soc . (2004) 63:579–85. doi: 10.1079/PNS2004388
109. Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr . (2008) 20:172–7. doi: 10.1097/MOP.0b013e3282f4f97b
110. Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol . (2001) 31:625–36. doi: 10.1046/j.1365-2222.2001.01068.x
111. Drakaki E, Dessinioti C, Antoniou C. Air pollution and the skin. Front Environ Sci Eng China . (2014) 15:2–8. doi: 10.3389/fenvs.2014.00011
112. Weisskopf MG, Kioumourtzoglou M-A, Roberts AL. Air pollution and autism spectrum disorders: causal or confounded? Curr Environ Health Rep . (2015) 2:430–9. doi: 10.1007/s40572-015-0073-9
113. Mo Z, Fu Q, Lyu D, Zhang L, Qin Z, Tang Q, et al. Impacts of air pollution on dry eye disease among residents in Hangzhou, China: a case-crossover study. Environ Pollut . (2019) 246:183–9. doi: 10.1016/j.envpol.2018.11.109
114. Klopfer J. Effects of environmental air pollution on the eye. J Am Optom Assoc . (1989) 60:773–8.
115. Ashfaq A, Sharma P. Environmental effects of air pollution and application of engineered methods to combat the problem. J Indust Pollut Control . (2012) 29.
116. Madronich S, de Gruijl F. Skin cancer and UV radiation. Nature . (1993) 366:23–9. doi: 10.1038/366023a0
117. Teramura A. Effects of UV-B radiation on the growth and yield of crop plants. Physiol Plant . (2006) 58:415–27. doi: 10.1111/j.1399-3054.1983.tb04203.x
118. Singh E, Tiwari S, Agrawal M. Effects of elevated ozone on photosynthesis and stomatal conductance of two soybean varieties: a case study to assess impacts of one component of predicted global climate change. Plant Biol Stuttg Ger . (2009) 11(Suppl. 1):101–8. doi: 10.1111/j.1438-8677.2009.00263.x
119. Manderson L. How global Warming is Adding to the Health Risks of Poor People . The Conversation. University of the Witwatersrand. Available online at: http://theconversation.com/how-global-warming-is-adding-to-the-health-risks-of-poor-people-109520 (accessed October 5, 2019).
120. Ministers of Energy and Environment. Federal/Provincial/Territorial Ministers of Energy and Environment (Canada), editor. The Canada-Wide Acid Rain Strategy for Post-2000 . Halifax: The Ministers (1999). 11 p.
121. Zuhara S, Isaifan R. The impact of criteria air pollutants on soil and water: a review. (2018) 278–84. doi: 10.30799/jespr.133.18040205
122. WHO. First WHO Global Conference on Air Pollution and Health. (2018). Available online at: https://www.who.int/airpollution/events/conference/en/ (accessed October 6, 2019).
123. What is the Kyoto Protocol? UNFCCC . Available online at: https://unfccc.int/kyoto__protocol (accessed October 6, 2019).
124. CopenhagenClimate Change Conference (UNFCCC) . Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
125. Durban Climate Change Conference,. UNFCCC (2011). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
126. Paris Climate Change Agreement,. (2016). Available online at: https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
Keywords: air pollution, environment, health, public health, gas emission, policy
Citation: Manisalidis I, Stavropoulou E, Stavropoulos A and Bezirtzoglou E (2020) Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 8:14. doi: 10.3389/fpubh.2020.00014
Received: 17 October 2019; Accepted: 17 January 2020; Published: 20 February 2020.
Reviewed by:
Copyright © 2020 Manisalidis, Stavropoulou, Stavropoulos and Bezirtzoglou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ioannis Manisalidis, giannismanisal@gmail.com ; Elisavet Stavropoulou, elisabeth.stavropoulou@gmail.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders (3), leading to infant mortality or chronic disease in adult age (6). National reports have mentioned the increased risk of morbidity and mortality (1).
Abstract. Air pollution is a pressing global environmental challenge with far-reaching consequences for human health and well-being. This research paper presents an extensive examination of air ...
Air pollution is defined as all destructive effects of any sources which contribute to the pollution of the atmosphere and/or deterioration of the ecosystem. Air pollution is caused by both human interventions and/or natural phenomena. It is made up of many kinds of pollutants including materials in solid, liquid, and gas phases. Air pollutions ...
Overall, four in 10 people exposed to unsafe PM2.5 levels live on less than $5.50 a day. Of the 716 million people living in extreme poverty and exposed to unsafe levels of air pollution, almost ...
Epidemiologic research and quantitative risk assessment play a crucial role in transferring fundamental scientific knowledge to policymakers so they can take action to reduce the burden of ambient air pollution. This commentary addresses several challenges in quantitative risk assessment of air pollution that require close attention. The background to this discussion provides a summary of and ...
The aim of this brief review article is to summarise the increased health hazards to emerge from PM air pollution research in recent years, drawing upon findings published in international projects (WHO 2012, 2013a), Health Effects Institute (HEI) research reports (HEI 2010, 2013a, b), authoritative reviews (Brook et al. 2010) and important ...
Despite progress in many countries, air pollution, and especially fine particulate matter air pollution (PM2.5) remains a global health threat: over 6 million premature cardiovascular and respiratory deaths/yr. have been attributed to household and outdoor air pollution. In this viewpoint, we identify present gaps in air pollution monitoring and regulation, and how they could be strengthened ...
Air pollution is high on the global agenda and is widely recognised as a threat to both public health and economic progress. The World Health Organization (WHO) estimates that 4.2 million deaths ...
As part of the Clean Air collection we highlight papers Nature Communications has published that look at how policy and technology can be part of the solution to air pollution. The high air ...
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders (3), leading to infant mortality or chronic disease in adult age (6). National reports have mentioned the increased risk of morbidity and mortality (1).