Childhood obesity treatment: case studies
Resources Policy Dossiers Childhood Obesity Treatment Childhood obesity treatment: case studies
- Sugar-Sweetened Beverage Tax
- Digital Marketing
- School-based interventions
- Community-level interventions
- Pregnancy & Obesity
- Childhood Obesity Treatment
- Front-of-pack nutrition labelling
- Obesity & COVID-19
- Physical Activity
- Food Systems
- Weight Stigma
Family-Based Interventions in the Prevention and Management of Childhood Overweight and Obesity: An International Review of Best Practices, and a Review of current Irish Interventions
The aim of this review is "to identify current family-based practice internationally for the prevention and treatment of childhood overweight and obesity and to examine current Irish Programmes so that best practice recommendations can be drawn up."
Cost-effectiveness of intensive inpatient treatment for severely obese children and adolescents in the Netherlands; a randomized controlled trials (HELIOS)
This paper presents "the design of a randomized controlled trial comparing the cost-effectiveness of two itnensive one-year inpatient treatments to each other and to usual are for severely obese children and adolescents."
Family-based behavioural treatment of childhood obesity in a UK National Health Service setting: randomized controlled trial
The objective of this randomised controlled trial was "to examine the acceptability and effectiveness of 'family-based behavioural treatment' (FBBT) for childhood obesity in an ethnically and social diverse sample of families in a UK National Health Service (NHS) setting."
Reducing childhood obesity in Poland by effective policies
The purpose of this report was "to faciliate the development of an action plan and implementation of the strategy dimensions around childhood obesity by providing evidence-based policy options adapted to the national context." https://www.who.int/europe/publications/i/item/WHO-EURO-2017-2977-42735-59610
The Malaysian Childhood Obesity Treatment Trial (MASCOT)
The primary aim of the study is "to describe a behavioural family-centred, group-based treatment programme for childhood obesity in Malaysia - the MASCOT."
Process evaluation of an up-scaled community-based child obesity treatment program: NSW Go4Fun®
This paper "describes the up-scaling of Go4Fun in New South Wales and the characteristics of the population it has reached and retained since inception in 2009,including characteristics of children who completed and did not copmlete the programme."
Randomized Controlled Trial of the MEND Program: A Family-Based Community Intervention for Childhood Obesity
The objective of this study was to evaluate the effectiveness of the Mind, Exercise, Nutrition, Do it (MEND) Programme.
Assessing the short-term outcomes of a community-based intervention for overweight and obese children: the MEND 5-7 programme
The aim of this study was "to report outcomes from the UK service level delivery of MEND 5-7."
Effectiveness of a Multi-Component Intervention for Overweight and Obese Children (Nereu Program): A Randomized Controlled Trial
The objective of this study was "to evaluate the effectiveness of the Nereu Program in improving anthropometric parameters, physical activity and sedentary behaviours, and dietary intake."
Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity: a prospective five-year Swedish nationwide study (AMOS)
The objective of this study was "to report outcomes over 5 years in adolescents follow Roux-en-Y gastric bypass (RYGB) or conservative treatment in a Swedish nationwide prospective non-randomised controlled study, with an additional matched adult comparison group undergoing RYGB."
Mapping the health system response to childhood obesity in the WHO European Region. An overview and country perspectives
This project aimed "to assess the response of health care delivery systems in 19 countries in the WHO European Region to the childhood obesity epidemic."
An Integrated Clinic-Community Partnership for Child Obesity Treatment: A Randomized Pilot Trial
This study aims “to describe the implementation of an integrated clinic-community partnership for child obesity treatment and [...] to evaluate the effectiveness of integrated treatment on child BMI and health outcomes” in a lower-income area. Enrolled children were between 5 and 11 years of age, over the 95th percentile for BMI, and referred to clinic by their paediatrician.
Adapting Pediatric Obesity Treatment Delivery for Low-Income Families: A Public–Private Partnership
The aim of this study was to “evaluate the feasibility of delivering a paediatric weight management intervention adapted for low-income families.”
Challenges and results of a school-based intervention to manage excess weight among school children in Tunisia 2012-2014
This study intended to “demonstrate the feasibility and effectiveness of a school-based weight management program based on healthy lifestyle promotion for obese and overweight adolescents in Sousse, Tunisia.”
The Effect of a Multidisciplinary Lifestyle Intervention on Obesity Status, Body Composition, Physical Fitness, and Cardiometabolic Risk Markers in Children and Adolescents with Obesity
The aim of this study was to develop a “moderate-intensity multidisciplinary lifestyle intervention program” to treat obesity in the “real world” and evaluate its effectiveness through anthropometric measures.
The GReat-Child™ Trial: A Quasi-Experimental Intervention on Whole Grains with Healthy Balanced Diet to Manage Childhood Obesity in Kuala Lumpur, Malaysia
Scientists designed the GReat-Child™ trial to determine if increasing whole grain consumption could effectively impact health parameters in Malaysian children.
Impact of readiness to change behaviour on the effects of a multidisciplinary intervention in obese Brazilian children and adolescents
This study examined how the success of a multifaceted obesity treatment was related to a child’s willingness to alter their lifestyle using Stages of Readiness for Behavior Change (SRBC).
Sacbe, a Comprehensive Intervention to Decrease Body Mass Index in Children with Adiposity: A Pilot Study
The aim of this study was to “to achieve a higher percentage of success in lowering the BMI z-score in children with adiposity and their parents through a pilot program "Sacbe" based on HLS, sensitive to the sociocultural context previously explored and with the active participation of parents.”
A Novel Home-Based Intervention for Child and Adolescent Obesity: The Results of the Whānau Pakari Randomized Controlled Trial
The aim of this study was to “report 12‐month outcomes from a multidisciplinary child obesity intervention program, targeting high‐risk groups” in New Zealand.


Systematic reviews
Cost studies
Government guidelines & recommendations
Share this page.
Training & Events
SCOPE E-Learning
We offer the only internationally recognised course on obesity management. Read more here.
Global Obesity Observatory
We offer various statistics, maps and key data around the topic of obesity. You can find all that and more here.
Policy & Advocacy
Our Policy Priorities
We have developed five key areas of policy that are a priority to us. Want to know more? Check them out here!
- Our Members
- Member Benefits
- Membership Application Form
- Partnerships
- Global Obesity Forum
- Patient Portal
- Finance Committee
- Annual Report and Financials
- Prevalence of Obesity
- Causes of Obesity
- Obesity Classification
- Prevention of Obesity
- Obesity as a disease
- Commercial determinants of obesity
- Childhood Obesity
- Obesity in Universal Health Coverage
- The ROOTS of Obesity
- Working with the UN
- World Obesity Day
- Healthy Venues
- Reinventing the Food System: A Report
- The Spotlight Project
- SCOPE Examination
- Guide to SCOPE Certification
- SCOPE Fellows
- Leadership Programme
- Accreditation
- SCOPE Schools
- SCOPE Pricing
- SCOPE Sessions
- SCOPE Accredited Events
- Event Archive
- International Congress on Obesity
Sign up for notifications
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Childhood Obesity Incidence in the United States: A Systematic Review
Patricia c cheung , mph, solveig a cunningham , phd, km venkat naryan , md, michael r kramer , phd.
- Author information
- Copyright and License information
Address correspondence to:, Patricia C. Cheung, MPH , Department of Epidemiology , Rollins School of Public Health , 1518 Clifton Road , Atlanta, GA 30322 E-mail: [email protected]
Corresponding author.
Background: This systematic review synthesizes the literature on incidence of obesity during childhood.
Methods: We searched PubMed, Excerpta Medica database (EMBASE), and Cumulative Index to Nursing and Allied Health Literature (CINAHL), and used the Web of Science tool in June 2015. Studies were included if they were published in English, presented results from primary or secondary analyses, used data about children in the US, provided obesity incidence data on children 0 to 18 years born after 1970, and did not pertain to clinically defined populations (disease, medication use, etc.). Author(s), study year, study design, location, sample size, age, and obesity incidence estimates were abstracted.
Results: Nineteen studies were included, three of which used nationally representative data. The median study-specific annual obesity incidences among studies using U.S. Centers for Disease Control and Prevention (CDC) growth charts were 4.0%, 3.2%, and 1.8% for preschool (2.0–4.9 years), school aged (5.0–12.9 years), and adolescence (13.0–18.0 years), respectively. This pattern of declining obesity incidence with age was consistent between and within studies.
Conclusions: Studies of childhood obesity in the US indicate declining incidence with age. Childhood obesity prevention efforts should be targeted to ages before obesity onset. Longitudinal data and consistent obesity definitions that correlate with long-term morbidity are needed to better characterize the life history of obesity.
Introduction
Childhood obesity is a major public health concern, as the prevalence of obesity worldwide is believed to be increasing. 1 In the United States, obesity prevalence among children ages 6–11 years more than tripled from 4.2%–15.3% between 1963–1965 and 1999–2000. 1 Although recent studies have reported decreased obesity prevalence among younger children, in 2011–2012, 16.9% of children in the United States were classified as obese, with prevalence being highest at ages 12–19 and lowest at ages 2–5 years. 2 In the past three decades, increases in obesity prevalence have been observed among children of all ages, 2 , 3 though differences in obesity prevalence have been documented by age, 2 race and ethnicity, 1 gender, 2 and geographic region. 4 Obesity in childhood has been associated with subsequent obesity in adulthood, other chronic diseases, and high medical costs, 5–9 so understanding the emergence of obesity in childhood may offer opportunities to improve health at all ages.
While the prevalence of obesity among children in the United States has been well documented, 2 , 3 less is known about obesity incidence. Prevalence of obesity for a given age group is a composite of preceding and concurrent incidence and remission for children. Detailing age-specific obesity incidence is important for elucidating peak periods of obesity onset to identify and maximize intervention opportunities and minimize healthcare costs. Tracking of childhood obesity into adulthood calls for intervention efforts to prevent obesity that are timed to precede onset, and age-specific incidence estimates contribute to this perspective. 13 , 14 Estimating incidence for racial, ethnic, and socioeconomic groups may be useful for understanding the disparities in obesity that have been observed across age groups. 6 , 10–12 We present results from a systematic review of studies that have estimated the incidence of obesity among children in the United States.
The procedures used in this review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement. We conducted systematic searches of peer-reviewed journals in June 2015 using PubMed, Excerpta Medica database (EMBASE), and Cumulative Index to Nursing and Allied Health Literature (CINAHL). Key words used for all searches were “obesity” and “incidence.” Incidence was searched as a medical subject heading (MeSH) term in PubMed. “Child: birth-18 years” was used as a search filter. Searches were not restricted by publication date. The studies identified through these search criteria were reviewed independently by two authors according to the following criteria: (1) published in English; (2) presented findings from analysis of primary or secondary data; (3) presented data from the United States; (4) provided estimates of obesity incidence among children ages 0–18 years or provided data from which incidence could be calculated; and (5) used data from individuals born after 1970. Studies of clinically defined populations, specifically those with a particular disease or medication regimen, were excluded, but control arms of intervention trials were included. Hand searches of the references of these articles were performed and the Web of Science Cited Reference Search tool, which identifies other articles referencing a specific study, was used for key articles. This review protocol was not registered prior to its outset.
A data extraction spreadsheet was used to assess whether articles met inclusion criteria and to compare studies. For each study, the first author collected the following information: author(s) and year of publication; years of data collection; study design (cohort versus randomized trial; representativeness); location in the United States; sample size; age at baseline and follow-up; years of birth; and obesity incidence estimates. If the study included data for individuals both younger and older than 18, only data for children less than 18 years were retained if age categorization permitted such subsetting. If subsetting was not possible, the study was excluded. Among intervention studies, only data on the control or nonintervention group were abstracted. One study did not estimate incidence but provided sufficient data for us to perform the calculation (number of children at risk for obesity at baseline and number of children obese at a later point). We reported cumulative incidence (incidence proportion) from each study, defined as the number of newly obese children during study follow-up divided by the number of nonobese children potentially at risk for obesity at baseline. Because studies varied in length of follow-up, we estimated annualized incidence proportions using cumulative incidence estimates from each study divided by years of follow-up.
Studies included convenience and representative samples, used differing study designs (e.g., observational cohort or randomized controlled trial), measures of adiposity (body mass index [BMI] or skin fold thickness), and definitions of obesity (cutpoints defined by the Centers for Disease Control and Prevention [CDC] International Obesity Task Force [IOTF], etc.). Such heterogeneity made formal statistical meta-analysis impractical. Similarly, this variation in study design and obesity measurement made it difficult to use uniform criteria or a single measurement to systematically assess bias. Potential biases at study and outcome levels are discussed in the limitations section.
The majority (15 of 19) of studies measured adiposity with BMI and defined obesity according to CDC cutpoints for BMI-for-age-and-sex at or above 95th percentile, or used CDC weight-for-length charts for infants. Due to the small number of studies within each age group, studies using the current CDC cutpoints or weight-for-length charts for infants were summarized by the median study-specific annualized incidence for each of the following age groups: infancy (0–1.9 years), preschool (2.0–4.9 years), school aged (5.0–12.9 years), and adolescence (13.0–18.0 years). These age groups were selected because they capture major developmental stages. Studies on children whose ages spanned two groups were included in median calculations of both age groups. To visualize age-specific trends in incident obesity, we plotted the annualized cumulative incidence of obesity against the age range of study follow-up. This was summarized with a weighted simple linear regression with weights for each study, defined as the inverse of the variance of the study-specific incidence estimate. Study-specific baseline risk varied by known demographic factors, so studies were categorized into two groups: (1) predominantly high-risk population (> 50% racial/ethnic minorities or a single high-risk socioeconomic community) and (2) not predominantly high-risk population (all other studies).
To consider temporal changes in environments that may have been linked with obesity patterns over the decades being studied, a sensitivity analysis was performed by decade of birth. In the 2000s, a shift in the obesity category definition occurred, so we examined whether the change influenced our findings. A second sensitivity analysis examined only studies using the CDC obesity definition published during and after 2007. 15 , 16
Literature Identification and Selection
We identified 2135 articles: 1068 in PubMed, 698 in EMBASE, and 369 in CINAHL ( Figure 1 ). After discarding duplicate articles, titles and abstracts were screened for inclusion criteria, resulting in 126 articles. After review and application of exclusion criteria, 19 articles were retained ( Table 1 ).
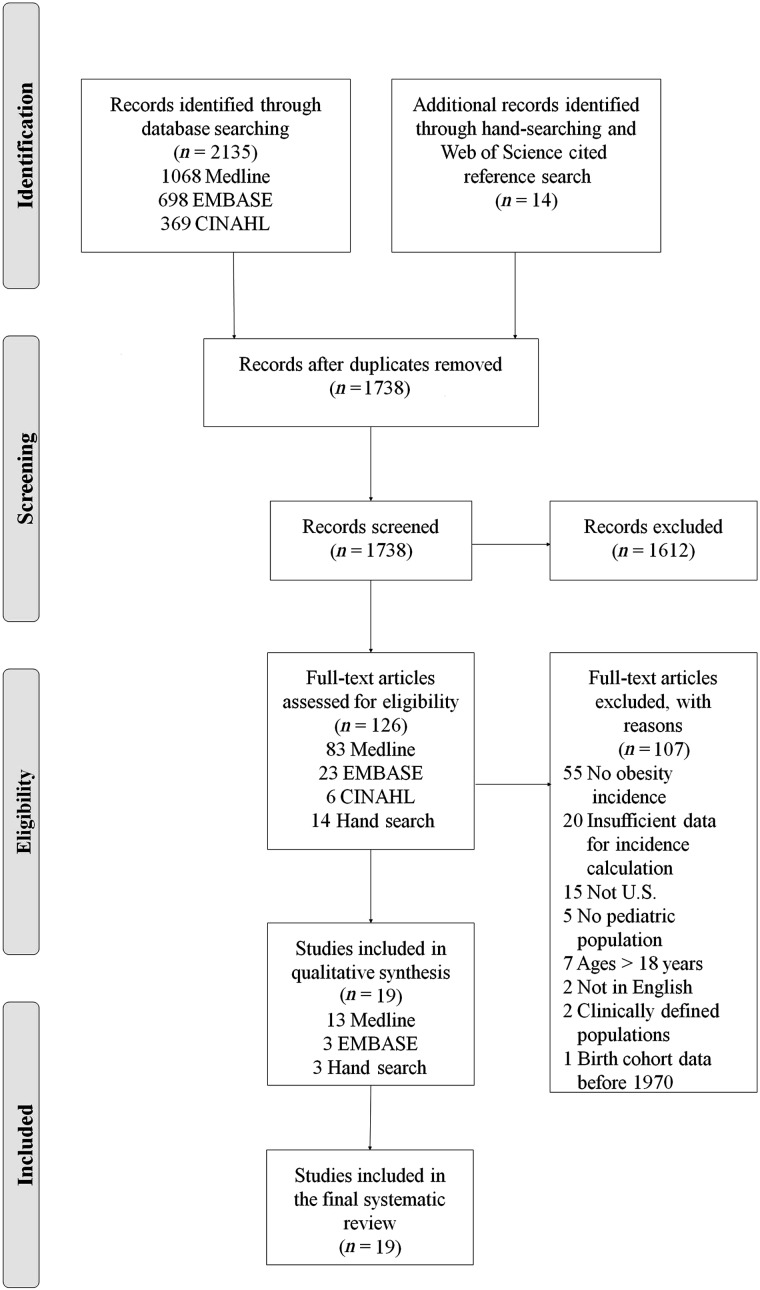
Preferred reporting items for systematic reviews and meta-analyses flow diagram describing article acquisition of 19 studies involving childhood obesity incidence in the United States. Articles ( n = 2135) were identified through database searches, and 14 articles were identified through hand searching. Among these studies, 1612 articles were excluded based on title and abstract review. After the remaining 126 articles were reviewed, 19 articles met the inclusion criteria and were included in the analysis.
Summary of 19 Studies Reporting Child Obesity Incidence in the United States: Predominantly High Risk Denotes Studies Conducted among Socioeconomically Disadvantaged or >50% Racial/Ethnic Minority Groups. (Not predominantly high risk denotes all other studies.)
Age was reported differently across studies. Available information was reported in this table.
Cohort study.
Nationally representative study population.
Randomized study or quasi-experimental study.
Based on sex- and age-specific reference values of the IOTF.
Based on 2000 CDC sex- and age-specific growth charts where obese was classified as BMI ≥95th percentile.
Based on 2000 CDC age- and sex-specific growth charts as BMI ≥95th percentile, which was previously the definition of overweight.
Based on NHANES I references, where obesity is defined as BMI and triceps skinfolds ≥85%.
Study only included girls only.
Based on 2000 CDC sex-specific weight-for-length charts ≥95th percentile.
Denominator for calculating incidence did not include overweight children.
Based on combined data of NHANES I and II, where obese was classified as BMI ≥95th percentile.
IOTF, International Obesity Task Force; CDC, Centers for Disease Control and Prevention; NHANES, National Health and Nutrition Examination Survey; SD, standard deviation; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.

Literature Overview
Eight articles were published during and after 2010, and only two studies were published before 2000. Only three used nationally representative data. 17 , 18 , 30 Studies reporting incidence included one study among children under 2 years of age, 29 two among children between 2.0–4.9 years, 24 , 29 seven among children 5.0–12.9 years, 6 , 10 , 11 , 18 , 23 , 28 , 31 and two among adolescents 13.0–18.0 years. 6 , 21 Many studies spanned age groups, including infancy through the preschool ages, 22 , 29 preschool through school age, 17 , 25 , 26 , 27 , 30 and school age through adolescence. 6 , 10 , 18–20 , 26 , 32
Many studies were based on secondary analysis of datasets, including the Pediatric Nutrition Surveillance System (PedNSS; n = 3); National Longitudinal Survey of Youth (NLSY; n = 2), Cambridge Public School Health Surveillance System ( n = 2); or others ( n = 3). Nine studies analyzed primary data, including five intervention studies randomized at the school level and providing control arm data. 20 , 23 , 28 , 31 , 32 Of the three nationally representative studies, two used the NLSY- Child Cohort data. One of these three representative studies included follow-up data from 1980–1988, finding an annual incidence of 1.3% for children 4–10 years old. 30 Another study included follow-up from 1980–1998, reporting annual incidence of 1.7% for children ages 4.5–10.5 years. 17 The most recent study used data from the Early Childhood Longitudinal Study, Kindergarten Class of 1998/9, which followed a cohort of children born in 1993 from an average age of 5.6–14.1 years. 18 Obesity incidence was estimated at 11.9% over the entire age range and annualized obesity incidences were estimated at 5.4% at mean ages of 5.6–6.1 years, 2.7% at 6.1–7.1 years, 3.0% at 7.1–9.1 years, 3.1% at 9.1–11.1 years, and 1.7% at 11.1–14.1 years. Sample sizes for studies included in this review ranged between 109 and 380,518 children. 23 , 29 Follow-up was on average 2.0 years (range: 0.5–9.0 years).
Height and weight were measured by medical personnel (physicians, nurses, nutritionists, dieticians) or trained researchers using stadiometers or tape measures and scales in all but two nationally representative studies (which used parent-reported data for a subset of participants. 17 , 30 ) Fifteen studies used the CDC definition of obesity (BMI-for-age-and-sex ≥95th percentile for children 2 years or older) or CDC gender-specific weight-for-length charts (≥ 95th percentile for children less than 2 years). One used a combination of BMI and triceps skinfolds measurements (both ≥95th percentile); 20 two used IOTF cutpoints; 11 , 21 and one used BMI >95th percentile derived from the first and second National Health and Nutrition Examination Surveys (NHANES). 30
Age-Specific Obesity Incidence
Across studies measuring adiposity with CDC BMI-for-age-and-sex or weight-for-length percentile definitions of obesity, the median annualized obesity incidence was 4.0% for infants 0–1.9 years (range: 2.1%–8.2%), 4.0% for preschool-aged children 2.0–4.9 years (range: 1.1%–6.7%), 3.2% for school-aged children 5.0–12.9 years (range: 1.1%–6.8%), and 1.8% for adolescents 13.0–18.0 years (range: 0.4%–4.4%). As an approximation of the trend, the weighted regression demonstrated a steady decline in incidence with age ( Figure 2 ).
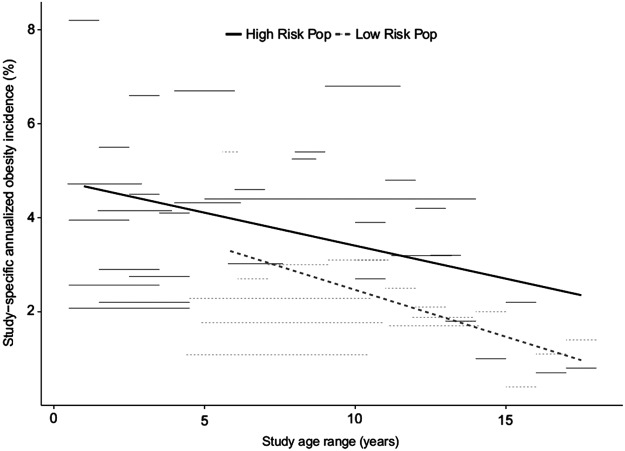
Annual obesity incidence by age across 19 studies in the United States. High-risk population denotes studies conducted among socioeconomically disadvantaged or >50% racial/ethnic minority groups. Low-risk population denotes all other studies. Trendlines are weighted by the inverse of the variance of each study-specific incidence estimate.
Five studies, including one nationally representative cohort, reported decreasing incidence with increasing age. 6 , 10 , 18 , 22 , 29 One study, using the PedNSS, a study of low-income children in 39 states and the District of Columbia, reported annual obesity incidence of 4.7% at ages 0–1 years and 4.1% at ages 1–2 years among children born in 2006–2008. 22 Another study, also using the PedNSS but among children born 1985–1990, reported annual incidence at baseline of 8.2% at ages 0–1 years, 5.5% at 1–2 years, 4.5% at 2–3 years, and 4.1% at 3–4 years. 29 A study using a nationally representative cohort reported an annual incidence ranging from 5.4% within kindergarten (5.6–6.1 years) to 1.7% between fifth and eighth grades (11.1–14.1 years. 18 ) A study of the Cambridge Public School Health Surveillance System in Cambridge, Massachusetts, reported that annual incidence peaked at 5.4% at 7–9 years at baseline, but declined between ages 9–11 years. 10 Finally, a study using data from the National Heart, Lung, and Blood Institute Growth and Health Study, a sample of urban Black and white girls, reported the annual incidence of obesity to be 3.1% at ages 10–11 years and 1.4% at 17–18 years among white girls; 6 for Black girls, incidences were 4.8% between 11–12 years and 0.7% between 16–17 years, but the incidence trends with age were less clear for this study. 6
Child Obesity Incidence by Demographics and Baseline Weight
Children from socioeconomically disadvantaged families and some racial and ethnic minorities experienced higher median obesity incidence than whites. Studies conducted among socioeconomically disadvantaged or >50% racial/ethnic minority groups and using CDC percentile definitions of obesity reported obesity incidences of 4.0% at ages 0–1.9 years (range: 2.1%–8.2%), 4.1% at 2.0–4.9 years (range: 2.1–6.7%), 4.4% at 5.0–12.9 years (range: 2.7–6.8%), and 2.2% at 13.0–18.0 years (range: 0.7%–4.4%). Six studies analyzed obesity incidence by race and ethnicity. Four of these studies, including two using nationally representative data, 18 , 30 showed higher obesity incidence rates among Blacks and Hispanics compared with Whites. 10 , 18 , 21 , 30 One study using data on girls in the Southwest reported annual incidences of 4.5% among Black, 2.0% among Hispanic, and 0.7% among white girls at ages 13–19 years. 21 Among low-income children across 39 states and the District of Columbia, incidences at 0–1.9 years were 6.3% among American Indians/Alaskan Natives, 5.5% among Hispanics, 3.7% among Asian Pacific Islanders, 3.5% among Blacks, and 3.9% among whites. 22 Among urban Black and white girls born in 1976–1977, incidence was higher among Black girls at some but not all ages. 6
Six studies, including one nationally representative cohort, examined incidence rates stratified by children's weight at baseline weight (e.g., normal weight, overweight, etc.). All but one study reported that children who became obese during the study period were more likely to have been overweight at baseline; 10 , 18 , 21 , 22 , 27 the other study showed a “regression to the mean” effect, where normal-weight children tended to gain weight, and overweight and obese children generally lost weight over time; but this study population had a high prevalence of overweight (44.3%) and obesity (22.0%) at a baseline. 11
Seven studies reported gender-specific obesity incidence. Three of these, including a nationally representative study, reported higher obesity incidences among boys compared with girls, 20 , 22 , 30 with a maximum difference in annual incidence of 0.9% (5.5% and 4.6% for boys and girls, respectively) at ages 11.7–13.5 years. 20 Two studies reported higher annual obesity incidence among girls: 3.2% for girls versus 0.5% for boys 11 and 5.0% for girls versus 4.0% for boys, 26 respectively. Two studies, including a nationally representative study, reported higher incidences for boys at some ages but not others. 10 , 18
One study examined differences in incidence across birth cohorts, estimating obesity incidence at ages 4.6–10.6 years for children born in 1980–1986, 1987–1992, and 1993–1998 in the nationally representative NLSY Youth Cohort. Annual incidence estimates were 1.1% for children born in 1980–1986, 2.3% for children born in 1987–1992, and 1.8% for children born in 1993–1998. 17
Sensitivity analyses showed that the pattern of decreasing childhood obesity incidence with age was consistent across birth cohorts ( Figure 3 ) for children born in the 1970s, 1980s, and 1990s. The same trend of decreasing childhood obesity incidence with increasing age was observed when restricting to studies published during and after 2007 (see online supplementary Figure S1 at www.liebertpub.com/jpm and at www.liebertonline.com ) after most researchers had adopted proposed terminology changes occurring in the 2000s. 15 , 16
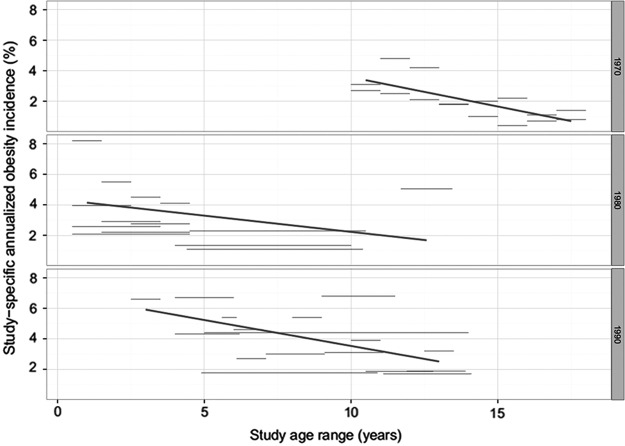
Annual obesity incidence by age stratified by birth cohort decade (1970s, 1980s, and 1990s) across studies in the United States. Trendlines are weighted by the inverse of the variance of each study-specific incidence estimate.
This systematic review synthesized current knowledge about the incidence of obesity from early childhood through adolescence in the United States. The main finding is that across studies, annual incidence declined with age: the median incidence proportion was 4.0% at ages 0–1.9 years, 4.0% at 2.0–4.9 years, 3.2% at 5.0–12.9 years, and 1.8% at 13.0–18.0 years.
These patterns are also consistent with some studies of obesity incidence among adults in the United States. A study using 2009 Behavioral Risk Factor Surveillance System (BRFSS) data used self-reported height and weight at the time of the study and one year previously to calculate obesity incidence among adults ≥18 years in the United States, and found obesity incidence decreased with age: 6.4% at ages 18–29 years, 4.8% at 30–49 years, 3.3% at 50–69 years, and 1.5% at ages 70 years and over. 33 These patterns were robust to adjusting for age, sex, race/ethnicity, education, region, physical activity, fruit and vegetable consumption, smoking, alcohol use, and baseline BMI. However, a study using the nationally representative National Longitudinal Study of Adolescent Health (Add Health Waves II and III) estimated annual incidences at 1.9% at ages 13–15 years, 2.4% at 16–17 years, and 2.4% at 18–20 years. 34
The declining incidence with age could suggest exhaustion of the pool of children susceptible to incident obesity, or may reflect aspects of growth dynamics associated with development, such as regression from obese to nonobese states, adiposity rebound, and pubertal changes in body composition. Four studies reported obesity remission rates in addition to incidence. Among obese infants (0–23 months), 63.5% were not obese at follow up 24–35 months later. 22 One study reported annual remission rates ranging from 13.3%–20.3% for children ages 5–14 years. 10 A third study reported annual remission rates between 8.0% and 24.1% among adolescents. 21 The fourth study indirectly reported annual remission for infants (0–1 year) of 64.4% and for ages 3–4 years at 37.5%. 29 Relating the observed patterns in age-specific obesity incidence with what is known about patterns in obesity prevalence requires further understanding of the timing and reasons for obesity remission and normal growth dynamics.
The downward trend of obesity incidence with age observed in this study is consistent with some studies from outside the United States. For example, a large prospective cohort in southwest England in 2011 reported annual incidences of 1.2% at 3–11 years and 0.4% at 11–15 years. 35 Other studies from outside the United States have shown different patterns. In a 2012 study in northern Germany, annual obesity incidence was 0.6% at mean ages of 2–6 years and 0.7% at mean ages of 6–10 years. 36
Incidence patterns may differ by race and ethnicity, with four of the six studies examining incidence by race reporting that Black and Hispanic children experienced higher age-specific incidence rates than white children. 10 , 18 , 21 , 30 Higher incidence and lower remission rates among Blacks and Hispanics 10 , 21 may partially explain the higher obesity prevalence observed among these children. 10 , 18
Limitations
There were several limitations to this review. Many studies used convenience data or data that were not initially designed with the primary intention of studying obesity incidence. Consequently, study designs, measurements of obesity, populations, cohorts, and locations of studies were not optimal and differed widely. Only three studies used nationally representative data. 17 , 18 , 30 Among the studies drawing on data from intervention programs, 20 , 23 , 28 , 31 , 32 many focused on specific populations, such as schools in high-risk areas 28 , 31 , 32 or Native American reservations, 23 limiting the generalizability of the results. The heterogeneity in population was a challenge for literature synthesis, making straightforward comparisons between studies difficult.
Because BMI can easily be calculated using self-reported or directly measured height and weight, BMI-for-age-and-sex and weight-for-length percentile growth charts are a common measure included in large-scale studies. While not an ideal measure, BMI is an acceptable indicator of adiposity. 37 However, the potential of BMI categories to predict future health risks remains unclear. 38 , 39
Most studies involving children older than 2 years used the CDC BMI percentile cutoffs for overweight and obesity, but other studies used IOTF cutoffs or other definitions. The use of different definitions across studies impedes comparison. IOTF cutoff points produce lower estimates of obesity prevalence and higher estimates of obesity incidence in comparison to CDC cutoff points. 34 , 40 , 41 It will be important to determine which cutoffs are best suited for identifying future health risks. World Health Organization (WHO) growth standards have been recommended for monitoring weight up to age 2 years, but there is no consensus obesity measure for children younger than 2 years. 42 Two studies included in this review used CDC weight-for-length ≥95th percentile to define obesity in children under age 2 years. 22 , 29 WHO and CDC weight-for-length growth charts are not comparable. 43 Identifying a measure of unhealthy weight for children under age 2 years will be useful, since studies have shown that obesity may originate early in life.
Conclusions
The literature on incidence of childhood obesity is relatively sparse and is heterogeneous in populations and study design. The studies to date have indicated that obesity incidence is highest at the youngest ages and declines with age through adolescence. They have also shown that incidence proportions may differ by gender, race, ethnicity, and socioeconomic status. The patterns suggest the need to focus obesity prevention early in life. However, limitations in existing data sources suggest that future surveillance of population-based patterns of obesity incidence will benefit from consistent use of measures with predictive capacity for future health outcomes, carried out in representative populations periodically assembled in order to understand incidence of childhood obesity, risk factors, and changes in these measures over time. The information from such systematized and representative surveillance could make it possible to (1) investigate etiologic explanations for incidence and remission of obesity, (2) identify windows of opportunity for effective intervention, and (3) evaluate the impact of ongoing interventions.
Supplementary Material
Acknowledgments.
This project was supported in part by grant numbers R03HD060602 (SAC, KMVN) and K01HD074726 (MRK) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the NIH.
Author Disclosure Statement
No competing financial interests exist.
- 1. Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation 2012;126:1770–1779 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Ogden CL, Carroll MD, Kit BK, et al. . Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Ogden CL, Flegal KM, Carroll MD, et al. . Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 2002;288:1728–1732 [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med 2010;164:598–607 [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Muller MJ, Danielzik S, Pust S. School- and family-based interventions to prevent overweight in children. Proc Nutr Soc 2005;64:249–254 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Thompson DR, Obarzanek E, Franko DL, et al. . Childhood overweight and cardiovascular disease risk factors: The National Heart, Lung, and Blood Institute growth and health data. J Pediatr 2007;150:18–25 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Murtagh J, Dixey R, Rudolf M. A qualitative investigation into the levers and barriers to weight loss in children: Opinions of obese children. Arch Dis Child 2006;91:920–923 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Storch EA, Milsom VA, DeBraganza N, et al. . Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol 2007;32:80–89 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: A consideration of shared risk factors. Health Educ Res 2006;21:770–782 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Kim J, Must A, Fitzmaurice GM, et al. . Incidence and remission rates of overweight among children aged 5 to 13 years in a district-wide school surveillance system. Am J Public Health 2005;95:1588–1594 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Williamson DA, Han H, Johnson WD, et al. . Longitudinal study of body weight changes in children: Who is gaining and who is losing weight. Obes 2011;19:66–670 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Wright CM, Emmett PM, Ness AR, et al. . Tracking of obesity and body fatness through mid-childhood. Arch Dis Child 2010;95:612–617 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Oude Luttikhuis H, Baur L, Jansen H, et al. . Interventions for treating obesity in children. Cochrane Database Syst Rev 2009:CD001872. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Singh AS, Mulder C, Twisk JW, et al. . Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev 2008;9:474–488 [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Institute of Medicine Committee on Prevention of Obesity in Children and Youth. Preventing Childhood Obesity: Health in the Balance. Washington, DC: National Academies Press, 2005 [ PubMed ] [ Google Scholar ]
- 16. Krebs NF, Himes JH, Jacobson D, et al. . Assessment of child and adolescent overweight and obesity. Pediatrics 2007;120;S193–S228 [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA 2010;303:623–630 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Cunningham S, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med 2014;370:401–409 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Stevens J, Murray DM, Baggett CD, et al. . Objectively assessed associations between physical activity and body composition in middle-school girls: The Trial of Activity for Adolescent Girls. Am J Epidemiol 2007;166:1298–1305 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Gortmaker SL, Peterson K, Wiecha J, et al. . Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409–418 [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Huh D, Stice E, Shaw H, et al. . Female overweight and obesity in adolescence: Developmental trends and ethnic differences in prevalence, incidence, and remission. J Youth Adolesc 2012;41:76–85 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Pan L, May AL, Wethington H, et al. . Incidence of obesity among young US children living in low-income families, 2008–2011. Pediatrics 2013;132:1006–1013 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Story M, Hannan PJ, Fulkerson JA, et al. . Bright start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obes 2012;20:2241–2249 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Welsh JA, Cogswell ME, Rogers S, et al. . Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics 2005;115:e223–e229 [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Lim S, Zoellner JM, Lee JM, et al. . Obesity and sugar-sweetened beverages in African-American preschool children: A longitudinal study. Obesity (Silver Spring) 2009;17: 1262–1268 [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Kim J, Must A, Fitzmaurice GM, et al. . Relationship of physical fitness to prevalence and incidence of overweight among schoolchildren. Obes Res 2005;13:1246–1254 [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Robbins JM, Khan KS, Lisi LM, et al. . Overweight among young children in the Philadelphia health care centers: Incidence and prevalence. Arch Pediatr Adolesc Med 2007;161:17–20 [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Rappaport EB, Daskalakis C, Sendecki JA. Using routinely collected growth data to assess a school-based obesity prevention strategy. Int J Obes (Lond) 2013;37:79–85 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Mei Z, Grummer-Strawn LM, Scanlon KS. Does overweight in infancy persist through the preschool years? An analysis of CDC Pediatric Nutrition Surveillance System data. Soz Praventivmed 2003;48:161–167 [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics 1999;103:e85. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Klish WJ, Karavias KE, White KS, et al. . Multicomponent school-initiated obesity intervention in a high-risk, Hispanic elementary school. J Pediatr Gastroenterol Nutr 2012;54:113–116 [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Foster GD, Sherman S, Borradaile KE, et al. . A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008;121:e794–e802 [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Pan L, Freedman DS, Gillespie C, et al. . Incidences of obesity and extreme obesity among US adults: Findings from the 2009 Behavioral Risk Factor Surveillance System. Popul Health Metr 2011;9:56. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Gordon-Larson P, Adair LS, Nelson MC, et al. . Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr 2004;80:569–575 [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Hughes AR, Sherriff A, Lawlor DA, et al. . Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev Med 2011;52:300–304 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. von Kries R, Beyerlein A, Muller MJ, et al. . Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int J Obes (Lond) 2012;36:505–510 [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Gallagher D, Visser M, Sepúlveda D, et al. . How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996;143:228–239 [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Moyer VA, Klein JD, Ockene JK, et al. . Screening for overweight in children and adolescents: Where is the evidence? A commentary by the Childhood Obesity Working Group of the US Preventive Services Task Force. Pediatrics 2005;116:235–238 [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Whitlock EP, Williams SB, Gold R, et al. . Screening and interventions for childhood overweight: A summary of evidence for the US Preventive Services Task Force. Pediatrics 2005;116:e125–e144 [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Vidal E, Carlin E, Driul D, et al. . A comparison study of the prevalence of overweight and obese Italian preschool children using different reference standards. Eur J Pediatr 2006;165:696–700 [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Twells LK, Newhook LA. Obesity prevalence estimates in a Canadian regional population of preschool children using variant growth references. BMC Pediatr 2011;11:21. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Grummer-Strawn LM, Reinold C, Krebs NF, et al. . Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR Recomm Rep 2010;59(RR-9):1–15 [ PubMed ] [ Google Scholar ]
- 43. Nash A, Secker D, Corey M, et al. . Field testing of the 2006 World Health Organization growth charts from birth to 2 years: Assessment of hospital undernutrition and overnutrition rates and the usefulness of BMI. J Parenter Enteral Nutr 2008;32:145–153 [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (337.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES