- Open access
- Published: 22 August 2017

Social conditions of becoming homelessness: qualitative analysis of life stories of homeless peoples
- Mzwandile A. Mabhala ORCID: orcid.org/0000-0003-1350-7065 1 , 3 ,
- Asmait Yohannes 2 &
- Mariska Griffith 1
International Journal for Equity in Health volume 16 , Article number: 150 ( 2017 ) Cite this article
71k Accesses
53 Citations
20 Altmetric
Metrics details
It is increasingly acknowledged that homelessness is a more complex social and public health phenomenon than the absence of a place to live. This view signifies a paradigm shift, from the definition of homelessness in terms of the absence of permanent accommodation, with its focus on pathways out of homelessness through the acquisition and maintenance of permanent housing, to understanding the social context of homelessness and social interventions to prevent it.
However, despite evidence of the association between homelessness and social factors, there is very little research that examines the wider social context within which homelessness occurs from the perspective of homeless people themselves. This study aims to examine the stories of homeless people to gain understanding of the social conditions under which homelessness occurs, in order to propose a theoretical explanation for it.
Twenty-six semi-structured interviews were conducted with homeless people in three centres for homeless people in Cheshire North West of England.
The analysis revealed that becoming homeless is a process characterised by a progressive waning of resilience capacity to cope with life challenges created by series of adverse incidents in one’s life. The data show that final stage in the process of becoming homeless is complete collapse of relationships with those close to them. Most prominent pattern of behaviours participants often describe as main causes of breakdown of their relationships are:
engaging in maladaptive behavioural lifestyle including taking drugs and/or excessive alcohol drinking
Being in trouble with people in authorities.
Homeless people describe the immediate behavioural causes of homelessness, however, the analysis revealed the social and economic conditions within which homelessness occurred. The participants’ descriptions of the social conditions in which were raised and their references to maladaptive behaviours which led to them becoming homeless, led us to conclude that they believe that their social condition affected their life chances: that these conditions were responsible for their low quality of social connections, poor educational attainment, insecure employment and other reduced life opportunities available to them.
It is increasingly acknowledged that homelessness is a more complex social and public health phenomenon than the absence of a place to live. This view signifies a paradigm shift, from the definition of homelessness in terms of the absence of permanent accommodation [ 1 , 2 , 3 , 4 , 5 ], with its focus on pathways out of homelessness through the acquisition and maintenance of permanent housing [ 6 ], to understanding the social context of homelessness and social interventions to prevent it [ 6 ].
Several studies explain the link between social factors and homelessness [ 6 , 7 , 8 , 9 , 10 ]. The most common social explanations centre on seven distinct domains of deprivation: income; employment; health and disability; education, skills and training; crime; barriers to housing and social support services; and living environment [ 11 ]. Of all forms, income deprivation has been reported as having the highest risk factors associated with homelessness [ 7 , 12 , 13 , 14 ]: studies indicate that people from the most deprived backgrounds are disproportionately represented amongst the homeless [ 7 , 13 ]. This population group experiences clusters of multiple adverse health, economic and social conditions such as alcohol and drug misuse, lack of affordable housing and crime [ 10 , 12 , 15 ]. Studies consistently show an association between risk of homelessness and clusters of poverty, low levels of education, unemployment or poor employment, and lack of social and community support [ 7 , 10 , 13 , 16 ].
Studies in different countries throughout the world have found that while the visible form of homelessness becomes evident when people reach adulthood, a large proportion of homeless people have had extreme social disadvantage and traumatic experiences in childhood including poverty, shortage of social housing stocks, disrupted schooling, lack of social and psychological support, physical, sexual, and emotional abuse, neglect, dysfunctional family environments, and unstable family structures, all of which increase the likelihood of homelessness [ 10 , 13 , 14 ].
Furthermore, a large body of evidence suggests that people exposed to diverse social disadvantages at an early age are less likely to adapt successfully compared to people without such exposure [ 9 , 10 , 13 , 17 ], being more susceptible to adopting maladaptive coping behaviours such as theft, trading sex for money, and selling or using drugs and alcohol [ 7 , 9 , 18 , 19 ]. Studies show that these adverse childhood experiences tend to cluster together, and that the number of adverse experiences may be more predictive of negative adult outcomes than particular categories of events [ 17 , 20 ]. The evidence suggests that some clusters are more predictive of homelessness than others [ 7 , 12 ]: a cluster of childhood problems including mental health and behavioural disorders, poor school performance, a history of foster care, and disrupted family structure was most associated with adult criminal activities, adult substance use, unemployment and subsequent homelessness [ 12 , 17 , 21 ]. However, despite evidence of the association between homelessness and social factors, there is very little research that examines the wider social context within which homelessness occurs from the perspective of homeless people themselves.
This paper adopted Anderson and Christian’s [ 18 ] definition, which sees homelessness as a ‘function of gaining access to adequate, affordable housing, and any necessary social support needed to ensure the success of the tenancy’. Based on our synthesis of the evidence, this paper proposes that homelessness is a progressive process that begins at childhood and manifests itself at adulthood, one characterised by loss of the personal resources essential for successful adaptation. We adopted the definition of personal resources used by DeForge et al. ([ 7 ], p. 223), which is ‘those entities that either are centrally valued in their own right (e.g. self-esteem, close attachment, health and inner peace) or act as a means to obtain centrally valued ends (e.g. money, social support and credit)’. We propose that the new paradigm focusing on social explanations of homelessness has the potential to inform social interventions to reduce it.
In this study, we examine the stories of homeless people to gain understanding of the conditions under which homelessness occurs, in order to propose a theoretical explanation for it.
The design of this study was philosophically influenced by constructivist grounded theory (CGT). The aspect of CGT that made it appropriate for this study is its fundamental ontological belief in multiple realities constructed through the experience and understanding of different participants’ perspectives, and generated from their different demographic, social, cultural and political backgrounds [ 22 ]. The researchers’ resulting theoretical explanation constitutes their interpretation of the meanings that participants ascribe to their own situations and actions in their contexts [ 22 ].
The stages of data collection and analysis drew heavily on other variants of grounded theory, including those of Glaser [ 23 ] and Corbin and Strauss [ 24 ].
Setting and sampling strategy
The settings for this study were three centres for homeless people in two cities (Chester and Crewe) in Cheshire, UK. Two sampling strategies were used in this study: purposive and theoretical. The study started with purposive sampling and in-depth one-to-one semi-structured interviews with eight homeless people to generate themes for further exploration.
One of the main considerations for the recruitment strategy was to ensure that the process complies with the ethical principles of voluntary participation and equal opportunity to participate. To achieve this, an email was sent to all the known homeless centres in the Cheshire and Merseyside region, inviting them to participate. Three centres agreed to participate, all of them in Cheshire – two in Chester and one in Crewe.
Chester is the most affluent city in Cheshire and Merseyside, and therefore might not be expected to be considered for a homelessness project. The reasons for including it were: first, it was a natural choice, since the organisations that funded the project and the one that led the research project were based in Chester; second, despite its affluence, there is visible evidence of homelessness in the streets of Chester; and third, it has several local authority and charity-funded facilities for homeless people.
The principal investigator spent 1 day a week for 2 months in three participating centres, during that time oral presentation of study was given to all users of the centre and invited all the participants to participate and written participants information sheet was provided to those who wished to participate. During that time the principal investigator learned that the majority of homeless people that we were working with in Chester were not local. They told us that they came to Chester because there was no provision for homeless people in their former towns.
To help potential participants make a self-assessment of their suitability to participate without unfairly depriving others of the opportunity, participants information sheet outline criteria that potential participants had to meet: consistent with Economic and Social Research Council’s Research Ethics Guidebook [ 25 ], at the time of consenting to and commencing the interview, the participant must appear to be under no influence of alcohol or drugs, have a capacity to consent as stipulated in England and Wales Mental Capacity Act 2005 [ 26 ], be able to speak English, and be free from physical pain or discomfort.
As categories emerged from the data analysis, theoretical sampling was used to refine undeveloped categories in accordance with Strauss and Corbin’s [ 27 ] recommendations. In total 26 semi-structured interviews were carried out. Theoretical sampling involved review of memos or raw data, looking for data that might have been overlooked [ 27 , 28 ], and returning to key participants asking them to give more information on categories that seemed central to the emerging theory [ 27 , 28 ].
The sample comprised of 22 male and 4 female, the youndgest participant was 18 the eldest was 74 years, the mean age was 38.6 years. Table 1 illustrates participant’s education history, childhood living arrangements, brief participants family and social history, emotional and physical health, the onset of and trigger for homelessness.
Ethical approval
Ethical approval was obtained from the Research Ethics Committee of the University of Chester. The centre managers granted access once ethical approval had been obtained, and after their review of the study design and other research material, and of the participant information sheet which included a letter of invitation highlighting that participation was voluntary.
Data analysis
In this study data collection and analysis occurred simultaneously. Analysis drew on Glaser’s [ 23 ] grounded theory processes of open coding, use of the constant comparative method, and the iterative process of data collection and data analysis to develop theoretical explanation of homelessness.
The process began by reading the text line-by-line identifying and open coding the significant incidents in the data that required further investigation. The findings from the initial stage of analysis are published in Mabhala [ 29 ]. The the second stage the data were organised into three themes that were considered significant in becoming homeless (see Fig. 1 ):
Engaging in maladaptive behaviour
Being in trouble with the authorities.
Being in abusive environments.
Social explanation of becoming homeless. Legend: Fig. 1 illustrates the process of becoming homeless
The key questions that we asked as we continued to interrogate the data were: What category does this incident indicate? What is actually happening in the data? What is the main concern being faced by the participants? Interrogation of the data revealed that participants were describing the process of becoming homeless.
The comparative analysis involved three processes described by Glaser ([ 23 ], p. 58–60): each incident in the data was compared with incidents from both the same participant and other participants, looking for similarities and differences. Significant incidents were coded or given labels that represented what they stood for, and similarly coded or labeled when they were judged to be about the same topic, theme or concept.
After a period of interrogation of the data, it was decided that the two categories - destabilising behaviour, and waning ofcapacity for resilience were sufficiently conceptual to be used as theoretical categories around which subcategories could be grouped (Fig. 1 ).
Once the major categories had been developed, the next step consisted of a combination of theoretical comparison and theoretical sampling. The emerging categories were theoretically compared with the existing literature. Once this was achieved, the next step was filling in and refining the poorly defined categories. The process continued until theoretical sufficiency was achieved.
Figure 1 illustrates the process of becoming homeless. The analysis revealed that becoming homeless is a process characterised by a progressive waning of resilience created by a series of adverse incidents in one’s life. Amongst the frequently cited incidents were being in an abusive environment and losing a significant person in one’s life. However, being in an abusive environment emerged from this and previously published studies as a major theme; therefore, we decided to analyse it in more detail.
The data further show that the final stage in the process of becoming homeless is a complete collapse of relationships with those with whom they live. The most prominent behaviours described by the participants as being a main cause of breakdown are:
Engaging in maladaptive behaviour: substance misuse, alcoholism, self-harm and disruptive behaviours
Being in trouble with the authorities: theft, burglary, arson, criminal offenses and convictions
The interrogation of data in relation to the conditions within which these behaviours occurred revealed that participants believed that their social contexts influenced their life chance, their engagement with social institution such as education and social services and in turn their ability to acquire and maintain home. Our experiences have also shown that homeless people readily express the view that behavioural lifestyle factors such as substance misuse and engaging in criminal activities are the causes of becoming homeless. However, when we spent time talking about their lives within the context of their status as homeless people, we began to uncover incidents in their lives that appeared to have weakened their capacity to constructively engage in relationships, engage with social institutions to make use of social goods [ 29 , 30 , 31 ] and maturely deal with societal demands.
Being in abusive environments
Several participants explicitly stated that their childhood experiences and damage that occurred to them as children had major influences on their ability to negotiate their way through the education system, gain and sustain employment, make appropriate choices of social networks, and form and maintain healthy relationships as adults.
It appears that childhood experiences remain resonant in the minds of homeless participants, who perceive that these have had bearing on their homelessness. Their influence is best articulated in the extracts below. When participants were asked to tell their stories of what led to them becoming homeless, some of their opening lines were:
What basically happened, is that I had a childhood of so much persistent, consistent abuse from my mother and what was my stepfather. Literally consistent, we went around with my mother one Sunday where a friend had asked us to stay for dinner and mother took the invitation up because it saved her from getting off her ass basically and do anything. I came away from that dinner genuinely believing that the children in that house weren’t loved and cared for, because they were not being hit, there was no shouting, no door slamming. [Marco]
It appears that Marco internalised the incidents of abuse, characterised by shouting, door slamming and beating as normal behaviour. He goes on to intimate how the internalised abusive behaviour affected his interaction with his employers.
‘…but consistently being put down, consistently being told I was thick, I started taking jobs and having employers effing and blinding at me. One employer actually used a “c” word ending in “t” at me quite frequently and I thought it was acceptable, which obviously now I know it’s not. So I am taking on one job after another that, how can I put it? That no one else would do basically. I was so desperate to work and earn my own money. [Marco]
Similarly, David makes a connection between his childhood experience and his homelessness. When he was asked to tell his life story leading to becoming homeless, his opening line was:
I think it [homelessness] started off when I was a child. I was neglected by my mum. I was physically and mentally abused by my mum. I got put into foster care, when I left foster care I was put in the hostel, from there I turn into alcoholic. Then I was homeless all the time because I got kicked out of the hostels, because you are not allowed to drink in the hostel. [David]
David and Marco’s experiences are similar to those of many participants. The youngest participant in this study, Clarke, had fresh memories of his abusive environment under his stepdad:
I wouldn't want to go back home if I had a choice to, because before I got kicked out me stepdad was like hitting me. I wouldn't want to go back to put up with that again. [I didn't tell anyone] because I was scared of telling someone and that someone telling me stepdad that I've told other people. ‘[Be] cause he might have just started doing again because I told people. It might have gotten him into trouble. [Clarke]
In some cases, participants expressed the beliefs that their abusive experience not only deprived them life opportunities but also opportunities to have families of their own. As Tom and Marie explain:
We were getting done for child neglect because one of our child has a disorder that means she bruise very easily. They all our four kids into care, social workers said because we had a bad childhood ourselves because I was abused by my father as well, they felt that we will fail our children because we were failed by our parents. We weren’t given any chance [Tom and Marie]
Norma, described the removal of her child to care and her maladaptive behaviour of excessive alcohol use in the same context as her experience of sexual abuse by her father.
I had two little boys with me and got took off from me and put into care. I got sexually abused by my father when I was six. So we were put into care. He abused me when I was five and raped me when I was six. Then we went into care all of us I have four brothers and four sisters. My dad did eighteen months for sexually abusing me and my sister. I thought it was normal as well I thought that is what dads do [Norma]
The analysis of participants in this study appears to suggest that social condition one is raised influence the choice of social connections and life partner. Some participants who have had experience of abuse as children had partner who had similar experience as children Tom and Marie, Lee, David and his partners all had partners who experienced child abuse as children.
Tom and Marie is a couple we interviewed together. They met in hostel for homeless people they have got four children. All four children have been removed from them and placed into care. They sleep rough along the canal. They explained:
We have been together for seven years we had a house and children social services removed children from us, we fell within bedroom tax. …we received an eviction order …on the 26th and the eviction date was the 27th while we were in family court fighting for our children. …because of my mental health …they were refusing to help us.
Our children have been adopted now. The adoption was done without our permission we didn’t agree to it because we wanted our children home because we felt we were unfairly treated and I [Marie] was left out in all this and they pin it all on you [Tom] didn’t they yeah, my [Tom] history that I was in care didn’t help.
Tom went on to talk about the condition under which he was raised:
I was abandoned by my mother when I was 12 I was then put into care; I was placed with my dad when I was 13 who physically abused me then sent back to care. [Tom].
David’s story provides another example of how social condition one is raised influence the choice of social connections and life partner. David has two children from two different women, both women grew up in care. Lisa one of David’s child mother is a second generation of children in care, her mother was raised in care too.
I drink to deal with problems. As I say I’ve got two kids with my girlfriend Kyleigh, but I got another lad with Lisa, he was taken off me by social services and put on for adoption ten years ago and that really what started it; to deal with that. Basically, because I was young, and I had been in care and the way I had been treated by my mum. Basically laid on me in the same score as my mum and because his mum [Lisa] was in care as well. So they treated us like that, which was just wrong. [David]
In this study, most participants identified alcohol or drugs and crime as the cause of relationships breakdown. However, the language they used indicates that these were secondary reasons rather than primary reasons for their homelessness. The typical question that MA and MG asked the interview participants was “tell us how did you become homeless”? Typically, participants cited different maladaptive behaviours to explain how they became homeless.
Alvin’s story is typical of:
Basically I started off as a bricklayer, … when the recession hit, there was an abundance of bricklayers so the prices went down in the bricklaying so basically with me having two young children and the only breadwinner in the family... so I had to kinda look for factory work and so I managed to get a job… somewhere else…. It was shift work like four 12 hour days, four 12 hour nights and six [days] off and stuff like that, you know, real hard shifts. My shift was starting Friday night and I’ll do Friday night, Saturday night to Monday night and then I was off Tuesday, Wednesday and Thursday, but I’d treat that like me weekend you know because I’ve worked all weekend. Then… so I’d have a drink then and stuff like that, you know. 7 o’ clock on a Monday morning not really the time to be drinking, but I used to treat it like me weekend. So we argued, me and my ex-missus [wife], a little bit and in the end we split up so moved back to me mum's, but kept on with me job, I was at me mum’s for possibly about five years and but gradually the drinking got worse and worse, really bad. I was diagnosed with depression and anxiety. … I used to drink to get rid of the anxiety and also to numb the pain of the breakup of me marriage really, you know it wasn’t good, you know. One thing led to another and I just couldn’t stop me alcohol. I mean I’ve done drugs you know, I was into the rave scene and I’ve never done hard drugs like heroin or... I smoke cannabis and I use cocaine, and I used to go for a pint with me mates and that. It all came to a head about November/December time, you know it was like I either stop drinking or I had to move out of me mum's. I lost me job in the January through being over the limit in work from the night before uum so one thing led to another and I just had to leave. [Alvin]
Similarly, Gary identified alcohol as the main cause of his relationship breakdown. However, when one listens to the full story alcohol appears to be a manifestation of other issues, including financial insecurities and insecure attachment etc.
It [the process of becoming homeless] mainly started with the breakdown of the relationship with me partner. I was with her for 15 years and we always had somewhere to live but we didn't have kids till about 13 years into the relationship. The last two years when the kids come along, I had an injury to me ankle which stopped me from working. I was at home all day everyday. …I was drinking because I was bored. I started drinking a lot ‘cause I couldn't move bout the house. It was a really bad injury I had to me ankle. Um, and one day me and me partner were having this argument and I turned round and saw my little boy just stood there stiff as a board just staring, looking at us. And from that day on I just said to me partner that I'll move out, ‘cause I didn't want me little boy to be seeing this all the time. [Gary]
In both cases Gary and Alvin indicate that changes in their employment status created conditions that promoted alcohol dependency, though both explained that they drank alcohol before the changes in their employment status occurred and the breakdown of relationships. Both intimated that that their job commitment limited the amount of time available to drink alcohol. As Gary explained, it is the frequency and amount of alcohol drinking that changed as a result of change in their employment status:
I used to have a bit of a drink, but it wasn’t a problem because I used to get up in the morning and go out to work and enjoy a couple of beers every evening after a day’s work. Um, but then when I wasn't working I was drinking, and it just snowballed out, you know snowball effect, having four cans every evening and then it went from there. I was drinking more ‘cause I was depressed. I was very active before and then I became like non-active, not being able to do anything and in a lot of pain as well. [Gary]
Furthermore, although the participants claim that drinking alcohol was not a problem until their employment circumstances changed, one gets a sense that alcohol was partly responsible for creating conditions that resulted in the loss of their jobs. In Gary’s case, for example, alcohol increased his vulnerability to the assault and injuries that cost him his job:
I got assaulted, kicked down a flight of stairs. I landed on me back on the bottom of the stairs, but me heel hit the stairs as it was still going up if you know what I mean. Smashed me heel, fractured me heel… So, by the time I got to the hospital and they x-rayed it they wasn't even able to operate ‘cause it was in that many pieces, they weren't even able to pin it if you know what I mean. [Gary]
Alvin, of the other hand, explained that:
I lost my job in the January through being over the limit in work from the night before, uum so one thing led to another and I just had to leave. [Alvin]
In all cases participants appear to construct marriage breakdown as an exacerbating factor for their alcohol dependence. Danny, for example, constructed marriage breakdown as a condition that created his alcohol dependence and alcohol dependence as a cause of breakdown of his relationship with his parents. He explains:
I left school when I was 16. Straight away I got married, had children. I have three children and marriage was fine. Umm, I was married for 17 years. As the marriage broke up I turned to alcohol and it really, really got out of control. I moved in with my parents... It was unfair for them to put up with me; you know um in which I became... I ended up on the streets, this was about when I was 30, 31, something like that and ever since it's just been a real struggle to get some permanent accommodation. [Danny]
Danny goes on to explain:
Yes [I drank alcohol before marriage broke down but] not very heavily, just like a sociable drink after work. I'd call into like the local pub and have a few pints and it was controlled. My drinking habit was controlled then. I did go back to my parents after my marriage break up, yes. I was drinking quite heavily then. I suppose it was a form of release, you know, in terms of the alcohol which I wish I'd never had now. When I did start drinking heavy at me parents’ house, I was getting in trouble with the police being drunk and disorderly. That was unfair on them. [Danny]
The data in this study indicate that homelessness occurs when the relationships collapse, irrespective of the nature of the relationship. There were several cases where lifestyle behaviour led to a relationship collapse between child and parents or legal guardians.
In the next excerpt, Emily outlines the incidents: smoking weed, doing crack and heroin, and drinking alcohol. She also uses the words ‘because’, ‘when’ and ‘obviously’, which provide clues about the precipitating condition for her behaviours “spending long time with people who take drugs”.
I've got ADHD like, so obviously my mum kicked me out when I was 17 and then like I went to **Beswick** and stuff like that. My mum in the end just let me do what I wanted to do, ‘cause she couldn't cope anymore. …I mean I tried to run away from home before that, but she'd always like come after me in like her nightie and pyjamas and all that. But in the end she just washed her hands of me . [Emily]
Emily presented a complex factors that made it difficult for her mother to live with her. These included her mother struggle with raising four kids as a single parent, Emily’s mental health (ADHD], alcohol and drug use. She goes on to explain that:
Ummm, well the reason I got kicked out of my hostel was ‘cause of me drinking, so I'd get notice to quit every month, then I’d have a meeting with the main boss and then they'd overturn it and this went on every month for about six months. Also, it was me behaviour as well, but obviously drink makes you do stuff you don't normally do and all that shit. I lived here for six months, got kicked out because I jumped out the window and broke me foot. I was on the streets for six months and then they gave me a second chance and I've been here a year now. So that's it basically. [Emily]
There were several stories of being evicted from accommodation due to excessive use of alcohol. One of those is David:
I got put into foster care. When I left foster care I was put in the hostel, from there I turn into alcoholic. Then I was homeless all the time because I got kicked out of the hostels, because you are not allowed to drink in the hostel. It’s been going on now for about… I was thirty-one on Wednesday, so it’s been going on for about thirteen years, homeless on and off. Otherwise if not having shoplifted for food and then go to jail, and when I don’t drink I have lot of seizures and I end up in the hospital. Every time I end up on the street. I trained as a chef, I have not qualified yet, because of alcohol addiction, it didn’t go very well. I did couple of jobs in restaurants and diners, I got caught taking a drink. [David]
Contrary to the other incidents where alcohol was a factor that led to homelessness, Barry’s description of his story appears to suggest that the reason he had to leave his parents’ home was his parents’ perception that his sexuality brought shame to the family:
When I came out they I’m gay, my mum and dad said you can’t live here anymore. I lived in a wonderful place called Nordic... but fortunately, mum and dad ran a pub called […] [and] one of the next door neighbours lived in a mansion. His name was [….] [and] when I came out, he came out as in he said “I'm a gay guy”, but he took me into Liverpool and housed me because I had nowhere to live. My mum and dad said you can't live here anymore. And unfortunately, we get to the present day. I got attacked. I got mugged... only walked away with a £5 note, it’s all they could get off me. They nearly kicked me to death so I was in hospital for three weeks. By the time I came out, I got evicted from my flat. I was made homeless. [Barry]
We used the phrase “engaging in maladaptive behaviour” to conceptualise the behaviours that led to the loss of accommodation because our analysis appear to suggest that these behaviours were strategies to cope with the conditions they found themselves in. For example, all participants in this category explained that they drank alcohol to cope with multiple health (mental health) and social challenges.
In the UK adulthood homelessness is more visible than childhood homelessness. However, most participants in this research reveal that the process of becoming homeless begins at their childhood, but becomes visible after the legal age of consent (16). Participants described long history of trouble with people in authority including parents, legal guardians and teachers. However, at the age of 16 they gain legal powers to leave children homes, foster homes, parental homes and schools, and move outside some of the childhood legal protections. Their act of defiance becomes subject to interdiction by the criminal justice system. This is reflected in number of convictions for criminal offenses some of the participants in this study had.
Participants Ruddle, David, Lee, Emily, Pat, Marco, Henry and many other participants in this study (see Table 1 ) clearly traced the beginning of their troubles with authority back at school. They all expressed the belief that had their schooling experience been more supportive, their lives would have been different. Lee explains that being in trouble with the authorities began while he was at school:
‘The school I came from a rough school, it was a main school, it consisted of A, B, C, D and The school I came from [was] a rough school, it was a main school, it consisted of A, B, C, D and E. I was in the lowest set, I was in E because of my English and maths. I was not interested, I was more interested in going outside with big lads smoking weed, bunking school. I used to bunk school inside school. I used to bunk where all cameras can catch me. They caught me and reported me back to my parents. My mum had a phone call from school asking where your son is. My mum grounded me. While my mum grounded me I had a drain pipe outside my house, I climbed down the drain pipe outside my bedroom window. I used to climb back inside. [Lee]
Lee’s stories constructed his poor education experiences as a prime mover towards the process of becoming homeless. It could be noted in Table 1 that most participants who described poor education experiences came from institutions such as foster care, children home and special school for maladjusted children. These participants made a clear connection between their experiences of poor education characterised by defiance of authorities and poor life outcomes as manifested through homelessness.
Patrick made a distinct link between his school experience and his homelessness, for example, when asked to tell his story leading up to becoming homeless, Patrick’s response was:
I did not go to school because I kept on bunking. When I was fifteen I left school because I was caught robbing. The police took me home and my mum told me you’re not going back to school again, you are now off for good. Because if you go back to school you keep on thieving, she said I keep away from them lads. I said fair enough. When I was seventeen I got run over by a car. [Patrick]
Henry traces the beginning of his troubles with authorities back at school:
[My schooling experience]… was good, I got good, well average grades, until I got myself into [a] few fights mainly for self-defence. In primary schools, I had a pretty... I had a good report card. In the start of high school, it was good and then when the fights started that gave me sort of like a... bad reputation. I remember my principal one time made me cry. Actually made me cry, but eh... I don't know how, but I remember sitting there in the office and I was crying. My sister also stuck up for me when she found out what had happened, she was on my side; but I can’t remember exactly what happened at that time. [Henry]
Emily’s story provides some clues about the series of incidents - including, delay in diagnosing her health condition, being labelled as a naughty child at school, being regularly suspended from school and consequently poor educational attainment.
Obviously, I wasn't diagnosed with ADHD till I was like 13, so like in school they used to say that's just a naughty child. … So it was like always getting suspended, excluded and all that sort of stuff. And in the end [I] went to college and the same happened there. [Emily]
The excerpt above provides intimations of what she considers to be the underlying cause of her behaviour towards the authorities. Emily suggests that had the authorities taken appropriate intervention to address her condition, her life outcomes would have been different.
Although the next participant did not construct school as being a prime mover of their trouble with authorities, their serious encounters with the criminal justice system occurred shortly after leaving school:
Well I did a bit of time at a very early age, I was only 16… I did some remand there, but then when I went to court ‘cause I'd done enough remand, I got let out and went to YMCA in Runcorn. Well, that was when I was a kid. When I was a bit older, ‘cause it was the years 2000 that I was in jail, I was just trying to get by really. I wasn’t with Karen at the time. I was living in Crewe and at the time I was taking a lot of amphetamines and was selling amphetamines as well, and I got caught and got a custodial sentence for it. But I've never been back to jail since. I came out in the year 2000 so it's like 16 years I've kept meself away from jail and I don't have any intentions of going back. [Gary]
The move from school and children social care system to criminal justice was a common pathways for many participants in this study. Some including Lee, Crewe, David, Patrick spent multiple prison sentences (see Table 1 ). Although Crewe did not make connection between his schooling experiences and his trouble with law, it could be noted that his serious encounter with criminal justice system started shortly after leaving foster care and schooling systems. As he explains:
I was put into prison at age of 17 for arson that was a cry for help to get away from the family, I came out after nine months. I have been in prison four times in my life, its not very nice, when I came out I made a promise to myself that I’m never going to go back to prison again. [Crewe]
Lee recalls his education experience. He explained:
I left school when I was fifteen… then I went off the rails. I got kidnapped for three and half months. When I came back I was just more interested in crime. When I left school I was supposed to go to college, but I went with travellers. I was just more interested in getting arrested every weekend, until my mum say right I have enough of you. I was only seventeen. I went through the hostels when I was seventeen. [Lee]
None describe the educational experience with a similar profundity to Marco:
On few occasions I came out on the corridors I would be getting battered on to my hands and knees and teachers walk pass me. There was quite often blood on the floor from my nose, would be punched on my face and be thrown on the floor. …. It was hard school, pernicious. I would go as far as saying I never felt welcome in that school, I felt like a fish out of the water, being persistently bullied did my head in. Eventually I started striking back, when I started striking back suddenly I was a bad one. My mother decided to put me in … school for maladjusted boys, everyone who been there including myself have spent time in prison. [Marco]
The trouble with authorities that was observes in participants stories in this category appear to be part of the wider adverse social challenges that the participants in this study were facing. Crewe’s description of arson as a cry for help appears to be an appropriate summation of all participants in this category.
The participants’ description of the social conditions in which were raised and their references to maladaptive behaviours which led to them becoming homeless, led us to conclude that they believe that their social condition affected their life chances: that these conditions were responsible for their low quality of social connections, poor educational attainment, insecure employment and other reduced life opportunities available to them.
The key feature that distinguish this study from comparable previous studies is that it openly acknowledges that data collection and analysis were influenced by the principles of social justice [ 28 , 30 , 31 ]. The resulting theoretical explanation therefore constitutes our interpretation of the meanings that participants ascribe to their own situations and actions in their contexts. In this study, defining homelessness within the wider socioeconomic context seemed to fit the data, and offered one interpretation of the process of becoming homeless.
While the participants’ experiences leading to becoming homeless may sound trite. What is pertinent in this study is understanding the conditions within which their behaviours occurred. The data were examined through the lens of social justice and socio-economic inequalities: we analysed the social context within which these behaviours occurred. We listened to accounts of their schooling experiences, how they were raised and their social network. The intention was not to propose a cause-and-effect association, but to suggest that interventions to mitigate homelessness should consider the social conditions within which it occurred.
Participants in this study identified substance misuse and alcohol dependency as a main cause of their homelessness. These findings are consistent with several epidemiological studies that reported a prevalence of substance misuse amongst the homeless people [ 32 , 33 , 34 , 35 , 36 ]. However, most these studies are epidemiological; and by nature epidemiological studies are the ‘gold standard’ in determining causes and effects, but do not always examine the context within which the cause and effect occur. One qualitative study that explored homelessness was a Canadian study by Watson, Crawley and Cane [ 37 ]. Participants in the Watson, et al. described ‘lack of quality social interactions and pain of addition. However, Watson et al. focus on the experiences of being homeless, rather than the life experiences leading to becoming homeless. To our knowledge the current study is one of very few that specifically examine the conditions within which homelessness occurs, looking beyond the behavioural factors. Based on the synthesis of data from previous studies, it makes sense that many interventions to mitigate homelessness focus more on tackling behavioural causes of homelessness rather than fundamental determinants of it [ 38 ]. From the public health intervention’ point of view, however, understanding the conditions within which homelessness occurs is essential, as it will encourage policymakers and providers of the services for homelessness people to devote equal attention to tackling the fundamental determinants of homelessness as is granted in dealing behavioural causes.
Participants in this study reported that they have been defiant toward people in positions of authority. For most of them this trouble began when they were at school, and came to the attention of the criminal justice system as soon as they left school at the age of 16. These findings are similar to these in the survey conducted by Williams, Poyser, and Hopkins [ 39 ] which was commissioned by the UK Ministry of Justice. This survey found that 15 % of prisoners in the sample reported being homeless before custody [ 39 ]; while three and a half percent of the general population reported having ever been homeless [ 39 ]. As the current study reveals there are three possible explanations for the increased population of homeless young people in the criminal justice system: first, at the age of 16 they gain legal powers to leave their foster homes, parents homes, and schools and move beyond some of the childhood legal protections; second, prior to the age of 16 their defiant behaviours were controlled and contained by schools and parents/legal guardians; and third, after the age of 16 their acts of defiant behaviour become subject to interdiction by the criminal justice system.
The conditions in which they were born and raised were described by some participants in this study as ‘chaotic’, abusive’, ‘neglect’, ‘pernicious’ ‘familial instability’, ‘foster care’, ‘care home’, etc. Taking these conditions, and the fact that all but one participants in this left school at or before the age of 16 signifies the importance of living conditions in educational achievement. It has been reported in previous studies that children growing up in such conditions struggle to adjust in school and present with behavioural problems, and thus, poor academic performance [ 40 ]. It has also been reported that despite these families often being known to social services, criminal justice systems and education providers, the interventions in place do little to prevent homelessness [ 40 ].
Analysis of the conditions within which participants’ homelessness occurred reveals the adverse social conditions within which they were born and raised. The conditions they described included being in an abusive environment, poor education, poor employment or unemployment, poor social connections and low social cohesion. These conditions are consistent with high index of poverty [ 37 , 41 , 42 ]. And several other studies found similar associations between poverty and homelessness [ 42 ]. For example, the study by Watson, Crowley et al. [ 37 ] found that there were extreme levels of poverty and social exclusion amongst homeless people. Contrary to previous studies that appear to construct homelessness as a major form of social exclusion, the analysis of participants’ stories in this current study revealed that the conditions they were raised under limited their capacity to engage in meaningful social interactions, thus creating social exclusion.
Homeless people describe the immediate behavioural causes of homelessness; however, this analysis revealed the social and economic conditions within which homelessness occurred. The participants’ descriptions of the social conditions in which were raised and their references to maladaptive behaviours which led to them becoming homeless, led us to conclude that they believe that their social condition affected their life chances: that these conditions were responsible for their low quality of social connections, poor educational attainment, insecure employment and other reduced life opportunities available to them.
Limitations
The conclusions drawn relate only to the social and economic context of the participants in this study, and therefore may not be generalised to the wider population; nor can they be immediately applied in a different context. It has to be acknowledged that the method of recruitment of the 26 participants generates a bias in favour of those willing to talk. The methodology used in this study (constructivist grounded theory) advocates mutual construction of knowledge, which means that the researchers’ understanding and interpretations may have had some influence on the research process as the researchers are an integral part of the data collection and analysis
Department for Communities and Local Government. Statutory homelessness: October to December quarter 2015, in 26 homelessness statistical release 2016. London: Stationery Office; 2015.
Google Scholar
HM Government. Homelessness act 2002. London: UK Government; 2002.
HM Government. Homelessness reduction act 2017. London: UK government; 2017.
MH Government. Housing (Homeless Persons) act 1977. London: UK Government; 1977.
Department for Communities and Local Government. Statutory homelessness: October to December quarter 2015, in 26 homelessness statistical release 2016. London: Stationery Office; 2016.
Christian J, Abrams D, Clapham D, Nayyar D, Cotler J. Intentions to move from homelessness to social inclusion: the role of participation beliefs, attitudes and prior behaviour. Soc Incl. 2016;4643(4):16–27.
Article Google Scholar
Deforge BR, Belcher J, O’rourke M, Lindsey MA. Personal resources and homelessness in early life: predictors of depression in consumers of homeless multiservice centres. J Loss Trauma. 2008;13:222–42.
Barman-Adhikari A, Petering R, Lengnick-Hall R, Rice E, Rhoades H, McCune S. Social context of service use among homeless youth in Los Angeles, California. J Soc Serv Res. 2016;42(4):501–15.
Barman-Adhikari A, Bowen E, Bender K, Brown S, Rice E. A social capital approach to identifying correlates of perceived social support among homeless youth. Child Youth Care Forum. 2016;45(5):691–708.
Keane CA, Magee CA, Kelly PJ. Is there a complex trauma experience typology for Australians experiencing extreme social disadvantage and low housing stability? Child Abuse Negl. 2016;61:43–54.
Article PubMed Google Scholar
Department for Communities and Local Government. The English indices of deprivation 2015. London: Stationery Office; 2016.
Patterson ML, Moniruzzaman A, Somers JM. History of foster care among homeless adults with mental illness in Vancouver, British Columbia: a precursor to trajectories of risk. BMC Psychiatry. 2015;15(1):32.
Article PubMed PubMed Central Google Scholar
Fry C, Langley K, Shelton K. A systematic review of cognitive functioning among young people who have experienced homelessness, foster care and of poverty. Child Neuropsychol. 2016; doi.10.1080/09297049.2016.1207758 .
Reeve K. Welfare conditionality, benefit sanctions and homelessness in the UK: ending the ‘something for nothing culture’ or punishing the poor? J Poverty Soc Justice. 2017;25(1):65–78.
Somers J, Patterson M, Moniruzzaman A, Currie L, Rezansoff S, Palepu A. Vancouver at home: pragmatic randomized trials investigating housing first for homeless and mentally ill adults. Trials. 2013. doi: 10.1186/1745-6215-14-365 .
Watson J, Crawley J, Kane D. Social exclusion, health and hidden homelessness. Public Health. 2016;139:96–102.
Article CAS PubMed Google Scholar
Roos LE, Distasio J, Bolton S-L, Katz LY, Afifi TO, Isaak C, Goering P, Bruce L, Sareen J. A history in-care predicts unique characteristics in a homeless population with mental illness. Child Abuse Negl. 2014;38(10):1618–27.
Anderson I, Christian J. Causes of homelessness in the UK: a dynamic analysis. J Community Appl Soc Psychol. 2003;13:105–18.
Anderson I. Synthesizing homelessness research: trends, lessons and prospects. J Community Appl Soc Psychol. 2003;13:197–205.
Tsai J, Edens EL, Rosenheck RA. A typology of childhood problems among chronically homeless adults and its association with housing and clinical outcomes. J Health Care Poor Underserved. 2011;22(3):853–70.
Haskett ME, Armstrong MJ, Tinsdale J. Developmental status and social-emotional functioning of young children experiencing homelessness. Early Childhood Educ J. 2016;44:119–25.
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: SAGE Publications; 2006.
Glaser BG. Remodelling grounded theory. Hist Soc Res. 2007;Supplement 19:47–68.
Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. Los Angeles: Sage Publications; 2008.
Book Google Scholar
Economic and Social Research Council: The research ethics guidebook a resource for social scientists. 2017. http://www.ethicsguidebook.ac.uk/ . Accessed 6 June 2017.
HM Government: Mental capacity act 2005.2005. http://www.legislation.gov.uk/ukpga/2005/9/pdfs/ukpga_20050009_en.pdf . Accessed 5 June 2017.
Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. London: Sage Publication; 1998.
Mabhala M. Public health nurse educators’ conceptualisation of public health as a strategy to reduce health inequalities: a qualitative study. Int J Equity Health. 2015;14:14.
Mabhala MA, Massey A, Ellahi B, Kingston P. Understanding the determinants of homelessness through examining the life stories of homeless people and those who work with them: a qualitative research protocol. Diversity Equality Health Care. 2016;13(4):284–9.
Mabhala M. Social justice and global perspectives on health improvement in health improvement and wellbeing strategies and actions. Maidenhead: McGrow Hill and Open University Press; 2014.
Mabhala MA. Health inequalities as a foundation for embodying knowledge within public health teaching: a qualitative study. Int J Equity Health. 2013;12:46.
North CS, Eyrich-Garg KM, Pollio DE, Thirthalli J. A prospective study of substance use and housing stability in a homeless population. Soc Psychiatric Epidemiol. 2010;45:1055–62.
Kushel M, Vittinghoff E, Haas J. Factors associated with the health care utilization of homeless persons. J Am Med Assoc. 2001;285:200–6.
Article CAS Google Scholar
Orwin RG, Scott CK, Arieira C. Transitions through homelessness and factors that predict them: three-year treatment outcomes. J Subst Abus Treat. 2005;28:S23–39.
Grinman MN, Chiu S, Redelmeier DA, Levinson W, Kiss A, Tolomiczenko G, Cowan L, Hwang SW. Drug problems among homeless individuals in Toronto, Canada: prevalence, drugs of choice, and relation to health status. BMC Public Health. 2010;10:94.
Linton SL, Celentano DD, Kirk GD, Mehta SH. The longitudinal association between homelessness, injection drug use, and injection-related risk behaviour among persons with a history of injection drug use in Baltimore, MD. Drug Alcohol Depend. 2013;132:457–65.
Crawley J, Kane D, Atkinson-Plato L, Hamilton M, Dobson K, Watson J. Needs of the hidden homeless – no longer hidden: a pilot study. Public Health. 2013;27(7): 674–80.
Office of the Deputy Prime Minister: Housing, planning, and local government and the regions committee: homelessness: third report of session 2004–05. 2005. https://www.publications.parliament.uk/pa/cm200405/cmselect/cmodpm/61/61i.pdf . Accessed 24 Oct 2016.
Williams K, Poyser J, Hopkins K. Accommodation, homelessness and reoffending of prisoners: results from the surveying prisoner crime reduction (SPCR) survey. London: Ministry of Justice; 2012.
Kennedy S. It should not be a pit stop: voices and perspectives of homeless youth on labeling and placement in special education. J Ment Health Res Intellect Disabil. 2017;10:1–19.
Lugo MA. Oxford Poverty & Human Development Initiative (OPHI): employment, in Oxford Poverty & Human Development Initiative (OPHI). Oxford: Oxford University; 2007.
Shinn M. Homelessness, poverty and social exclusion in the United States and Europe. Eur J Homelessness. 2010;4:19–43.
Download references
Acknowledgements
The authors wish to thank all participants in this study; without their contribution it would not have been possible to undertake the research. The authors acknowledge the contribution of Professor Paul Kingston and Professor Basma Ellahi at the proposal stage of this project. A very special thanks to Robert Whitehall, John and all the staff at the centres for homeless people for their help in creating a conducive environment for this study to take place; and to Roger Whiteley for editorial support. A very special gratitude goes to the reviewers of this paper, who will have expended considerable effort on our behalf.
This research was funded by quality-related research (QR) funding allocation for the University of Chester.
Availability of data and materials
The datasets generated during and/or analysed during the current study are not publicly available due to ethical restriction and privacy of participant data but are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Faculty of Health and Social Care, Department of Public Health and Wellbeing, University of Chester, Riverside Campus, Chester, CH1 1SL, UK
Mzwandile A. Mabhala & Mariska Griffith
Mount Sinai, Department of Surgery, Ambulatory Surgery Centre, 5 East 98th Street, 14th Floor, Box 1259, New York, NY, 10029-6574, USA
Asmait Yohannes
Department of Public health and Wellbeing, University of Chester, Riverside Campus, Chester, CH1 1SF, UK
Mzwandile A. Mabhala
You can also search for this author in PubMed Google Scholar
Contributions
MM wrote the entire manuscript, designed the study, collected data, analysed and interpreted data, and presented the findings. AY contributed to transcribing data and manuscript editing. MG contributed to data collection, and transcribed the majority of data. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mzwandile A. Mabhala .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval to conduct the study was provided by the Faculty of Health and Social Care Research Ethics Subcommittee of the University of Chester.
Consent for publication
All participants have given consent to publish.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Mabhala, M.A., Yohannes, A. & Griffith, M. Social conditions of becoming homelessness: qualitative analysis of life stories of homeless peoples. Int J Equity Health 16 , 150 (2017). https://doi.org/10.1186/s12939-017-0646-3
Download citation
Received : 24 March 2017
Accepted : 10 August 2017
Published : 22 August 2017
DOI : https://doi.org/10.1186/s12939-017-0646-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Homeless People
- Poor Educational Attainment
- Public Health Phenomenon
- Permanent Accommodation
- Behavioral Causes
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: journalsubmissions@springernature.com
The Center for Evidence-based Solutions to Homelessness

- Children and families
- Chronic homelessness
- Criminal justice reentry
- Homeless services system
- Homelessness prevention
- Permanent supportive housing
- Rapid re-housing
- Rental housing subsidies and homelessness
- Trends and patterns of homelessness
Related Content
Privacy overview.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Homelessness and health-related outcomes: an umbrella review of observational studies and randomized controlled trials
Michele fornaro, elena dragioti, michele de prisco, martina billeci, anna maria mondin, raffaella calati, simon hatcher, mark kaluzienski, jess g fiedorowicz, marco solmi, andrea de bartolomeis, andré f carvalho.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2022 Jan 19; Accepted 2022 May 30; Collection date 2022.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Homelessness has been associated with multiple detrimental health outcomes across observational studies. However, relatively few randomized controlled trials (RCTs) have been conducted on people who experience homelessness (PEH). Thus, this umbrella review ranked the credibility of evidence derived from systematic reviews (SRs) and meta-analyses (MAs) of observational studies investigating the associations between homelessness and any health outcome as well as RCTs targeting health needs in this population.
Several databases were systematically searched from inception through April 28, 2021. Any SR and/or MA reporting quantitative data and providing a control group were eligible for inclusion. The credibility of the evidence derived from observational studies was appraised by considering the significance level of the association and the largest study, the degree of heterogeneity, the presence of small-study effects as well as excess significance bias. The credibility of evidence was then ranked in five classes. For SRs and/or MAs of RCTs, we considered the level of significance and whether the prediction interval crossed the null. The AMSTAR-2 and AMSTAR-plus instruments were adopted to further assess the methodological quality of SRs and/or MAs. The Newcastle-Ottawa Scale (NOS) was employed to further appraise the methodological quality of prospective cohort studies only; a sensitivity analysis limited to higher quality studies was conducted.
Out of 1549 references, 8 MAs and 2 SRs were included. Among those considering observational studies, 23 unique associations were appraised. Twelve of them were statistically significant at the p ≤0.005 level. Included cases had worst health-related outcomes than controls, but only two associations reached a priori-defined criteria for convincing (class I) evidence namely hospitalization due to any cause among PEH diagnosed with HIV infection, and the occurrence of falls within the past year among PEH. According to the AMSTAR-2 instrument, the methodological quality of all included SRs and/or MAs was “critically low.” Interventional studies were scant.
While homelessness has been repeatedly associated with detrimental health outcomes, only two associations met the criteria for convincing evidence. Furthermore, few RCTs were appraised by SRs and/or MAs. Our umbrella review also highlights the need to standardize definitions of homelessness to be incorporated by forthcoming studies to improve the external validity of the findings in this vulnerable population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-022-02423-z.
Keywords: Homeless, Health outcomes, Severe mental illness, Umbrella review
Homelessness is an important social, public health, and human rights issue worldwide. The prevalence of homelessness varies among diverse countries and cultures around the world. Lifetime prevalence estimates from representative samples are 4.2% in the USA [ 1 ] to 4.9% in Europe [ 2 ]. However, high-quality data on the prevalence of homelessness in low- and middle-income countries (LMICs) is scant.
The operational definitions for homelessness likewise vary across different literature sources and settings [ 3 ] although a commonly accepted and implemented definition of homelessness globally comes from the European Typology of Homeless and Housing Exclusion study [ 4 ].
People experiencing homelessness (PEH) may face social and economic challenges that may lead to poor health, such as poverty, poor nutrition, and social exclusion. People who lack stable and appropriate housing appear to be at relatively high risk for a broad range of acute and chronic illnesses, especially infectious diseases, heart diseases, substance use disorders, and severe mental disorders [ 5 ]. However, it is unclear whether homelessness causes these disorders or otherwise these illnesses per se contribute to homelessness. Finally, evidence indicates that PEH has a lower probability of receiving proper care for their health conditions compared to the general population [ 6 ].
Data about differences in the prevalence of multiple health conditions between PEH and the general population is substantially unreliable, as exemplified by current knowledge about mental health [ 7 ] and infectious diseases among PEH [ 8 ]. Cohort and case-control studies have reported various health outcomes associated with homelessness, and several health outcomes have been the subject of a multitude of systematic reviews (SRs) and meta-analyses (MAs). While informative, this latter knowledge synthesis is usually restricted to a single outcome, and some of their results may be affected by biases, which are often poorly appraised [ 9 ]. Furthermore, randomized controlled trials (RCTs) targeting health-related outcomes in homeless populations are few, thus providing limited evidence to inform health policies [ 10 ]. Specifically, significant associations claimed by the original observational studies, or their pooled synthesis may be susceptible to biases such as excess significance [ 11 ], publication bias, reporting bias, and residual confounding, leading to misleading or inflated estimates of these associations [ 12 ].
Umbrella reviews (URs)—a systematic collection and appraisal of SRs and MAs performed on a specific topic [ 13 ]—can disentangle the aforementioned biases through appraising the quality and comprehensiveness of the data, and hence, assess which associations derived from observational studies are supported by the most credible evidence. Likewise, URs can provide a methodological appraisal of RCTs targeting a specific population or condition. Thus, in the current report, we aimed to conduct an umbrella review of the evidence from observational studies and RCTs considering multiple health outcomes involving PEH. In particular, we aimed at (i) assessing the reported association measures between homelessness and any health outcome and (ii) appraising the interventions targeting any health outcome among PEH.
Search strategy
We performed an umbrella review that included observational or RCTs that investigated the association between homelessness and any health outcome. The PubMed/MEDLINE, EMBASE, and SCOPUS databases were systematically searched from inception up to April 28, 2021. The following string was adopted for PubMed: (((“homeless persons”[MeSH Terms]) OR (“homeless youth”[MeSH Terms])) OR (“vulnerable populations”[MeSH Terms]) OR (homeless*[Title/Abstract])) AND (((((“meta analysis as topic”[MeSH Terms]) OR (“systematic reviews as topic”[MeSH Terms])) OR (“meta analysis”[Title/Abstract])) OR (“systematic review”[Title/Abstract]))). Please see Additional file 1 : material 1. The definition of homelessness and related phenomena were independently recorded by two investigators.
Eligibility criteria
For the synthesis of evidence from SRs and MAs of observational studies, we included those studies reporting any health outcome among PEH compared to the general population or otherwise provided controls (i.e., people who are not experiencing homelessness, PEH without a particular exposure). We excluded those SRs or MAs of observational studies that only provided prevalence estimates of a given health condition in PEH without providing a measure of association. Specifically, those studies reporting interventions just targeting housing, but not the related health status, were likewise excluded. The SRs and MAs of RCTs suitable for inclusion were those documenting interventions targeting any health outcome among PEH; controls were PEH exposed to a health-targeting intervention different from the health-outcome intervention delivered to PEH cases. Eligible quantitative SRs and MAs of observational studies had to include at least 3 studies; eligible SRs and MAs of intervention studies had to include at least 5 studies. The rationale for this inclusion criterion is explained in detail elsewhere [ 14 ]. In the case of multiple MAs reporting on the same topic (i.e., overlapping with the same type of intervention or exposure), we considered only the one that included the largest number of studies as it is a standard procedure in previously conducted umbrella reviews [ 15 , 16 ]. In cases there were two or more MAs pooling the same number of studies, we retained the most recent one. Qualitative reports were excluded. There were no language restrictions for the inclusion of studies for this umbrella review.
The protocol for this study was registered in PROSPERO with the following numbers: CRD42021252185, for the protocol investigating observational studies, and CRD42021252191 for the protocol that assessed evidence from intervention studies, respectively. Complete versions of each protocol are fully available online at https://osf.io/am67d/ and https://osf.io/58mhu/ .

Data extraction
Three investigators (MDP, MB, MF) independently searched title/abstracts of retrieved references for eligibility, and when a consensus could not be achieved, additional authors with considerable expertise in umbrella reviews (AFC, MS, LS) and the study of homelessness (LS, JGF, SH, MK) were consulted. The same procedure was followed at the full-text level. The reference lists of included studies were also searched for the identification of additional eligible references. Among other variables, we recorded the following: publication year, considered health outcome, study design, number of the included studies, total sample size, homelessness definition, and disclosure of sponsorship. For each primary study included in the SRs or MAs, we additionally recorded the first author, year of publication, study design (i.e., cohort, case-control, cross-sectional, RCT), setting of the study (i.e., inpatients, outpatients, population-based), number of subjects included in the study (total sample, cases, and controls), sex, ethnicity, both adjusted and unadjusted effect sizes (ES), and 95% confidence interval (CI). Intervention and mean duration of RCT studies were likewise extracted.
Data analysis and assessment of the credibility of evidence
We re-analyzed each eligible MA using the extracted individual study estimates to compute the summary effect estimates and the exact p-value under the random-effects model with DerSimonian and Laird method if included studies were equal or more than 10, and Hartung, Knapp, Sidik, and Jonkman (HKSJ) if less than 10 [ 17 , 18 ]. Cochran’s Q test and the I 2 statistics were computed for the evaluation of heterogeneity across studies ( I 2 >50% indicated high heterogeneity) [ 19 , 20 ]. To further account for heterogeneity between studies, we computed 95% prediction intervals for the summary random-effect estimates [ 21 ]. We evaluated the presence of small-study effects (i.e., large studies fetching significantly more conservative results than smaller studies) by adopting the Egger’s regression asymmetry test ( p ≤0.10) [ 22 ]. For statistically significant MAs, we assessed the presence of excess significance bias by evaluating whether the number of observed studies with nominally statistically significant results was different from the expected number of studies with statistically significant results [ 23 ]. The expected number of statistically significant studies in each association was calculated from the sum of the statistical power estimates for each component study using an algorithm from a non-central t distribution [ 24 – 26 ]. The power estimates of each component study depended on the plausible effect size of the tested association, which was assumed to be the effect size of the largest study in each MA [ 27 ]. The presence of excess significance bias for individual MAs was considered at p ≤0.10. The credibility of the evidence of each association provided by MAs of observational studies was assessed using the criteria previously applied in various medical fields [ 26 , 28 , 29 ], waiving the “number of cases” criterion since some health outcomes of PEH represent infrequent events. Briefly, the associations that presented nominally significant random-effect summary estimates were considered as “convincing” (Class I), “highly suggestive” (Class II), “suggestive” (Class III), “weak evidence” (Class IV), or “non-significant” (NS). Please, see the credibility box in Additional file 1 : Table S1. For MAs of intervention studies, we assessed the significance of the pooled effect size as P <0.005, P =0.005–0.005, and P ≥0.05 [ 30 ], the 95% prediction interval (excluding the null or not), the significance of the effect size of the largest study, and the presence of large heterogeneity (i.e., I 2 >50%) [ 31 ]. In addition, the methodological quality of those SRs and/or MAs was further appraised with the Assessment of Multiple Systematic Reviews Plus (AMSTAR-Plus) instrument [ 32 ]. All statistical tests were two-tailed. The data abstraction was performed using pre-defined Microsoft Excel® forms, while the statistical computations were carried out by an expert senior author (ED) using the STATA/SE, version 17.0 (StataCorp LLC) software. For each eligible quantitative report, two investigators (MDP and MB) independently rated the methodological quality using the AMSTAR-2 (Assessment of multiple SRs) tool [ 33 ] for quantitative SRs or MAs of observational studies. The prospective cohort studies included in the quantitative SRs or MAs of observational studies were rated for quality using the Newcastle-Ottawa scale (NOS) [ 34 ]. Finally, we adopted the following thresholds for the NOS scores: “good quality” (3-4 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), “fair quality” (2 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), and “poor quality” (0-1 stars in the “selection domain” OR 0 stars in the “comparability” domain OR 0-1 star in the “outcome” domain) [ 35 ].
The search returned 1549 potentially eligible records, of which 11 records were manually retrieved. Upon title and abstract screening, 189 records were further assessed at the full-text level, of which 179 were excluded with reasons as detailed in Additional file 1 : Table S2 [ 7 , 8 , 36 – 210 ]. Nine SRs or MAs of observational studies [ 211 – 219 ] were included, which yielded 23 comparisons. One MA of interventional studies [ 220 ] fetched two comparisons. Figure 1 provides a flowchart for study selection.
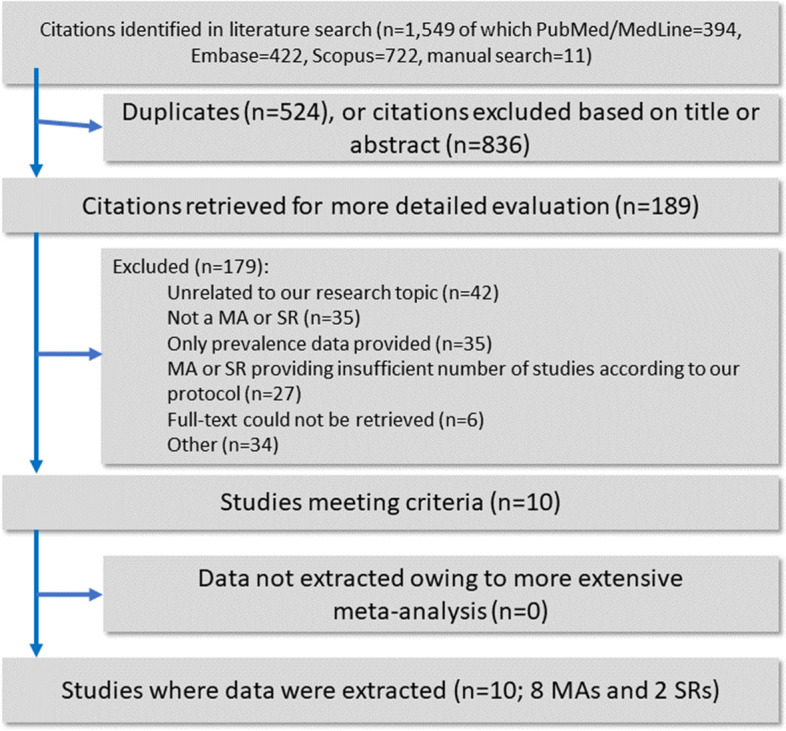
Flowchart of the literature search and evaluation process returning 10 systematic reviews and meta-analyses
Given the scant evidence for intervention studies, we decided to combine the reporting of both registration protocols into a single publication.
Descriptive characteristics of the 10 included eligible SRs and MAs of observational and intervention studies are outlined in Table 1 . The observational studies had the following control groups: PEH without SUD [ 211 ], PEH who did not inject drugs [ 212 ], people not experiencing homelessness [ 213 – 215 , 218 , 219 ], or the general population [ 216 , 217 ]. Although substantially overlapping, we nonetheless recorded “people not experiencing homelessness” and “general population” controls, as documented by the original study at review. The included MA of RCTs controlled for various treatment exposures [ 220 ].
Characteristics of the included SRs or MAs of observational and interventional studies
MA meta-analysis, PTSD post-traumatic stress disorder, RCT randomized controlled trial, SMI severe mental illness, SR systematic review, UR umbrella review
Description and summary of associations
Observational studies.
Nine eligible SRs and/or MAs of observational studies assessed 23 associations, evaluated by 122 individual studies from 73 original reports, estimating adverse health outcomes associated with homelessness. Six (26.1%) associations concerned various causes of mortality among PEH, five (21.7%) associations regarded health outcomes related to HIV infection, and four (17.4%) associations inquired about premature geriatric syndromes (e.g., falls, functional limitations). Please refer to Fig. 2 for additional details. Twelve out of 23 (52.2%) associations were nominally statistically significant at a p ≤0.005 level based on the random-effects model, and 7 (30.4%) reached p ≤1×10 −6 . Fifteen associations (65.2%) had large heterogeneity, and the 95% prediction interval excluded the null value for only five associations (21.7%). In twenty associations (86.9%), the effect of the largest study was statistically significant at p ≤0.05. A small-study effect was detected in one association (4.3%), and excess significance bias occurred in one out of ten studies suitable for such estimation (10%). Please refer to Table 2 for details.
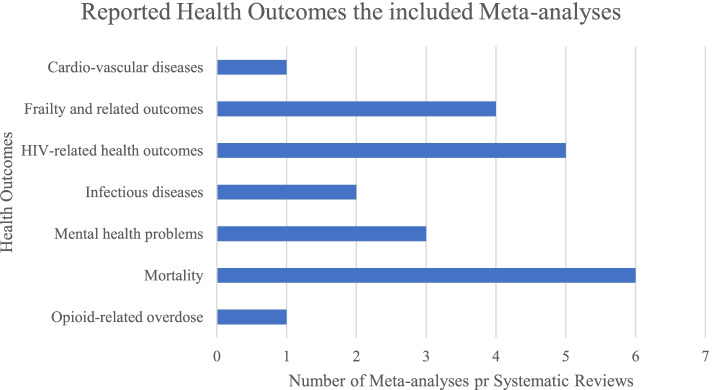
Number of systematic reviews or meta-analyses of observational studies reporting health outcomes among PEH by category of health outcome
Evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome
CE credibility evidence, CI confidence interval, ES effect size, ESB excess significance bias, HR hazard ratio, ICD-10 International Classification of Diseases, 10th revision, LS largest study with significant effect, MA meta-analysis, NA not applicable, NP not pertinent because of fewer than expected number of observed studies, NS not significant, OR odds ratio, PEH people experiencing homelessness, PI prediction interval, RR risk ratio, SMI severe mental illness, SMR standardized mortality ratio, SR systematic review, SSE small study effect, SUD substance use disorder
Intervention studies
One eligible MA of intervention studies documented two therapeutic interventions, evaluated by 10 unique RCTs from 10 original reports, estimating interventions associated with mental health status among PEH [ 220 ]. One association concerned the psychological interventions among PEH diagnosed with depression, while the remaining one dealt with psychological interventions for anxiety. None of the assessed associations reached a statistically significant value at p ≤0.005 based on the random-effects model [ 30 ]. The degree of heterogeneity of the documented associations was quantified in I 2 =42.5% for depression and 39.9% for anxiety. The 95% prediction intervals crossed the null for the outcomes of both interventions. Neither of the largest studies of the two associations was statistically significant at p ≤0.05. Please refer to Table 3 for details.
Evidence from SRs or MAs of intervention studies for the association between different interventions for PEH and any health outcome
CI confidence interval, ES effect size, LS largest study with significant effect, MA meta-analysis, PI prediction interval, RR risk ratio, SMD standardized mean difference, SR systematic review
Grading of systematic reviews and meta-analyses of observational studies
Concerning the SRs and/or MAs of observational studies, none of them concurrently reached a “convincing evidence” threshold, according to the adapted credibility box, and a “high quality” score based on the AMSTAR-2 tool. According to the latter, every SR and/or MA included in the present study was rated as having “critically low” methodological quality. Please refer to Additional file 1 : Table S3 [ 211 – 219 ].
Convincing evidence
Among the 23 associations, two (8.7%) were supported by “convincing evidence”: hospitalization due to any cause among PEH diagnosed with HIV infection and the occurrence of falls within the past year among PEH. Both health outcomes were more common among PEH compared to non-homeless controls.
Highly suggestive evidence
Five (21.7%) associations were rated “highly suggestive evidence”: (1) mortality due to any cause; (2) mortality due to external causes (i.e., intentional injury, unintentional injury, poisoning) among PEH compared to the general population; (3) HCV-infection among PEH using injection drugs compared to those who did not; (4) the presence of limitations in activities of daily living (ADL, e.g., dressing, eating, toileting); and (5) instrumental activities of daily living (IADL, e.g., using telephone, using transportations, taking medications) among PEH compared to non-homeless controls. These above-mentioned health outcomes were more common among PEH compared to their respective controls. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios=6.22 (95% C.I.=4.2–9.2), and SMR=15.75 (95% C.I.=10.58–23.44), respectively.
Suggestive, weak, and no evidence
Five (21.7%) associations were rated “suggestive evidence,” four (17.4%) were “weak evidence,” while “no significant evidence” was found in seven (30.5%) associations.
Grading of systematic reviews and meta-analyses of intervention studies
Concerning intervention studies, the sole MA retrieved obtained a score of “10” at the AMSTAR-plus. Please refer to Table 3 for details.
Sensitivity analysis
A sensitivity analysis limited to high-quality prospective cohort studies included eleven (47.8%) associations, rated according to the NOS. Upon sensitivity analysis, two associations worsen, and one association improved in terms of credibility evidence. Hospitalization due to any cause among PEH with HIV infection shifted from “convincing evidence” to “highly suggestive evidence”, non-adherence to antiretroviral therapy (ART) among PEH with HIV infection shifted from “suggestive evidence” to “weak evidence”, and mortality due to any cause among PEH with SUD up-graded from “no significant evidence” to “highly suggestive evidence”. Please refer to Additional file 1 : Table S4 [ 211 , 214 , 217 , 219 ].
Statement of principal findings
We found convincing evidence that all-cause hospitalization in people with HIV infection and the occurrence of falls within the past year were more common among PEH compared to comparison populations. We also found highly suggestive evidence that mortality due to any cause; mortality due to external causes; hepatitis C infection among PEH using injection drugs; limitations in activities of daily living; and limitations in instrumental activities of daily living were significantly more common in PEH compared to their comparison populations. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios such that PEH had a mortality rate six times their comparison groups and they were about 15 times more likely to die from either accidents or intentional self-harm.
Strengths and limitations
To our knowledge, this study is the first umbrella review that systematically inquired about any health-related outcomes and interventions among PEH, grading the evidence by using previously adopted and widely accepted criteria of credibility [ 14 , 16 , 29 , 31 , 221 ]. All SRs/or MAs of observational studies were graded as having “critically low” methodological quality according to the AMSTAR-2 instrument. Among the associations rated with “highly suggestive evidence”, two were not deemed as “convincing” due to high heterogeneity. Overall, 65.2% of the associations covered by the present umbrella review were hampered by high heterogeneity, which held upon controlling for high-quality prospective studies (seven out of eleven associations—63.6%—had an I 2 >50%).
The differences in definitions of “homelessness” and thus categories of homelessness (for example individuals without permanent housing who may live on the streets; stay in a shelter, mission, single room occupancy facilities, abandoned building or vehicle; or in any other unstable or non-permanent situation) adopted by the authors of the included SRs or MAs could likewise account for the high rates of heterogeneity. Half of the appraised studies lacked a “homelessness” definition, and the remaining half provided a broad definition, as detailed in Table 1 . The timeframe for the homelessness definition, or its related labels, varied across the individual studies included by the appraised SRs or MAs, often merging people who were currently homeless with people who were experiencing this condition within varying timeframes (i.e., 30-day, 6-month, or 12-month intervals, as usually documented by the authors of the original studies). Future research should, therefore, rely on consistent operational definitions, or otherwise stratify their results accordingly, especially considering that substantial variability of the adopted definitions exists across different world regions [ 222 ].
The limitations of this review include the exclusion of RCTs on the impact of housing interventions (Housing First) on PEH. However, such interventions were not deemed eligible for inclusion according to our a priori criteria since we focused on those interventions directly targeting health outcomes in PEH rather than on interventions aimed at reducing the burden of homelessness. Sensitivity analyses were restricted to high-quality prospective studies. Because of the lack of relevant SRs or MAs, we could not appraise otherwise relevant associations between homelessness and health outcomes such as alcohol-related issues, cancer, or infectious diseases other than HIV or HCV. Mental illness-related issues were only accounted for by three comparisons focusing on children experiencing homelessness [ 223 ].
Comparison with previous studies
Considering the two associations reaching “convincing evidence” before sensitivity analysis, the documented hospitalization trend due to any cause in people with HIV is consistent with a recent retrospective cohort study [ 224 ]. A significant increase in “falls during the previous year” may be the result of high rates of concurrent geriatric syndromes, alcohol use disorders, and drug abuse as described elsewhere [ 225 ].
Hence, upstream (e.g., poverty, poor nutrition, barriers to healthcare, and HIV treatment) and downstream factors (i.e., comorbidities and multimorbidity) significantly affect PEH [ 5 ], jeopardize their healthcare, and inflate their hospitalization rates compared to the general population [ 222 ].
Although we were unable to include any SR and MA reporting on the relationship between the COVID-19 pandemic and homelessness, PEH could be at higher risk also at developing hospitalization or fatalities due to COVID-19 according to recent evidence [ 226 ] although this finding deserves replication, providing evidence for the need of well-designed interventions targeting this vulnerable population.
Conclusions and implications for further research
This review adds weight to arguments about why reducing homelessness should be a priority beyond human rights justification. The evidence that experiencing homelessness leads to worse health outcomes is only a secondary consideration for providing affordable housing albeit an important one. Housing reduces hospitalization rates according to RCTs involving PEH with chronic illnesses [ 227 , 228 ]. This study demonstrates that a readily treatable illness such as HIV is not adequately managed in PEH resulting in significant downstream healthcare costs in addition to preventable patient suffering. A recent SR identified that housing PEH (in the short term) improves some aspects of health in this population with HIV, anxiety, and depression [ 229 ].
However, focusing just on providing housing for this population does not mean that an individual’s health needs are automatically solved. We know from Housing First studies that just providing housing does not result in improvements in mental health or addictions after a year, especially in people who have experienced significant trauma [ 55 ]. This umbrella review suggests that the health effects of homelessness are serious, longstanding, and involve all parts of the health system. Finally, while psychological interventions are expected to be more effective than TAU in reducing the burden of the associated health condition among clinical and non-clinical populations [ 230 ], the herein reviewed MA focusing on PEH on the matter [ 220 ] failed to reach a statistically significant threshold according to our conservative p value set at p =.005, though it could not be excluded the condition of homelessness itself could attenuate the effects of such psychological interventions.
What is needed now are studies that look at better coordination of care for this population that may involve hospitals and community partners as well as programs to address health issues in people recently housed after experiencing homelessness. In addition, it should be reiterated that there is an urgent need for international standardization of housing status to improve research rigor that could improve the external generalizability of this field and hence direct policy. Furthermore, more studies should be conducted in low- and middle-income countries as the vast majority of studies to date on this topic have been performed in developed nations. Such bias related to the geographical region may depend on a variety of issues, including, but not necessarily limited to, public health policies as well as the limited funding in LMICs. Lastly, more SRs and MAs with enhanced methodological quality are an unmet need in this field.
Additional file 1: Material 1. adopted search strings. Table S1. criteria for the evaluation of the credibility of the evidence of observational studies. Please note that criterion n.1 (sample size of cases) was purposely waived as outlined in the main-text, methods section. Table S2. List of the 179 excluded records, with the reason(s). Note: duplicate records may appear multiple times for consistency issues. Table S3. Included SRs or MAs of observational studies; quality rating according to the AMSTAR-2. Table S4. Sensitivity analysis of evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome.
Acknowledgments
Abbreviations.
Activities of daily living
Assessment of Multiple Systematic Reviews 2
Assessment of Multiple Systematic Reviews Plus
Antiretroviral therapy
Confidence interval
Coronavirus disease 2019
Effect size
Hepatitis C virus
Human immunodeficiency virus
Instrumental activities of daily living
Low- and middle-income countries
Meta-analysis
Newcastle-Ottawa Scale
People experiencing homelessness
Randomized controlled trial
Standardized mortality ratio
Systematic review
Substance use disorder
Authors’ contributions
MF and AFC conceived the study together with MS. MS and AFC provided input over the study process. MDP, MB, and AM extracted the data, assisting in manuscript drafting under MF guidance. ED performed the analyses. AdB, LS, RC, SH, JGF, ED, and MK provided expert input over the review process and final drafting. The authors read and approved the final manuscript.
Open access funding provided by Linköping University. This study received no funding.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and are available online at https://osf.io/am67d/ and https://osf.io/58mhu/ .
The additional file includes the following: material 1 – [search strings]; table S 1 - [criteria for the evaluation of the credibility of the evidence of observational studies]; table S 2 – [excluded studies with reasons]; table S 3 – [quality rating of the included SRs or MAs of observational studies, according to the AMSTAR-2]; table S 4 – [sensitivity analysis].
Declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Michele Fornaro, Email: dott.fornaro@gmail.com.
Elena Dragioti, Email: elena.dragioti@liu.se.
Michele De Prisco, Email: deprisco.michele@gmail.com.
Martina Billeci, Email: martina.bi@hotmail.it.
Anna Maria Mondin, Email: annamondin90@gmail.com.
Raffaella Calati, Email: raffaella.calati@unimib.it.
Lee Smith, Email: Lee.Smith@aru.ac.uk.
Simon Hatcher, Email: shatcher@toh.ca.
Mark Kaluzienski, Email: mkaluzienski@toh.ca.
Jess G. Fiedorowicz, Email: jess-fiedorowicz@uiowa.edu
Marco Solmi, Email: marco.solmi83@gmail.com.
Andrea de Bartolomeis, Email: adebarto@unina.it.
André F. Carvalho, Email: andrefc7@hotmail.com
- 1. Tsai J. Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health. 2018;40(1):65–74. doi: 10.1093/pubmed/fdx034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Taylor O, Loubiere S, Tinland A, Vargas-Moniz M, Spinnewijn F, Manning R, Gaboardi M, Wolf JR, Bokszczanin A, Bernad R. Lifetime, 5-year and past-year prevalence of homelessness in Europe: a cross-national survey in eight European nations. BMJ Open. 2019;9(11):e033237. doi: 10.1136/bmjopen-2019-033237. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Bensken WP. How do we define homelessness in large health care data? Identifying variation in composition and comorbidities. Health Serv Outcomes Res Methodol. 2021;21(1):145–166. doi: 10.1007/s10742-020-00225-5. [ DOI ] [ Google Scholar ]
- 4. EUROPEAN TYPOLOGY OF HOMELESSNESS AND HOUSING EXCLUSION (ETHOS) [ https://www.feantsa.org/download/ethos2484215748748239888.pdf ]
- 5. Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Prim. 2021;7(1):1–2. doi: 10.1038/s41572-020-00234-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Gilmer C, Buccieri K. Homeless patients associate clinician bias with suboptimal care for mental illness, addictions, and chronic pain. J Prim Care Commun Health. 2020;11:2150132720910289. doi: 10.1177/2150132720910289. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–870. doi: 10.1016/S1473-3099(12)70177-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124. doi: 10.1371/journal.pmed.0020124. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Ojo-Fati O, Joseph AM, Ig-Izevbekhai J, Thomas JL, Everson-Rose SA, Pratt R, Raymond N, Cooney NL, Luo X, Okuyemi KS. Practical issues regarding implementing a randomized clinical trial in a homeless population: strategies and lessons learned. Trials. 2017;18(1):1–10. doi: 10.1186/s13063-017-2046-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Ioannidis JP, Munafo MR, Fusar-Poli P, Nosek BA, David SP. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cognit Sci. 2014;18(5):235–241. doi: 10.1016/j.tics.2014.02.010. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Ioannidis JP. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640–8. 10.1097/EDE.0b013e31818131e7. [ DOI ] [ PubMed ]
- 13. Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Cmaj. 2009;181(8):488–493. doi: 10.1503/cmaj.081086. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: An umbrella review. J Rehabil Med. 2018;50(9):779–791. doi: 10.2340/16501977-2377. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607. [ DOI ] [ PubMed ]
- 16. Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035. 10.1136/bmj.g2035. [ DOI ] [ PMC free article ] [ PubMed ]
- 17. DerSimonian R, Laird N. Meta-analysis in clinical trials. Contr Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14(1):1–12. doi: 10.1186/1471-2288-14-25. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–129. doi: 10.2307/3001666. [ DOI ] [ Google Scholar ]
- 20. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. 10.1136/bmj.d549. [ DOI ] [ PubMed ]
- 22. Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. 10.1136/bmj.d4002. [ DOI ] [ PubMed ]
- 23. Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–253. doi: 10.1177/1740774507079441. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Tsilidis KK, Papatheodorou SI, Evangelou E, Ioannidis JP. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J Natl Cancer Inst. 2012;104(24):1867–1878. doi: 10.1093/jnci/djs437. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Tsilidis KK, Panagiotou OA, Sena ES, Aretouli E, Evangelou E, Howells DW. Salman RA-S, Macleod MR, Ioannidis JP: Evaluation of excess significance bias in animal studies of neurological diseases. PLoS Biol. 2013;11(7):e1001609. doi: 10.1371/journal.pbio.1001609. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatrica Scandinavica. 2017;136(3):236–246. doi: 10.1111/acps.12713. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Ioannidis JP. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. 2013;57(5):184–187. doi: 10.1016/j.jmp.2013.03.002. [ DOI ] [ Google Scholar ]
- 28. Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinson Relat Disord. 2016;23:1–9. doi: 10.1016/j.parkreldis.2015.12.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Bortolato B, Köhler CA, Evangelou E, León-Caballero J, Solmi M, Stubbs B, Belbasis L, Pacchiarotti I, Kessing LV, Berk M. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. 2017;19(2):84–96. doi: 10.1111/bdi.12490. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Koletsi D, Solmi M, Pandis N, Fleming PS, Correll CU, Ioannidis JP. Most recommended medical interventions reach P< 0.005 for their primary outcomes in meta-analyses. Int J Epidemiol. 2020;49(3):885–893. doi: 10.1093/ije/dyz241. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Li X, Meng X, Timofeeva M, Tzoulaki I, Tsilidis KK, Ioannidis JP, Campbell H, Theodoratou E. Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. Bmj. 2017;357:j2376. doi: 10.1136/bmj.j2376. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatr. 2017;74(7):675–684. doi: 10.1001/jamapsychiatry.2017.0624. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. 2017;358:j4008. doi: 10.1136/bmj.j4008. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: 2000.
- 35. Sharmin S, Kypri K, Khanam M, Wadolowski M, Bruno R, Mattick RP. Parental supply of alcohol in childhood and risky drinking in adolescence: systematic review and meta-analysis. Int J Environ Res Public Health. 2017;14(3):287. doi: 10.3390/ijerph14030287. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Ontario HQ. Interventions to Improve Access to Primary Care for People Who Are Homeless: A Systematic Review. Ont Health Technol Assess Ser. 2016;16(9):1–50. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Abad N, Baack B, O'Leary A, Lyles C. A review of HIV/STD behavioral prevention interventions for female sex workers in the United States. Sexual Transmit Dis. 2014;41:S114. doi: 10.1097/OLQ.0000000000000078. [ DOI ] [ Google Scholar ]
- 38. Adams-Guppy JR, Guppy A. A systematic review of interventions for homeless alcohol-abusing adults. Drugs. 2016;23(1):15–30. [ Google Scholar ]
- 39. Alividza V, Mariano V, Ahmad R, Charani E, Rawson TM, Holmes AH, Castro-Sánchez E. Investigating the impact of poverty on colonization and infection with drug-resistant organisms in humans: a systematic review. Infect Dis Poverty. 2018;7(1):76. doi: 10.1186/s40249-018-0459-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Altena AM, Brilleslijper-Kater SN, Wolf JL. Effective interventions for homeless youth: a systematic review. Am J Prev Med. 2010;38(6):637–645. doi: 10.1016/j.amepre.2010.02.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Altena AM, Brilleslijper-Kater SN, Wolf JLM. Effective Interventions for Homeless Youth. A Systematic Review. Am J Prevent Med. 2010;38(6):637–645. doi: 10.1016/j.amepre.2010.02.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Andrade FMR, Figueiredo AS, Capelas ML, Charepe Z, Deodato S. Experiences of homeless families in parenthood: a systematic review and synthesis of qualitative evidence. Int J Environ Res Public Health. 2020;17(8):2712. 10.3390/ijerph17082712. [ DOI ] [ PMC free article ] [ PubMed ]
- 43. Aubry T, Bloch G, Brcic V, Saad A, Magwood O, Abdalla T, Alkhateeb Q, Xie E, Mathew C, Hannigan T, et al. Effectiveness of permanent supportive housing and income assistance interventions for homeless individuals in high-income countries: a systematic review. Lancet Public Health. 2020;5(6):e342–e360. doi: 10.1016/S2468-2667(20)30055-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Auerswald C, Woan J, Lin J. The health status of street children in low-and middle-income countries: A systematic review. Turk Pediatri Arsivi. 2013;48:75. doi: 10.1016/j.jadohealth.2013.03.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Ayano G, Shumet S, Tesfaw G, et al. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20:731. 10.1186/s12889-020-08819-x. [ DOI ] [ PMC free article ] [ PubMed ]
- 46. Ayano G, Belete A, Duko B, Tsegay L, Dachew BA. Systematic review and meta-analysis of the prevalence of depressive symptoms, dysthymia and major depressive disorders among homeless people. BMJ Open. 2021;11(2):e040061. doi: 10.1136/bmjopen-2020-040061. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Ayano G, Shumet S, Tesfaw G, Tsegay L. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20(1):731. doi: 10.1186/s12889-020-08819-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Ayano G, Solomon M, Tsegay L, Yohannes K, Abraha M. A Systematic Review and Meta-Analysis of the Prevalence of Post-Traumatic Stress Disorder among Homeless People. Psychiatr Q. 2020;91(4):949–963. doi: 10.1007/s11126-020-09746-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Ayano G, Tesfaw G, Shumet S. The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):370. doi: 10.1186/s12888-019-2361-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Ayano G, Tsegay L, Abraha M, Yohannes K. Suicidal Ideation and Attempt among Homeless People: a Systematic Review and Meta-Analysis. Psychiatr Q. 2019;90(4):829–842. doi: 10.1007/s11126-019-09667-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Bahji A, Bajaj N. Opioids on trial: a systematic review of interventions for the treatment and prevention of opioid overdose. Can J Addict. 2018;9(1):26–33. doi: 10.1097/CXA.0000000000000013. [ DOI ] [ Google Scholar ]
- 52. Banks S, McHugo GJ, Williams V, Drake RE, Shinn M. A prospective meta-analytic approach in a multisite study of homelessness prevention. New Direct Eval. 2002;2002(94):45–60. doi: 10.1002/ev.50. [ DOI ] [ Google Scholar ]
- 53. Barajas-Nava L. Oral substitution treatment of injecting opioid users for prevention of HIV infection. J Assoc Nurs AIDS Care. 2017;28(5):832–833. doi: 10.1016/j.jana.2017.05.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Batra K, Pharr J, Olawepo JO, Cruz P. Understanding the multidimensional trajectory of psychosocial maternal risk factors causing preterm birth: A systematic review. Asian J Psychiatr. 2020;54:102436. doi: 10.1016/j.ajp.2020.102436. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Baxter AJ, Tweed EJ, Katikireddi SV, Thomson H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health. 2019;73(5):379–387. doi: 10.1136/jech-2018-210981. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, Biello KB. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions. BMC Public Health. 2019;19(1):31. doi: 10.1186/s12889-018-6314-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, Biello KB. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: Evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health. 2019;19(1):1. doi: 10.1186/s12889-018-6314-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Behzadifar M, Gorji HA, Rezapour A, Bragazzi NL. Prevalence of hepatitis C virus among street children in Iran. Infect Dis Poverty. 2018;7(1):88. doi: 10.1186/s40249-018-0469-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 59. Benston EA. Housing Programs for Homeless Individuals With Mental Illness: Effects on Housing and Mental Health Outcomes. Psychiatr Serv. 2015;66(8):806–816. doi: 10.1176/appi.ps.201400294. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2015;105(2):e46–e60. doi: 10.2105/AJPH.2014.302330. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Blanquet M, Legrand A, Pélissier A, Mourgues C. Socio-economics status and metabolic syndrome: A meta-analysis. Diab Metab Syndr. 2019;13(3):1805–1812. doi: 10.1016/j.dsx.2019.04.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Bonner A, Luscombe C. Suicide and homelessness. J Public Mental Health. 2009;8(3):7–19. doi: 10.1108/17465729200900016. [ DOI ] [ Google Scholar ]
- 63. Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, Li LC, Buchbinder R, Ueffing E, Beaton D, et al. Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res (Hoboken) 2011;63(1):39–52. doi: 10.1002/acr.20349. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Brownfield NR, Thielking M, Bates G, Morrison F. Does poverty impact student academic outcomes and wellbeing in australian universities? A systematic review. J Soc Inclusion. 2020;11(2):4–19. [ Google Scholar ]
- 65. Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction. 2011;106(9):1568–1585. doi: 10.1111/j.1360-0443.2011.03467.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Burra TA, Stergiopoulos V, Rourke SB. A systematic review of cognitive deficits in homeless adults: implications for service delivery. Can J Psychiatr. 2009;54(2):123–133. doi: 10.1177/070674370905400210. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Byrne T, Montgomery AE, Dichter ME. Homelessness among female veterans: a systematic review of the literature. Women Health. 2013;53(6):572–596. doi: 10.1080/03630242.2013.817504. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Campos-Matos I, Russo G, Perelman J. Connecting the dots on health inequalities - A systematic review on the social determinants of health in Portugal. Int J Equity Health. 2016;15(1):26. doi: 10.1186/s12939-016-0314-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Carver H, Ring N, Miler J, Parkes T. What constitutes effective problematic substance use treatment from the perspective of people who are homeless? A systematic review and meta-ethnography. Harm Reduct J. 2020;17(1):10. doi: 10.1186/s12954-020-0356-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Cassone A. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Pathog Glob Health. 2012;106(7):377. doi: 10.1179/2047772412Z.00000000086. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Chandler CE, Austin AE, Shanahan ME. Association of Housing Stress With Child Maltreatment: A Systematic Review. Trauma Violence Abuse. 2020;23:639–659. doi: 10.1177/1524838020939136. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Chant C, Smith O, Wang A, Burns K, Dos Santos CC, Friedrich JO, Hwang S. Critical illness in homeless persons: A systematic review of the literature. Intens Care Med. 2013;39:S512. doi: 10.1007/s00134-013-3124-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Chant C, Smith O, Wang A, Hwang S, Friedrich JO, Burns KEA, et al. Homelessness and critical care: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–5. 10.1007/s00134-013-3124-4. [ DOI ] [ PubMed ]
- 74. Chant C, Wang A, Burns KE, dos Santos CC, Hwang SW, Friedrich JO, Smith OM. Critical illness in homeless persons is poorly studied: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–125. doi: 10.1007/s00134-013-3124-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Charron CB, Hayes T, Pakhale S. A systematic review of interventions for smoking tobacco in low socio-economic populations. Am J Respir Crit Care Med. 2018;197. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A6253 .
- 76. Clark NC, Lintzeris N, Gijsbers A, Whelan G, Dunlop A, Ritter A, Ling WW. LAAM maintenance vs methadone maintenance for heroin dependence. Cochrane Database Syst Rev. 2002;2:CD002210. doi: 10.1002/14651858.CD002210. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Coldwell CM, Bender WS. The effectiveness of assertive community treatment for homeless populations with severe mental illness: a meta-analysis. Am J Psychiatry. 2007;164(3):393–399. doi: 10.1176/ajp.2007.164.3.393. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Conn VS, Ruppar TM. Medication adherence outcomes of 771 intervention trials: Systematic review and meta-analysis. Prev Med. 2017;99:269–276. doi: 10.1016/j.ypmed.2017.03.008. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Constance J, Lusher JM. Diabetes management interventions for homeless adults: a systematic review. Int J Public Health. 2020;65(9):1773–1783. doi: 10.1007/s00038-020-01513-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Coren E, Hossain R, Pardo JP, Veras MM, Chakraborty K, Harris H, Martin AJ. Interventions for promoting reintegration and reducing harmful behaviour and lifestyles in street-connected children and young people. Evid Based Child Health. 2013;8(4):1140–1272. doi: 10.1002/ebch.1923. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS Negl Trop Dis. 2015;9(9):e0003898. doi: 10.1371/journal.pntd.0003898. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 82. Coufopoulos A, McDowell G, Roe B, Maden M. Interventions to improve nutrition and nutrition related health amongst homeless mothers and their children: a systematic review. Proceed Nutr Soc. 2012;71(OCE2):E161. 10.1017/S0029665112002182.
- 83. Cumber SN, Tsoka-Gwegweni JM. The Health Profile of Street Children in Africa: A Literature Review. J Public Health Afr. 2015;6(2):566. doi: 10.4081/jphia.2015.566. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Curtis J. Impact of x-ray screening programmes for active tuberculosis in homeless populations: a systematic review of original studies. J Public Health (Oxf) 2016;38(1):106–114. doi: 10.1093/pubmed/fdv014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. da Silva TFC, Lovisi GM, Verdolin LD, Cavalcanti MT. Adherence to drug treatment among schizophrenic spectrum patients: A systematic review of the literature. Jornal Brasileiro de Psiquiatria. 2012;61(4):242–251. doi: 10.1590/S0047-20852012000400008. [ DOI ] [ Google Scholar ]
- 86. Dalton-Locke C, Marston L, McPherson P, Killaspy H. The Effectiveness of Mental Health Rehabilitation Services: A Systematic Review and Narrative Synthesis. Front Psychiatry. 2020;11:607933. doi: 10.3389/fpsyt.2020.607933. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10):e13–e26. doi: 10.2105/AJPH.2013.301491. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. De Vet R, Van Luijtelaar MJA, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JRLM. Effectiveness of case management for homeless persons: A systematic review. Am J Public Health. 2013;103(10):e13–e26. doi: 10.2105/AJPH.2013.301491. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 89. Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, Stone J, Cunningham EB, Trickey A, Dumchev K, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–e1207. doi: 10.1016/S2214-109X(17)30375-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Doran KM, Ragins KT, Gross CP, Zerger S. Medical respite programs for homeless patients: a systematic review. J Health Care Poor Underserved. 2013;24(2):499–524. doi: 10.1353/hpu.2013.0053. [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Dorney-Smith S, Thomson E, Hewett N, Burridge S, Khan Z. Homeless medical respite service provision in the UK. House Care Support. 2019;22(1):40–53. doi: 10.1108/HCS-08-2018-0021. [ DOI ] [ Google Scholar ]
- 92. Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62(5):1353–1363. doi: 10.1002/hep.27978. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 93. El Baba R, Colucci E. Post-traumatic stress disorders, depression, and anxiety in unaccompanied refugee minors exposed to war-related trauma: a systematic review. Int J Cult Mental Health. 2018;11(2):194–207. doi: 10.1080/17542863.2017.1355929. [ DOI ] [ Google Scholar ]
- 94. Embleton L, Mwangi A, Vreeman R, Ayuku D, Braitstein P. The epidemiology of substance use among street children in resource-constrained settings: a systematic review and meta-analysis. Addiction. 2013;108(10):1722–1733. doi: 10.1111/add.12252. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Ennis N, Roy S, Topolovec-Vranic J. Memory impairment among people who are homeless: a systematic review. Memory. 2015;23(5):695–713. doi: 10.1080/09658211.2014.921714. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, Hwang SW. Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health. 2011;11:638. doi: 10.1186/1471-2458-11-638. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Flach Y, Razza TS. Suicidality in homeless children and adolescent: a systematic review. Aggress Violent Behav. 2022;64:101575.
- 98. Folsom D, Jeste DV. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatr Scand. 2002;105(6):404–413. doi: 10.1034/j.1600-0447.2002.02209.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman K. Emergency department interventions for homelessness: a systematic review. Cjem. 2021;23(1):111–122. doi: 10.1007/s43678-020-00008-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman KG. 302 Emergency Department Interventions for Homelessness: A Systematic Review. Ann Emerg Med. 2019;74(4):S119. doi: 10.1016/j.annemergmed.2019.08.261. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Fry CE, Langley K, Shelton KH. A systematic review of cognitive functioning among young people who have experienced homelessness, foster care, or poverty. Child Neuropsychol. 2017;23(8):907–934. doi: 10.1080/09297049.2016.1207758. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Gentry S, Forouhi NG, Notley C. Are Electronic Cigarettes an Effective Aid to Smoking Cessation or Reduction Among Vulnerable Groups? A Systematic Review of Quantitative and Qualitative Evidence. Nicotine Tob Res. 2019;21(5):602–616. doi: 10.1093/ntr/nty054. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 103. Getty CA, Morande A, Lynskey M, Weaver T, Metrebian N. Mobile telephone-delivered contingency management interventions promoting behaviour change in individuals with substance use disorders: a meta-analysis. Addiction. 2019;114(11):1915–1925. doi: 10.1111/add.14725. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Gulati G, Keating N, O'Neill A, Delaunois I, Meagher D, Dunne CP. The prevalence of major mental illness, substance misuse and homelessness in Irish prisoners: systematic review and meta-analyses. Ir J Psychol Med. 2019;36(1):35–45. doi: 10.1017/ipm.2018.15. [ DOI ] [ PubMed ] [ Google Scholar ]
- 105. Hamilton K, Tolfree R, Mytton J. A systematic review of active case-finding strategies for tuberculosis in homeless populations. Int J Tuberc Lung Dis. 2018;22(10):1135–1144. doi: 10.5588/ijtld.17.0784. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Hamilton K, Tolfree R, Mytton J. Impact and implementation of active case finding for tuberculosis in homeless populations: a systematic review. Lancet. 2019;394:S48. doi: 10.1016/S0140-6736(19)32845-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Hanlon P, Yeoman L, Gibson L, Esiovwa R, Williamson AE, Mair FS, Lowrie R. A systematic review of interventions by healthcare professionals to improve management of non-communicable diseases and communicable diseases requiring long-term care in adults who are homeless. BMJ Open. 2018;8(4):e020161. doi: 10.1136/bmjopen-2017-020161. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 108. Heerde JA, Hemphill SA. A systematic review of associations between perpetration of physically violent behaviors and property offenses, victimization and use of substances among homeless youth. Children Youth Serv Rev. 2014;44:265–277. doi: 10.1016/j.childyouth.2014.06.020. [ DOI ] [ Google Scholar ]
- 109. Heerde JA, Hemphill SA. Is Substance Use Associated with Perpetration and Victimization of Physically Violent Behavior and Property Offences Among Homeless Youth? A Systematic Review of International Studies. Child Youth Care Forum. 2015;44(2):277–307. doi: 10.1007/s10566-014-9282-x. [ DOI ] [ Google Scholar ]
- 110. Heerde JA, Hemphill SA. The role of risk and protective factors in the modification of risk for sexual victimization, sexual risk behaviors, and survival sex among homeless youth: A meta-analysis. J Investig Psychol Offend Profil. 2017;14(2):150–174. doi: 10.1002/jip.1473. [ DOI ] [ Google Scholar ]
- 111. Heerde JA, Hemphill SA. Associations between individual-level characteristics and exposure to physically violent behavior among young people experiencing homelessness: A meta-analysis. Aggress Violent Behav. 2019;47:46–57. doi: 10.1016/j.avb.2019.03.002. [ DOI ] [ Google Scholar ]
- 112. Heerde JA, Scholes-Balog KE, Hemphill SA. Associations between youth homelessness, sexual offenses, sexual victimization, and sexual risk behaviors: a systematic literature review. Arch Sex Behav. 2015;44(1):181–212. doi: 10.1007/s10508-014-0375-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 113. Herrman H. Mental disorders among homeless people in western countries. PLoS Med. 2008;5(12):e237. doi: 10.1371/journal.pmed.0050237. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 114. Heuvelings CC, de Vries SG, Greve PF, Visser BJ, Bélard S, Janssen S, Cremers AL, Spijker R, Shaw B, Hill RA, et al. Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis. 2017;17(5):e144–e158. doi: 10.1016/S1473-3099(16)30532-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. Heuvelings CC, Greve PF, de Vries SG, Visser BJ, Bélard S, Janssen S, Cremers AL, Spijker R, Shaw E, Hill RA, et al. Effectiveness of service models and organisational structures supporting tuberculosis identification and management in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. BMJ Open. 2018;8(9):e019642. doi: 10.1136/bmjopen-2017-019642. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 116. Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo T, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Rev Esc Enferm USP. 2021;55:e03688. doi: 10.1590/s1980-220x2019039603688. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo TMRM, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Revista da Escola de Enfermagem da U S P. 2021;55:e03688. doi: 10.1590/s1980-220x2019039603688. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. Hodgson KJ, Shelton KH, van den Bree MB, Los FJ. Psychopathology in young people experiencing homelessness: a systematic review. Am J Public Health. 2013;103(6):e24–e37. doi: 10.2105/AJPH.2013.301318. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 119. Hodgson KJ, Shelton KH, Van Den Bree MBM, Los FJ. Psychopathology in young people experiencing homelessness: A systematic review. Am J Public Health. 2013;103(6):e24–e37. doi: 10.2105/AJPH.2013.301318. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. Hoell A, Franz M, Salize HJ. Healthcare for homeless people with mental illness-A review of results of current interventions. Psychiatrie. 2017;14(2):75–85. [ Google Scholar ]
- 121. Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481–498. doi: 10.1111/sltb.12369. [ DOI ] [ PubMed ] [ Google Scholar ]
- 122. Hossain MM, Purohit N, Sultana A, Ma P, McKyer ELJ, Ahmed HU. Prevalence of mental disorders in South Asia: An umbrella review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020;51:102041. doi: 10.1016/j.ajp.2020.102041. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med. 2005;29(4):311–319. doi: 10.1016/j.amepre.2005.06.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Ijaz S, Jackson J, Thorley H, Porter K, Fleming C, Richards A, Bonner A, Savović J. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71. doi: 10.1186/s12939-017-0564-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 125. Ijaz S, Thorley H, Porter K, Fleming C, Jones T, Kesten J, Mamluk L, Richards A, Marques EMR, Savović J. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8. doi: 10.1186/s12939-018-0722-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2:e1229. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 127. Kenworthy J, Ayyub R, Rtveladze K, Wright D, Xia A, Fordham R. A systematic literature review of the societal costs and consequences of heroin addiction. Value Health. 2017;20(9):A497. doi: 10.1016/j.jval.2017.08.560. [ DOI ] [ Google Scholar ]
- 128. Klop HT, de Veer AJE, van Dongen SI, Francke AL, Rietjens JAC, Onwuteaka-Philipsen BD. Palliative care for homeless people: a systematic review of the concerns, care needs and preferences, and the barriers and facilitators for providing palliative care. BMC Palliat Care. 2018;17(1):67. doi: 10.1186/s12904-018-0320-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 129. Krahn J, Caine V, Chaw-Kant J, Singh AE. Housing interventions for homeless, pregnant/parenting women with addictions: a systematic review. J Soc Distress Homeless. 2018;27(1):75–88. doi: 10.1080/10530789.2018.1442186. [ DOI ] [ Google Scholar ]
- 130. Kyle T, Dunn JR. Effects of housing circumstances on health, quality of life and healthcare use for people with severe mental illness: a review. Health Soc Care Community. 2008;16(1):1–15. doi: 10.1111/j.1365-2524.2007.00723.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 131. Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 132. Leibler JH, Zakhour CM, Gadhoke P, Gaeta JM. Zoonotic and Vector-Borne Infections Among Urban Homeless and Marginalized People in the United States and Europe, 1990-2014. Vector Borne Zoonotic Dis. 2016;16(7):435–444. doi: 10.1089/vbz.2015.1863. [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Lowrie R, Stock K, Lucey S, Knapp M, Williamson A, Montgomery M, Lombard C, Maguire D, Allan R, Blair R, et al. Pharmacist led homeless outreach engagement and non-medical independent prescribing (Rx) (PHOENIx) intervention for people experiencing homelessness: a non- randomised feasibility study. Int J Equity Health. 2021;20(1):19. doi: 10.1186/s12939-020-01337-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 134. Luong CT, Rew L, Banner M. Suicidality in Young Men Who Have Sex with Men: A Systematic Review of the Literature. Issues Ment Health Nurs. 2018;39(1):37–45. doi: 10.1080/01612840.2017.1390020. [ DOI ] [ PubMed ] [ Google Scholar ]
- 135. Ly A, Latimer E. Housing First Impact on Costs and Associated Cost Offsets: A Review of the Literature. Can J Psychiatry. 2015;60(11):475–487. doi: 10.1177/070674371506001103. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 136. Ly TDA, Castaneda S, Hoang VT, Dao TL, Gautret P. Vaccine-preventable diseases other than tuberculosis, and homelessness: A scoping review of the published literature, 1980 to 2020. Vaccine. 2021;39(8):1205–1224. doi: 10.1016/j.vaccine.2021.01.035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Maglione MA, Raaen L, Chen C, Azhar G, Shahidinia N, Shen M, Maksabedian E, Shanman RM, Newberry S, Hempel S. Effects of medication assisted treatment (MAT) for opioid use disorder on functional outcomes: a systematic review. J Subst Abuse Treatment. 2018;89:28–51. doi: 10.1016/j.jsat.2018.03.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Magwood O, Salvalaggio G, Beder M, Kendall C, Kpade V, Daghmach W, Habonimana G, Marshall Z, Snyder E, O'Shea T, et al. The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLoS One. 2020;15(1):e0227298. doi: 10.1371/journal.pone.0227298. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 139. Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, Pinto R, Rhodes S, Moya E, Chavez-Baray S. Evaluating the Impact of Immigration Policies on Health Status Among Undocumented Immigrants: A Systematic Review. J Immigrant Minor Health. 2015;17(3):947–970. doi: 10.1007/s10903-013-9968-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 140. Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209. doi: 10.1002/14651858.CD002209.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 141. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2:CD002207. doi: 10.1002/14651858.CD002207.pub4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 142. McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons' access to and use of information technologies. Am J Public Health. 2013;103(Suppl 2):e11–e24. doi: 10.2105/AJPH.2013.301623. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 143. McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry. 2018;18(1):128. doi: 10.1186/s12888-018-1725-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 144. Mendes KT, Ronzani TM, de Paiva FS. Homeless population, vulnerabilities and drugs: a systematic review. Psicol Soc. 2019;31:e169056. 10.1590/1807-0310/2019v31169056.
- 145. Moe J, Kirkland SW, Rawe E, Ospina MB, Vandermeer B, Campbell S, Rowe BH. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Acad Emerg Med. 2017;24(1):40–52. doi: 10.1111/acem.13060. [ DOI ] [ PubMed ] [ Google Scholar ]
- 146. Momsen AM, Rasmussen JO, Nielsen CV, Iversen MD, Lund H. Multidisciplinary team care in rehabilitation: An overview of reviews. J Rehabil Med. 2012;44(11):901–912. doi: 10.2340/16501977-1040. [ DOI ] [ PubMed ] [ Google Scholar ]
- 147. Moniruzzaman A, Kazanjian A, Wong H, Chowdhury MM, Elwood RK, Fitzgerald JM. A systematic review on risk factors of mortality among Tb patients. Am J Respir Crit Care Med. 2010;181. 10.1164/ajrccm-conference.2010.181.1_MeetingAbstracts.A5460.
- 148. Morton MH, Kugley S, Epstein R, Farrell A. Interventions for youth homelessness: A systematic review of effectiveness studies. Child Youth Serv Rev. 2020;116:105096. doi: 10.1016/j.childyouth.2020.105096. [ DOI ] [ Google Scholar ]
- 149. Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf) 2009;31(2):258–277. doi: 10.1093/pubmed/fdp008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 150. Muzzey FK, Fortenberry JD, Maas MK, Holtrop K, McCauley H. 169. Sexual and Gender Minority Homeless Youth and Their Sexual Relationships: A Systematic Review of Recent Literature. J Adolesc Health. 2020;66(2):S86. doi: 10.1016/j.jadohealth.2019.11.172. [ DOI ] [ Google Scholar ]
- 151. Nevard I, Green C, Bell V, Gellatly J, Brooks H, Bee P. Conceptualising the social networks of vulnerable children and young people: a systematic review and narrative synthesis. Soc Psychiatry Psychiatr Epidemiol. 2021;56(2):169–182. doi: 10.1007/s00127-020-01968-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 152. Nilsson S, Nordentoft M, Hjorthoj C. Psychiatric predictors for becoming homeless and exiting homelessness: A systematic review and meta-analysis. Schizophrenia Bull. 2020;46:S278. doi: 10.1093/schbul/sbaa029.686. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 153. Noh D. Psychological Interventions for Runaway and Homeless Youth. J Nurs Scholar. 2018;50(5):465–472. doi: 10.1111/jnu.12402. [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Omerov P, Craftman Å, Mattsson E, Klarare A. Homeless persons' experiences of health- and social care: A systematic integrative review. Health Soc Care Community. 2020;28(1):1–11. doi: 10.1111/hsc.12857. [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Paisi M, March-McDonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: a systematic review. BMJ Sex Reprod Health. 2020;47:211–220. doi: 10.1136/bmjsrh-2020-200799. [ DOI ] [ PubMed ] [ Google Scholar ]
- 156. Paisi MD, March-Mcdonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: A systematic review. BMJ Sex Reprod Health. 2020;47:211–220. doi: 10.1136/bmjsrh-2020-200799. [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Paquette K, Cheng MP, Kadatz MJ, Cook VJ, Chen W, Johnston JC. Chest radiography for active tuberculosis case finding in the homeless: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2014;18(10):1231–1236. doi: 10.5588/ijtld.14.0105. [ DOI ] [ PubMed ] [ Google Scholar ]
- 158. Parks RW, Stevens RJ, Spence SA. A systematic review of cognition in homeless children and adolescents. J R Soc Med. 2007;100(1):46–50. doi: 10.1177/014107680710000116. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 159. Parriott A, Malekinejad M, Miller AP, Marks SM, Horvath H, Kahn JG. Care Cascade for targeted tuberculosis testing and linkage to Care in Homeless Populations in the United States: a meta-analysis. BMC Public Health. 2018;18(1):485. doi: 10.1186/s12889-018-5393-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 160. Peng Y, Hahn RA, Finnie RKC, Cobb J, Williams SP, Fielding JE, Johnson RL, Montgomery AE, Schwartz AF, Muntaner C, et al. Permanent Supportive Housing With Housing First to Reduce Homelessness and Promote Health Among Homeless Populations With Disability: A Community Guide Systematic Review. J Public Health Manag Pract. 2020;26(5):404–411. doi: 10.1097/PHH.0000000000001219. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 161. Polcin DL. Co-occurring substance abuse and mental health problems among homeless persons: Suggestions for research and practice. J Soc Distress Homeless. 2016;26(1):1–10. doi: 10.1179/1573658X15Y.0000000004. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 162. Polillo A, Gran-Ruaz S, Sylvestre J, Kerman N. The use of eHealth interventions among persons experiencing homelessness: A systematic review. Digit Health. 2021;7:2055207620987066. doi: 10.1177/2055207620987066. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 163. Ponka D, Agbata E, Kendall C, Stergiopoulos V, Mendonca O, Magwood O, Saad A, Larson B, Sun AH, Arya N, et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: A systematic review. PLoS One. 2020;15(4):e0230896. doi: 10.1371/journal.pone.0230896. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 164. Rajendran M, Zaki RA, Aghamohammadi N. Contributing risk factors towards the prevalence of multidrug-resistant tuberculosis in Malaysia: A systematic review. Tuberculosis (Edinb) 2020;122:101925. doi: 10.1016/j.tube.2020.101925. [ DOI ] [ PubMed ] [ Google Scholar ]
- 165. Rezaei O, Ghiasvand H, Higgs P, Noroozi A, Noroozi M, Rezaei F, Armoon B, Bayani A. Factors associated with injecting-related risk behaviors among people who inject drugs: a systematic review and meta-analysis study. J Addict Dis. 2020;38(4):420–437. doi: 10.1080/10550887.2020.1781346. [ DOI ] [ PubMed ] [ Google Scholar ]
- 166. Richter D, Hoffmann H. Independent housing and support for people with severe mental illness: systematic review. Acta Psychiatr Scand. 2017;136(3):269–279. doi: 10.1111/acps.12765. [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. Riquelme-Miralles D, Palazón-Bru A, Sepehri A, Gil-Guillén VF. A systematic review of non-pharmacological interventions to improve therapeutic adherence in tuberculosis. Heart Lung. 2019;48(5):452–461. doi: 10.1016/j.hrtlng.2019.05.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 168. Roy L. Criminal behavior and victimization among homeless individuals with severe mental illness: A systematic review (Psychiatric Services (2014)) Psychiatr Serv. 2014;65(7):896. doi: 10.1176/appi.ps.657erratum. [ DOI ] [ PubMed ] [ Google Scholar ]
- 169. Roy L, Crocker AG, Nicholls TL, Latimer EA, Ayllon AR. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr Serv. 2014;65(6):739–750. doi: 10.1176/appi.ps.201200515. [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Sandgren A, Vonk Noordegraaf-Schouten M, van Kessel F, Stuurman A, Oordt-Speets A, van der Werf MJ. Initiation and completion rates for latent tuberculosis infection treatment: a systematic review. BMC Infect Dis. 2016;16:204. doi: 10.1186/s12879-016-1550-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 171. Saulle R, Vecchi S, Gowing L. Supervised dosing with a long-acting opioid medication in the management of opioid dependence. Cochrane Database Syst Rev. 2017;4:CD011983. doi: 10.1002/14651858.CD011983.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 172. Sayal AP, Slomovic J, Bhambra NS, Popovic MM, Lichter M. Visual impairment and the prevalence of ocular pathology in homeless children and adults globally: a systematic review. Can J Ophthalmol. 2020;56:158–165. doi: 10.1016/j.jcjo.2020.09.023. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Scappaticci ALSS, Blay SL. Homeless adolescent mothers: A systematic review of the literature. Revista de Psiquiatria do Rio Grande do Sul. 2010;32(1):3–15. doi: 10.1590/S0101-81082010000100002. [ DOI ] [ Google Scholar ]
- 174. Schneider JA, Skaathun B, Michaels S, Young L, Green K, Morgan E, Coombs RW, Friedman S, Laumann E. Drivers of HIV treatment success among a population-based sample of younger black MSM. Top Antiviral Med. 2015;23:494–495. [ Google Scholar ]
- 175. Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, Gutwinski S. The Prevalence of Mental Illness in Homeless People in Germany. Dtsch Arztebl Int. 2017;114(40):665–672. doi: 10.3238/arztebl.2017.0665. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 176. Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, Gutwinski S. The prevalence of mental illness in homeless people in Germany - A systematic review and meta-analysis. Deutsches Arzteblatt Int. 2017;114(40):665–672. doi: 10.3238/arztebl.2017.0665. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 177. Schumacher JE, Milby JB, Wallace D, Meehan DC, Kertesz S, Vuchinich R, Dunning J, Usdan S. Meta-analysis of day treatment and contingency-management dismantling research: Birmingham Homeless Cocaine Studies (1990-2006) J Consult Clin Psychol. 2007;75(5):823–828. doi: 10.1037/0022-006X.75.5.823. [ DOI ] [ PubMed ] [ Google Scholar ]
- 178. Shortt SE, Hwang S, Stuart H, Bedore M, Zurba N, Darling M. Delivering primary care to homeless persons: a policy analysis approach to evaluating the options. Healthc Policy. 2008;4(1):108–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 179. Silva EN, da Silva Pereira ACE, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Revista Panamericana de Salud Publica/Pan Am J Public Health. 2018;42:e40. doi: 10.26633/RPSP.2018.40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 180. Silva EN, Pereira A, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Rev Panam Salud Publica. 2018;42:e40. doi: 10.26633/RPSP.2018.114. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 181. Simmonds M, Simmonds K, Weleff J. Prevalence and problems of pain in the homeless: A systematic review. J Pain. 2016;17(4):S12–S13. doi: 10.1016/j.jpain.2016.01.050. [ DOI ] [ Google Scholar ]
- 182. Simoens S, Matheson C, Bond C, Inkster K, Ludbrook A. The effectiveness of community maintenance with methadone or buprenorphine for treating opiate dependence. Br J Gen Pract. 2005;55(511):139–146. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 183. Soar K, Dawkins L, Robson D, Cox S. Smoking amongst adults experiencing homelessness: A systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. J Smok Cessation. 2020;15:94–108. doi: 10.1017/jsc.2020.11. [ DOI ] [ Google Scholar ]
- 184. Speirs V, Johnson M, Jirojwong S. A systematic review of interventions for homeless women. J Clin Nurs. 2013;22(7-8):1080–1093. doi: 10.1111/jocn.12056. [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Spence S, Stevens R, Parks R. Cognitive dysfunction in homeless adults: a systematic review. J R Soc Med. 2004;97(8):375–379. doi: 10.1177/014107680409700804. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 186. Strang J, Groshkova T, Uchtenhagen A, Van Den Brink W, Haasen C, Schechter MT, Lintzeris N, Bell J, Pirona A, Oviedo-Joekes E. Heroin on trial: systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addiction. Br J Psychiatr. 2015;207(1):5–14. doi: 10.1192/bjp.bp.114.149195. [ DOI ] [ PubMed ] [ Google Scholar ]
- 187. Stubbs JL, Thornton AE, Sevick JM, Silverberg ND, Barr AM, Honer WG, Panenka WJ. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5(1):e19–e32. doi: 10.1016/S2468-2667(19)30188-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 188. Sudarsanam TD, Tharyan P. Rifampicin compared to isoniazid for preventing active TB in HIV-negative people at risk of developing active TB: Implications for public health. Clin Epidemiol Global Health. 2014;2(1):28–36. doi: 10.1016/j.cegh.2013.11.003. [ DOI ] [ Google Scholar ]
- 189. Sumalinog R, Harrington K, Dosani N, Hwang SW. Advance care planning, palliative care, and end-of-life care interventions for homeless people: A systematic review. Palliat Med. 2017;31(2):109–119. doi: 10.1177/0269216316649334. [ DOI ] [ PubMed ] [ Google Scholar ]
- 190. Sundin EC. Homelessness and experiences of psychological trauma in the western world: A research review and a qualitative study. Eur Psychiatry. 2011;26:1811. doi: 10.1016/S0924-9338(11)73515-5. [ DOI ] [ Google Scholar ]
- 191. Tankimovich M. Barriers to and interventions for improved tuberculosis detection and treatment among homeless and immigrant populations: a literature review. J Community Health Nurs. 2013;30(2):83–95. doi: 10.1080/07370016.2013.778723. [ DOI ] [ PubMed ] [ Google Scholar ]
- 192. Thomas CP, Fullerton CA, Kim M, Montejano L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME. Medication-assisted treatment with buprenorphine: assessing the evidence. Psychiatric Serv. 2014;65(2):158–170. doi: 10.1176/appi.ps.201300256. [ DOI ] [ PubMed ] [ Google Scholar ]
- 193. Thomas Y, Gray M, McGinty S. A systematic review of occupational therapy interventions with homeless people. Occup Ther Health Care. 2011;25(1):38–53. doi: 10.3109/07380577.2010.528554. [ DOI ] [ PubMed ] [ Google Scholar ]
- 194. Thorley H, Porter K, Fleming C, Jones T, Kesten J, Marques E, Richards A, Savović J. Interventions for preventing or treating malnutrition in problem drinkers who are homeless or vulnerably housed: protocol for a systematic review. Syst Rev. 2015;4:131. doi: 10.1186/s13643-015-0114-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 195. To MJ, Brothers TD, Van Zoost C. Foot Conditions among Homeless Persons: A Systematic Review. PLoS One. 2016;11(12):e0167463. doi: 10.1371/journal.pone.0167463. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 196. Topolovec-Vranic J, Ennis N, Colantonio A, Cusimano MD, Hwang SW, Kontos P, Ouchterlony D, Stergiopoulos V. Traumatic brain injury among people who are homeless: a systematic review. BMC Public Health. 2012;12:1059. doi: 10.1186/1471-2458-12-1059. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 197. Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177–195. doi: 10.1093/epirev/mxu004. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 198. Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. doi: 10.1136/bmjopen-2014-006414. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 199. Vijayaraghavan M, Elser H, Frazer K, Lindson N, Apollonio D. Interventions to reduce tobacco use in people experiencing homelessness. Cochrane Database Syst Rev. 2020;12:CD013413. doi: 10.1002/14651858.CD013413.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 200. Wang JZ, Mott S, Magwood O, Mathew C, McLellan A, Kpade V, Gaba P, Kozloff N, Pottie K, Andermann A. The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: a systematic review. BMC Public Health. 2019;19(1):1528. doi: 10.1186/s12889-019-7856-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 201. Weber JJ. A systematic review of nurse-led interventions with populations experiencing homelessness. Public Health Nurs. 2019;36(1):96–106. doi: 10.1111/phn.12552. [ DOI ] [ PubMed ] [ Google Scholar ]
- 202. White BM, Newman SD. Access to primary care services among the homeless: a synthesis of the literature using the equity of access to medical care framework. J Prim Care Community Health. 2015;6(2):77–87. doi: 10.1177/2150131914556122. [ DOI ] [ PubMed ] [ Google Scholar ]
- 203. Whitney B, Kruszka B, Lorvick J, Lucas GM, Wechsberg W, Kuo I, Cunningham WE, Clemenzi-Allen A, Franks J, Crane HM. Association between housing stability and new HIV diagnosis in seek and test studies. Topics Antiviral Med. 2017;25(1):362s–363s. [ Google Scholar ]
- 204. Wilson MG, Aidala A, Gogolishvili D, Shubert V, Rueda S, Bozack A, Chambers LA, Caban M, Rourke SB. Housing status and the health of people living with HIV/AIDS: A systematic review. Can J Infect Dis Med Microbiol. 2012;23:40A–41A. [ Google Scholar ]
- 205. Woan J, Lin J, Auerswald C. The health status of street children and youth in low- and middle-income countries: a systematic review of the literature. J Adolesc Health. 2013;53(3):314–321.e312. doi: 10.1016/j.jadohealth.2013.03.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. Wright N, Walker J. Homelessness and drug use - A narrative systematic review of interventions to promote sexual health. AIDS Care Psycholog Socio Med Aspects AIDS/HIV. 2006;18(5):467–478. doi: 10.1080/09540120500220474. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Wright NM, Walker J. Homelessness and drug use - a narrative systematic review of interventions to promote sexual health. AIDS Care. 2006;18(5):467–478. doi: 10.1080/09540120500220474. [ DOI ] [ PubMed ] [ Google Scholar ]
- 208. Xiang J, Kaminga AC, Wu XY, Lai Z, Yang J, Lian Y, Wang X, Wen SW, Liu A, Dai W. Lifetime prevalence of suicidal attempt among homeless individuals in North America: a meta-analysis. J Affect Disord. 2021;287:341–349. doi: 10.1016/j.jad.2021.03.052. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Yadee J, Bangpan M, Thavorn K, Welch V, Tugwell P, Chaiyakunapruk N. Assessing evidence of interventions addressing inequity among migrant populations: A two-stage systematic review. Int J Equity Health. 2019;18(1):64. doi: 10.1186/s12939-019-0970-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 210. Zlotnick C, Tam T, Zerger S. Common needs but divergent interventions for U.S. homeless and foster care children: results from a systematic review. Health Soc Care Community. 2012;20(5):449–476. doi: 10.1111/j.1365-2524.2011.01053.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 211. Tweed EJ, Thomson RM, Lewer D, Sumpter C, Kirolos A, Southworth PM, Purba AK, Aldridge RW, Hayward A, Story A, et al. Health of people experiencing co-occurring homelessness, imprisonment, substance use, sex work and/or severe mental illness in high-income countries: a systematic review and meta-analysis. J Epidemiol Community Health. 2021;75:1010–1018. doi: 10.1136/jech-2020-215975. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 212. Arum C, Fraser H, Artenie AA, Bivegete S, Trickey A, Alary M, Astemborski J, Iversen J, Lim AG, MacGregor L, et al. Homelessness, unstable housing, and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis. Lancet Public Health. 2021;6:e309–e323. doi: 10.1016/S2468-2667(21)00013-X. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 213. Suh K, Beck J, Katzman W, Allen DD. Homelessness and rates of physical dysfunctions characteristic of premature geriatric syndromes: systematic review and meta-analysis. Physiother Theory Pract. 2020;38:1–10. doi: 10.1080/09593985.2020.1809045. [ DOI ] [ PubMed ] [ Google Scholar ]
- 214. Al-Shakarchi NJ, Evans H, Luchenski SA, Story A, Banerjee A. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. 2020;106(19):1483–1488. doi: 10.1136/heartjnl-2020-316706. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 215. van Draanen J, Tsang C, Mitra S, Karamouzian M, Richardson L. Socioeconomic marginalization and opioid-related overdose: A systematic review. Drug Alcohol Depend. 2020;214:108127. doi: 10.1016/j.drugalcdep.2020.108127. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 216. Lin D, Zhang CY, He ZK, Zhao XD. How does hard-to-reach status affect antiretroviral therapy adherence in the HIV-infected population? Results from a meta-analysis of observational studies. BMC Public Health. 2019;19(1):789. doi: 10.1186/s12889-019-7135-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 217. Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, Tweed EJ, Lewer D, Vittal Katikireddi S, Hayward AC. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391(10117):241–250. doi: 10.1016/S0140-6736(17)31869-X. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 218. Bassuk EL, Richard MK, Tsertsvadze A. The prevalence of mental illness in homeless children: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54(2):86–96.e82. doi: 10.1016/j.jaac.2014.11.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 219. Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, Bozack AK, Caban M, Rourke SB. Housing Status, Medical Care, and Health Outcomes Among People Living With HIV/AIDS: A Systematic Review. Am J Public Health. 2016;106(1):e1–e23. doi: 10.2105/AJPH.2015.302905. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 220. Hyun M, Bae SH, Noh D. Systematic review and meta-analyses of randomized control trials of the effectiveness of psychosocial interventions for homeless adults. J Adv Nurs. 2020;76(3):773–786. doi: 10.1111/jan.14275. [ DOI ] [ PubMed ] [ Google Scholar ]
- 221. Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, Stubbs B, Firth J, Fornaro M, Tsartsalis D. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76(12):1241–1255. doi: 10.1001/jamapsychiatry.2019.2859. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 222. Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 223. Smartt C, Prince M, Frissa S, Eaton J, Fekadu A, Hanlon C. Homelessness and severe mental illness in low-and middle-income countries: scoping review. BJPsych Open. 2019;5(4):e57. doi: 10.1192/bjo.2019.32. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 224. Clemenzi-Allen A, Neuhaus J, Geng E, Sachdev D, Buchbinder S, Havlir D, et al. Housing instability results in increased acute care utilization in an urban HIV clinic cohort. In: Open forum infectious diseases: Oxford University Press US; 2019. p. ofz148. [ DOI ] [ PMC free article ] [ PubMed ]
- 225. Brown RT, Kiely DK, Bharel M, Mitchell SL. Factors associated with geriatric syndromes in older homeless adults. J Health Care Poor Underserved. 2013;24:456–468. doi: 10.1353/hpu.2013.0077. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 226. Culhane D, Treglia D, Steif K, Kuhn R, Byrne T. Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality. 2020. https://endhomelessness.org/wp-content/uploads/2020/03/COVID-paper_clean-636pm.pdf .
- 227. Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(S3):S675–S680. doi: 10.2105/AJPH.2008.137810. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 228. Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. Jama. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [ DOI ] [ PubMed ] [ Google Scholar ]
- 229. Onapa H, Sharpley CF, Bitsika V, McMillan ME, MacLure K, Smith L, Agnew LL. The physical and mental health effects of housing homeless people: A systematic review. Health Soc Care Community. 2021;30:448–468. doi: 10.1111/hsc.13486. [ DOI ] [ PubMed ] [ Google Scholar ]
- 230. van Agteren J, Iasiello M, Lo L, Bartholomaeus J, Kopsaftis Z, Carey M, Kyrios M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat Human Behav. 2021;5(5):631–652. doi: 10.1038/s41562-021-01093-w. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (1.1 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
2024 AHAR: Part 1 - PIT Estimates of Homelessness in the U.S.
Posted Date: December 2024
Description
This report outlines the key findings of the Point-In-Time (PIT) count and Housing Inventory Count (HIC) conducted in January 2024. Specifically, this report provides 2024 national, state, and CoC-level PIT and HIC estimates of homelessness, as well as estimates of chronically homeless persons, homeless veterans, and homeless children and youth.
Keywords: 2024 PIT; 2024 HIC; 2024 Point-in-Time count; Annual Homelessness Assessment Report to Congress
To view all AHARs since 2007, visit the AHAR page .
Resource Links
- 2024 AHAR Report: Part 1 - PIT Estimates of Homelessness (PDF)
- 2007 - 2024 Point-in-Time Estimates by CoC (XLSB)
- 2007 - 2024 Point-in-Time Estimates by State (XLSB)
- 2007 - 2024 Housing Inventory Count by CoC (XLSX)
- 2007 - 2024 Housing Inventory Count by State (XLSX)
- 2011 - 2024 PIT Veteran Counts by CoC (XLSX)
- 2011 - 2024 PIT Veteran Counts by State (XLSX)
- 2024 Housing Inventory Count (Raw File) (CSV)
- Research, Evaluation, and Best Practices
- HUD Approved

IMAGES
COMMENTS
We address many of these issues in the context of public health and explore the public health implications and potential solutions to homelessness, focusing on contemporary and emerging research and innovative strategies, and highlighting best practices to address homelessness among key populations.
In this overview, we highlight structural and individual risk factors that can lead to homelessness, explore evidence on the relationship between homelessness and health, discuss programmatic and...
A Research Agenda for Ending Homelessness. This document is intended to inform government agencies, philanthropic organizations, and other funders about outstanding research questions on homeless populations and subpopulations and interventions designed to end homelessness.
Homelessness in the United States is an urgent public health issue and humanitarian crisis. It impacts cities, suburbs, and rural towns in every state. Housing is a social determinant of health, meaning lack of it has a negative impact on overall health and life expectancy.
Jan 20, 2022 · HHS funds the development of research projects to aid providers and policymakers in addressing the issues facing people experiencing homelessness.
Aug 22, 2017 · This study aims to examine the stories of homeless people to gain understanding of the social conditions under which homelessness occurs, in order to propose a theoretical explanation for it. Twenty-six semi-structured interviews were conducted with homeless people in three centres for homeless people in Cheshire North West of England.
federal investments in homelessness research and offer a roadmap for academic researchers, philanthropy, students, and others committed to advancing the most effective responses to homelessness in the United States.
Dec 8, 2017 · The Center for Evidence-based Solutions to Homelessness is a new resource dedicated to synthesizing and explaining the key research insights needed to end homelessness. The Alliance partnered with Abt Associates to build the Evidence Base, a collection of research
Homelessness has been associated with multiple detrimental health outcomes across observational studies. However, relatively few randomized controlled trials (RCTs) have been conducted on people who experience homelessness (PEH).
Learning Agenda & Research Roadmap. Ongoing Research Activities. Research Centers of Excellence. Research Partnerships. PD&R Studies ... in January 2024. Specifically, this report provides 2024 national, state, and CoC-level PIT and HIC estimates of homelessness, as well as estimates of chronically homeless persons, homeless veterans, and ...